Abstract
Objective
Some patients with acute large vessel occlusion (LVO) presented imaging mismatch, low Alberta Stroke Program Early CT Score (ASPECTS) with small ischemic core, or high ASPECTS with large ischemic core. The study was designed to explore whether patients with imaging mismatch could benefit from endovascular treatment (EVT).
Methods
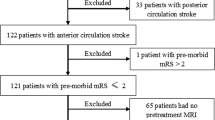
We retrospectively reviewed patients with LVO treated with EVT in our center from March 2018 to Jul 2020. Patients were divided into three groups, imaging mismatch, small ischemic core, and large ischemic core groups. Pooled analyses based on stroke onset to treatment time were done. Multivariate regression analysis was performed to explore the factors for good outcomes.
Results
Sixty-eight of 419 patients with LVO presented with imaging mismatch, and 35 of those (51%) achieved good outcomes after EVT at 90-day. No significant differences were noted in good outcomes and symptomatic intracranial hemorrhage (sICH) between patients with imaging mismatch and small ischemic core. Compared with large ischemic core, patients with imaging mismatch presented lower risk of sICH (95% confidence interval (CI) 0.04–0.75, p = 0.011) within 6 h and higher proportion of good outcomes (95% CI 0.37–0.82, p = 0.002) at 6 to 24 h. Baseline NIHSS (odds ratio (OR) = 0.91, 95% CI 0.88–0.95)), ASPECTS (OR = 1.14, 95% CI 1.01–1.29), ischemic core (OR = 0.99, 95% CI 0.98–1.00), and sICH (OR = 61.61, 95% CI 8.09–461.32) were associated with good outcomes.
Conclusions
Patients with imaging mismatch treated within 24 h could benefit from EVT and without increasing the risk of sICH.
Key Points
• Patients with imaging mismatch between ASPECTS and ischemic core could achieve good outcomes after endovascular treatment.
• Compared with large ischemic core, patients with imaging mismatch presented lower risk of symptomatic hemorrhage within 6 h and higher proportion of good outcomes within 6–24 h.
• Baseline NIHSS score, ASPECTS, ischemic core, and symptomatic intracranial hemorrhage were associated with good outcomes.


Similar content being viewed by others
Abbreviations
- ASITN/SIRs:
-
American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology scale
- ASPECTS:
-
Alberta Stroke Program Early CT Score
- CBF:
-
Relative cerebral blood flow
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- EVT:
-
Endovascular treatment
- HALC:
-
High ASPECTS with large ischemic core
- ICH:
-
Intracranial hemorrhage
- IQR:
-
Inter-quartile range
- LASC:
-
Low ASPECTS with small ischemic core
- LVO:
-
Large vessel occlusions
- mRS:
-
Modified Rankin Scale
- mTICI:
-
Modified thrombolysis in cerebral infarction scale
- NIHSS:
-
National Institutes of Health Stroke Scale
- OR:
-
Odds ratio
- RAPID:
-
Automated computed tomography analysis software
- sICH:
-
Symptomatic intracranial hemorrhage
References
Berkhemer OA, Fransen PS, Beumer D et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20
Saver JL, Goyal M, Bonafe A et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke. N Engl J Med 372:2285–2295
Albers GW, Marks MP, Kemp S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718
Nogueira RG, Jadhav AP, Haussen DC et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21
Goyal M, Menon BK, van Zwam WH et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731
Phan K, Saleh S, Dmytriw AA et al (2019) Influence of ASPECTS and endovascular thrombectomy in acute ischemic stroke: a meta-analysis. J Neurointerv Surg 11:664–669
Davoli A, Motta C, Koch G et al (2018) Pretreatment predictors of malignant evolution in patients with ischemic stroke undergoing mechanical thrombectomy. J Neurointerv Surg 10:340–344
Deb-Chatterji M, Pinnschmidt H, Flottmann F et al (2020) Predictors of independent outcome of thrombectomy in stroke patients with large baseline infarcts in clinical practice: a multicenter analysis. J Neurointerv Surg 12:1064–1068
