Abstract
Objective
To evaluate the feasibility, efficiency, and safety of microwave ablation (MWA) for T1N0M0 multifocal (≤ 3) papillary thyroid carcinoma (PTC).
Methods
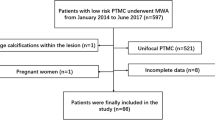
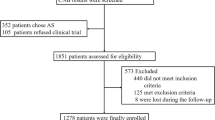
This was a retrospective study, and patients who underwent MWA for multifocal (≤ 3) PTC were reviewed between October 2016 and December 2020. After ablation, the changes in tumor size and volume, as well as the rate of technical success, tumor disappearance, disease progression, and complications were assessed.
Results
There were a total of 57 cases enrolled in the present study, which included 18 males and 39 females. The mean age was 44 ± 11 years (22–66 years); the mean follow-up time was 18 ± 11 months (6–48 months). Complete ablation was achieved in all enrolled cases. Therefore, the technical success rate was 100%. Due to expanding ablation, the MD and volume of the ablation zone, as well as the VRR, increased at the 1st and 3rd months after ablation and decreased at 12 and 18 months after ablation (p < 0.05 for all). The total complete tumor disappearance rate was 43.9% (25/57), including 54% (24/44) in the T1a subgroup vs. 7.7% (1/13) in the T1b subgroup (p = 0.003). The total disease progression rate was 7% (4/57), including 9.1% (4/44) in the T1a subgroup vs. 0% (0/13) in the T1b subgroup (p = 0.142). The overall complication rate was 5.3% (3/57), including 6.8% (4/44) in the T1a subgroup vs. 0% (0/13) in the T1b subgroup (p = 0.206).
Conclusion
This preliminary study indicates that MWA is a safe and effective treatment for T1N0M0 multifocal (≤ 3) PTC.
Key points
• MWA is a promising alternative method for T1N0M0 multifocal (≤ 3) PTC.


Similar content being viewed by others
Abbreviations
- AS:
-
Active surveillance
- CEUS:
-
Contrast-enhanced ultrasound
- CLT:
-
Chronic lymphocytic thyroiditis
- FNA:
-
Fine-needle aspiration
- HCC:
-
Hepatocellular carcinoma
- LNM:
-
Lymph node metastasis
- MD:
-
Maximum diameter
- MWA:
-
Microwave ablation
- PTC:
-
Papillary thyroid carcinoma
- RCC:
-
Renal cell carcinoma
- RFA:
-
Radiofrequency ablation
- RLN:
-
Recurrent laryngeal nerve
- SD:
-
Standard deviation
- US:
-
Ultrasound
- VRR:
-
Volume reduction ratio
References
Londero SC, Krogdahl A, Bastholt L et al (2013) Papillary thyroid carcinoma in Denmark 1996-2008: an investigation of changes in incidence. Cancer Epidemiol 37:e1–e6
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer Statistics, 2021. CA Cancer J Clin 71:7–33
Hawk WA, Hazard JB (1976) The many appearances of papillary carcinoma of the thyroid. Cleve Clin Q 43:207–215
Russell WO, Ibanez ML, Clark RL, White EC (1963) Thyroid carcinoma. classification, intraglandular dissemination, and clinicopathological study based upon whole organ sections of 80 glands. Cancer 16:1425–1460
Carcangiu ML, Zampi G, Pupi A et al (1985) Papillary carcinoma of the thyroid. A clinicopathologic study of 241 cases treated at the University of Florence, Italy. Cancer 55:805–828
Iida F, Yonekura M, Miyakawa M (1969) Study of intraglandular dissemination of thyroid cancer. Cancer 24:764–771
Tscholl-Ducommun J, Hedinger CE (1982) Papillary thyroid carcinomas. Morphology and prognosis. Virchows Arch A Pathol Anat Histol 396:19–39
Haddad RI, Nasr C, Bischoff L et al (2018) NCCN guidelines insights: thyroid carcinoma, Version 2.2018. J Natl Compr Cancer Netw 16:1429–1440
Kang TW, Rhim H (2015) Recent advances in tumor ablation for hepatocellular carcinoma. Liver Cancer 4:176–187
Filippiadis DK, Gkizas C, Chrysofos M et al (2018) Percutaneous microwave ablation of renal cell carcinoma using a high power microwave system: focus upon safety and efficacy. Int J Hyperthermia 34:1077–1081
de Baere T, Tselikas L, Catena V et al (2016) Percutaneous thermal ablation of primary lung cancer. Diagn Interv Imaging 97:1019–1024
Crocetti L, Scalise P, Bozzi E et al (2021) Microwave ablation of very-early- and early-stage HCC: efficacy evaluation by correlation with histology after liver transplantation. Cancers (Basel) 13:3420. https://doi.org/10.3390/cancers13143420
Cao X-J, Wang S-R, Che Y et al (2021) Efficacy and safety of thermal ablation for treatment of solitary T1N0M0 papillary thyroid carcinoma: a multicenter retrospective study. Radiology 300:209–216
Cao X-J, Liu J, Zhu Y-L et al (2021) Efficacy and safety of thermal ablation for solitary T1bN0M0 papillary thyroid carcinoma: a multicenter study. J Clin Endocrinol Metab 106:e573–e581
