Abstract
Objectives
Several studies have compared the efficacy of hepatic resection (HR) and thermal ablation (TA) for unresectable tumors; however, results remain inconsistent. Most cohorts in previous studies were heterogeneous groups of synchronous colorectal liver metastases (CRLM) and extrahepatic metastases. This retrospective study aimed to compare the therapeutic efficacy between TA and HR in synchronous CRLM without extrahepatic metastases.
Methods
Cases with initially synchronous CRLM without extrahepatic metastases between January 2007 and December 2018 were enrolled. Of the 448 cases, 346 received HR and 102 TA. Propensity score matching with a 1:1 ratio was used to improve the comparability between the HR and TA groups. Technical success, complications, disease-free survival (DFS), and overall survival (OS) were compared before and after matching.
Results
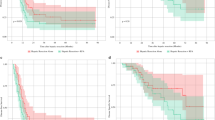
All patients achieved technical success. Major complication rates in the HR and TA groups were, respectively, 36.7% and 8.8% (p < 0.001). Before matching, the 5-year OS and DFS (p = 0.004 and p = 0.020, respectively) were significantly higher in the HR group than in the TA group. After matching, no significant difference in the 5-year OS and DFS was found between the groups (p = 0.770 and p = 0.939, respectively). Local tumor progression rate was significantly higher in the TA group both before (p = 0.027) and after (p = 0.029) matching.
Conclusions
For patients with CRC with synchronous CRLM, TA and HR provide comparable OS and DFS. TA is preferable if complete ablation is predicted.
Key Points
• Thermal ablation and hepatic resection provide comparable overall survival and disease-free survival.
• Thermal ablation is a safe and effective treatment for patients with colorectal cancer with synchronous liver metastases and has a lower major complication rate and higher repeatability than hepatic resection.
• Thermal ablation is preferable if complete ablation is predicted.



Similar content being viewed by others
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- CRC:
-
Colorectal cancer
- CRLM:
-
Colorectal liver metastases
- DFS:
-
Disease-free survival
- IDR:
-
Intrahepatic distant recurrence
- LTP:
-
Local tumor progression
- MDT:
-
Multidisciplinary team
- MWA:
-
Microwave ablation
- OS:
-
Overall survival
- RFA:
-
Radiofrequency ablation
- TA:
-
Thermal ablation
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Gillams A, Goldberg N, Ahmed M et al (2015) Thermal ablation of colorectal liver metastases: a position paper by an international panel of ablation experts, The Interventional Oncology Sans Frontières meeting 2013. Eur Radiol 25:3438–3454
Engstrand J, Nilsson H, Strömberg C, Jonas E, Freedman J (2018) Colorectal cancer liver metastases - a population-based study on incidence, management and survival. BMC Cancer 18:78
Elias D, Viganò L, Orsi F et al (2016) New perspectives in the treatment of colorectal metastases. Liver Cancer 6:90–98
Ahmed M, Brace CL, Lee FT Jr, Goldberg SN (2011) Principles of and advances in percutaneous ablation. Radiology 258:351–369
Sucandy I, Cheek S, Golas BJ, Tsung A, Geller DA, Marsh JW (2016) Longterm survival outcomes of patients undergoing treatment with radiofrequency ablation for hepatocellular carcinoma and metastatic colorectal cancer liver tumors. HPB (Oxford) 18:756–763
Shady W, Petre EN, Gonen M et al (2016) Percutaneous radiofrequency ablation of colorectal cancer liver metastases: factors affecting outcomes--a 10-year experience at a single center. Radiology 278:601–611
Nieuwenhuizen S, Puijk RS, van den Bemd B, et al (2020) Resectability and ablatability criteria for the treatment of liver only colorectal metastases: multidisciplinary consensus document from the COLLISION trial group. Cancers (Basel) 1779. https://doi.org/10.3390/cancers12071779
Vasiniotis Kamarinos N, Sofocleous CT (2020) Imaging and image-guided thermal ablation for oligometastatic colorectal cancer liver disease. Cancer J 26:124–128
McEachron KR, Ankeny JS, Robbins A et al (2021) Surgical microwave ablation of otherwise non-resectable colorectal cancer liver metastases: expanding opportunities for long term survival. Surg Oncol 36:61–64
Reuter NP, Woodall CE, Scoggins CR, McMasters KM, Martin RC (2009) Radiofrequency ablation vs. resection for hepatic colorectal metastasis: therapeutically equivalent? J Gastrointest Surg 13:486–491
Minami Y, Kudo M (2013) Radiofrequency ablation of liver metastases from colorectal cancer: a literature review. Gut Liver 7:1–6
Imai K, Allard MA, Castro Benitez C et al (2017) Long-term outcomes of radiofrequency ablation combined with hepatectomy compared with hepatectomy alone for colorectal liver metastases. Br J Surg 104:570–579
Lei P, Ruan Y, Tan L, Wei H, Chen T (2020) Laparoscopic colorectal resection combined with simultaneous thermal ablation or surgical resection of liver metastasis: a retrospective comparative study. Int J Hyperth 37:137–143