Rebello LC, Bouslama M, Haussen DC et al (2017) Endovascular treatment for patients with acute stroke who have a large ischemic core and large mismatch imaging profile. JAMA Neurol 74:34–40
Xing PF, Zhang YW, Zhang L et al (2021) Higher baseline cortical score predicts good outcome in patients with low Alberta Stroke Program Early Computed Tomography Score treated with endovascular treatment. Neurosurgery 88:612–618
Haussen DC, Dehkharghani S, Rangaraju S et al (2016) Automated CT perfusion ischemic core volume and noncontrast CT ASPECTS (alberta stroke program early CT score): correlation and clinical outcome prediction in large vessel stroke. Stroke 47:2318–2322
Powers WJ, Rabinstein AA, Ackerson T et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:e344–e418
Xing PF, Zhang YW, Li ZF et al (2020) The “distal-to-proximal” strategy for the treatment of posterior circulation tandem occlusions: a single-centre experience. Neuroradiology 62:867–876
Broocks G, Kniep H, Schramm P et al (2019) Patients with low Alberta Stroke Program Early CT score (ASPECTS) but good collaterals benefit from endovascular recanalization. J Neurointerv Surg 12:747–752
Boned S, Padroni M, Rubiera M et al (2017) Admission CT perfusion may overestimate initial infarct core: the ghost infarct core concept. J Neurointerv Surg 9:66–69
Yoshimura S, Sakai N, Yamagami H et al (2022) Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med 386:1303–1313
Desilles JP, Consoli A, Redjem H et al (2017) Successful reperfusion with mechanical thrombectomy is associated with reduced disability and mortality in patients with pretreatment diffusion-weighted imaging-Alberta Stroke Program Early Computed Tomography Score≤6. Stroke 48:963–969
Tan BY, Wan-Yee K, Paliwal P et al (2016) Good intracranial collaterals trump poor ASPECTS (alberta stroke program early CT score) for intravenous thrombolysis in anterior circulation acute ischemic stroke. Stroke 47:2292–2298
Seyman E, Shaim H, Shenhar-Tsarfaty S et al (2016) The collateral circulation determines cortical infarct volume in anterior circulation ischemic stroke. BMC Neurol 16:206–214
Al-Ajlan FS, Goyal M, Demchuk AM et al (2016) Intra-arterial therapy and post-treatment infarct volumes: insights from the ESCAPE randomized controlled trial. Stroke 47:777–781
Igarashi H, Hamamoto M, Yamaguchi H et al (2003) Cerebral blood flow index: dynamic perfusion MRI delivers a simple and good predictor for the outcome of acute-stage ischemic lesion. J Comput Assist Tomogr 27:874–881
Guenego A, Mlynash M, Christensen S et al (2018) Hypoperfusion ratio predicts infarct growth during transfer for thrombectomy. Ann Neurol 84:616–620
Hao Y, Yang D, Wang H et al (2017) Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke 48:1203–1209
Tian B, Tian X, Shi Z et al (2022) Clinical and imaging indicators of hemorrhagic transformation in acute ischemic stroke after endovascular thrombectomy. Stroke 53:1674–1681
Zhang X, Xie Y, Wang H et al (2020) Symptomatic intracranial hemorrhage after mechanical thrombectomy in Chinese ischemic stroke patients: The ASIAN Score. Stroke 51:2690–2696
Weyland CS, Mokli Y, Vey JA et al (2021) Predictors for failure of early neurological improvement after successful thrombectomy in the anterior circulation. Stroke 52:1291–1298
Acknowledgements
We thank all nurses of the Department of Neurovascular Center for their care on the patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yongwei Zhang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• monocentric study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(JPG 183 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xing, P., Zhou, X., Shen, F. et al. Imaging mismatch between Alberta Stroke Program Early CT Score and perfusion imaging may be a good variable for endovascular treatment. Eur Radiol 33, 2629–2637 (2023). https://doi.org/10.1007/s00330-022-09273-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09273-6