Wu J, Zhao Z-L, Cao X-J et al (2021) A feasibility study of microwave ablation for papillary thyroid cancer close to the thyroid capsule. Int J Hyperthermia 38:1217–1224
Cheng Z, Che Y, Yu S et al (2017) US-guided percutaneous radiofrequency versus microwave ablation for benign thyroid nodules: a prospective multicenter study. Sci Rep 7:9554. https://doi.org/10.1038/s41598-017-09930-7
Yan L, Zhang M, Song Q et al (2022) Clinical outcomes of radiofrequency ablation for multifocal papillary thyroid microcarcinoma versus unifocal papillary thyroid microcarcinoma: a propensity-matched cohort study. Eur Radiol 32:1216–1226
Gimm O, Brauckhoff M, Thanh PN et al (2002) An update on thyroid surgery. Eur J Nucl Med Mol Imaging 29(Suppl 2):S447–S452
Ghai S, O’Brien C, Goldstein DP et al (2021) Ultrasound in active surveillance for low-risk papillary thyroid cancer: imaging considerations in case selection and disease surveillance. Insights Imaging 12:130. https://doi.org/10.1186/s13244-021-01072-9
Jovanovic L, Delahunt B, McIver B et al (2008) Most multifocal papillary thyroid carcinomas acquire genetic and morphotype diversity through subclonal evolution following the intra-glandular spread of the initial neoplastic clone. J Pathol 215:145–154
Kim H, Kwon H, Moon B-I (2021) Association of multifocality with prognosis of papillary thyroid carcinoma: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 147:847–854
Xiao J, Zhang Y, Zhang M et al (2021) Ultrasonography-guided radiofrequency ablation vs. surgery for the treatment of solitary T1bN0M0 papillary thyroid carcinoma: a comparative study. Clin Endocrinol (Oxf) 94:684–691
Tamai H, Okamura J (2021) New next-generation microwave thermosphere ablation for small hepatocellular carcinoma. Clin Mol Hepatol 27:564–574
Lin S-M (2013) Local ablation for hepatocellular carcinoma in taiwan. Liver Cancer 2:73–83
Doyle A, Gorgen A, Muaddi H et al (2019) Outcomes of radiofrequency ablation as first-line therapy for hepatocellular carcinoma less than 3 cm in potentially transplantable patients. J Hepatol 70:866–873
Zhang W, Jiang L, Yan L et al (2016) Radiofrequency ablation for HCC patients with multifocal tumours meeting the Milan criteria: a single-centre experience. Dig Liver Dis 48:1485–1491
Choi Y, Jung S-L (2020) Efficacy and safety of thermal ablation techniques for the treatment of primary papillary thyroid microcarcinoma: a systematic review and meta-analysis. Thyroid 30:720–731
Mukasa K, Noh JY, Kunii Y et al (2011) Prevalence of malignant tumors and adenomatous lesions detected by ultrasonographic screening in patients with autoimmune thyroid diseases. Thyroid 21:37–41
Lyu YS, Pyo JS, Cho WJ et al (2021) Clinicopathological significance of papillary thyroid carcinoma located in the isthmus: a meta-analysis. World J Surg 45:2759–2768
Cao X-J, Zhao Z-L, Wei Y et al (2021) Microwave ablation for papillary thyroid cancer located in the thyroid isthmus: a preliminary study. Int J Hyperthermia 38:114–119
Reede DL, Garcon E, Smoker WRK, Kardon R (2008) Horner’s syndrome: clinical and radiographic evaluation. Neuroimaging Clin N Am 18(369–385):xi
Xiao J, Zhang Y, Yan L et al (2021) Ultrasonography-guided radiofrequency ablation for solitary T1aN0M0 and T1bN0M0 papillary thyroid carcinoma: a retrospective comparative study. Eur J Endocrinol 186. https://doi.org/10.1530/EJE-21-0580
Wei Y, Niu W-Q, Zhao Z-L et al (2022 Sep) (2022) Microwave ablation versus surgical resection for solitary T1N0M0 papillary thyroid carcinoma. Radiology 304(3):704–713
Zhou W, Zhang L, Zhan W et al (2016) Percutaneous laser ablation for treatment of locally recurrent papillary thyroid carcinoma <15 mm. Clin Radiol 71:1233–1239
Acknowledgements
We thank all participants for their support in this study.
Funding
This study has received fundings by National Natural Science Foundation of China (Grant No.62176268) and National High Level Hospital Clinical Research Funding (Grant No. 2022-NHLHCRF-PY-07).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Mingan Yu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
-
retrospective
-
diagnostic or prognostic study
-
performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Hd., Yu, Xy., Wei, Y. et al. A clinical study on microwave ablation of multifocal (≤ 3) T1N0M0 papillary thyroid carcinoma. Eur Radiol 33, 4034–4041 (2023). https://doi.org/10.1007/s00330-022-09333-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09333-x