Yang G, Wang G, Sun J et al (2021) The prognosis of radiofrequency ablation versus hepatic resection for patients with colorectal liver metastases: a systematic review and meta-analysis based on 22 studies. Int J Surg 87:105896. https://doi.org/10.1016/j.ijsu.2021.105896
Tinguely P, Dal G, Bottai M, Nilsson H, Freedman J, Engstrand J (2020) Microwave ablation versus resection for colorectal cancer liver metastases - a propensity score analysis from a population-based nationwide registry. Eur J Surg Oncol 46:476–485
van Amerongen MJ, van der Stok EP, Fütterer JJ et al (2019) Results after simultaneous surgery and RFA liver ablation for patients with colorectal carcinoma and synchronous liver metastases. Eur J Surg Oncol 45:2334–2339
Dupré A, Jones RP, Diaz-Nieto R, Fenwick SW, Poston GJ, Malik HZ (2017) Curative-intent treatment of recurrent colorectal liver metastases: a comparison between ablation and resection. Eur J Surg Oncol 43:1901–1907
Xu Y, Shen Q, Wang N et al (2017) Percutaneous microwave ablation of 5-6 cm unresectable hepatocellular carcinoma: local efficacy and long-term outcomes. Int J Hyperth 33:247–254
Xu Y, Shen Q, Liu P et al (2017) Microwave ablation for the treatment of hepatocellular carcinoma that met up-to-seven criteria: feasibility, local efficacy and long-term outcomes. Eur Radiol 27:3877–3887
Xu Y, Shen Q, Wang N et al (2017) Microwave ablation is as effective as radiofrequency ablation for very-early-stage hepatocellular carcinoma. Chin J Cancer 36:14
Teratani T, Yoshida H, Shiina S et al (2006) Radiofrequency ablation for hepatocellular carcinoma in so-called high-risk locations. Hepatology 43:1101–1108
Howard C, Clements TW, Edwards JP et al (2018) Synchronous colorectal liver metastases: a national survey of surgeon opinions on simultaneous resection and multidisciplinary cooperation. Hepatobiliary Surg Nutr 7:242–250
Boudjema K, Locher C, Sabbagh C et al (2021) Simultaneous versus delayed resection for initially resectable synchronous colorectal cancer liver metastases: a prospective, open-label, randomized, controlled trial. Ann Surg 273:49–56
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Kurilova I, Bendet A, Petre EN et al (2020) Factors associated with local tumor control and complications after thermal ablation of colorectal cancer liver metastases: a 15-year retrospective cohort study. Clin Colorectal Cancer S1533-0028(20):30134–30131. https://doi.org/10.1016/j.clcc.2020.09.005
Laimer G, Jaschke N, Schullian P et al (2021) Volumetric assessment of the periablational safety margin after thermal ablation of colorectal liver metastases. Eur Radiol https://doi.org/10.1007/s00330-020-07579-x
Vasiniotis Kamarinos N, Sofocleous CT (2020) Role of image-guided percutaneous thermal ablation in the management of colorectal cancer liver metastases. Hepatobiliary Surg Nutr 9:235–238
Cucchetti A, Zhong J, Berhane S et al (2020) The chances of hepatic resection curing hepatocellular carcinoma. J Hepatol 72:711–717
Franzese C, Comito T, Clerici E et al (2018) Liver metastases from colorectal cancer: propensity score-based comparison of stereotactic body radiation therapy vs. microwave ablation. J Cancer Res Clin Oncol 144:1777–1783
Acknowledgements
The author would thank the staff of the Department of Colorectal Surgery, Fudan University Shanghai Cancer Center. This study was supported by the Science and Technology Commission of Shanghai Municipality (grant numbers: 20DZ1100101 and 19511121202).
Funding
This study was supported by the Science and Technology Commission of Shanghai Municipality (grant numbers: 20DZ1100101 and 19511121202). The funding source played no role in research design and collection, analysis, report writing, and the decision to submit articles for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ye Xu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been reported in previous studies (Reuter et al J Gastrointest Surg 2009 Mar 10.1007/s11605-008-0727-0; Dupré et al Eur J Surg Oncol 2017 Oct 10.1016/j.ejso.2017.08.008; Tinguely et al Eur J Surg Oncol 2020 Mar 10.1016/j.ejso.2019.12.002. While these studies found that patients who received hepatic resection (HR) had better survival and lower local recurrence rates, selection bias was possible because thermal ablation (TA) was mostly used for unresectable CRLM. In addition, cohorts in previous studies were heterogeneous groups of synchronous CRLM, metachronous CRLM, and extrahepatic metastases. Hence, this study aimed to compare the therapeutic efficacy between TA and HR in treating synchronous CRLM without extrahepatic metastases using propensity score matching and to determine the feasibility, local efficacy, and long-term outcomes of TA for patients with synchronous CRLM only.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 18 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Y., Zhang, Y., Zheng, C.Z. et al. Thermal ablation versus hepatic resection for colorectal cancer with synchronous liver metastases: a propensity score matching study. Eur Radiol 32, 6678–6690 (2022). https://doi.org/10.1007/s00330-022-09080-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09080-z