Abstract
Objectives
Patients with colorectal liver metastases (CRLM) who underwent hepatic resection after conversion therapy had a high recurrence rate of nearly 90%. Preoperative DEB-TACE has the potential to prevent postoperative recurrence which has not been elucidated. The objective of this study was to evaluate the safety and efficacy of preoperative DEB-TACE.
Materials and methods
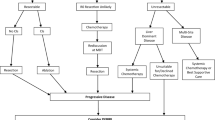
Patients with CRLM who underwent liver resection from June 1, 2016, to June 30, 2021, were collected and those who received conversional hepatectomy were included in this study. Patients with preoperative DEB-TACE were propensity-score matched in a 1:1 ratio to patients without preoperative DEB-TACE. Short-term outcomes and recurrence-free survival (RFS) were compared between the two groups.
Results
After PSM, 44 patients were included in each group. The toxicities of DEB-TACE were mild and could be managed by conservative treatment. Overall response rate (ORR) of conversion therapy (75.0% vs. 81.2%, p = 0.437) and postoperative complication of hepatic resection (27.3% vs. 20.5%, p = 0.453) were similar between the two groups. The median RFS of the DEB-TACE group (10.7 months, 95%CI: 6.6–14.8 months) was significantly longer than that of the control group (8.1 months, 95%CI: 3.4–12.8 months) (HR: 0.60, 95%CI: 0.37–0.95, p = 0.027).
Conclusions
In patients who became resectable after conversion therapy, preoperative DEB-TACE might be a safe option to achieve longer RFS.
Key Points
• This is a propensity-score matching study comparing patients who underwent conversional hepatectomy with or without preoperative DEB-TACE.
• The preoperative DEB-TACE was safe and with mild toxicities (without toxicities more than CTCAE grade 3).
• The preoperative DEB-TACE significantly prolonged the RFS of those patients who underwent conversional hepatectomy (10.7 vs. 8.1 months, p = 0.027).


Similar content being viewed by others
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- CRC:
-
Colorectal carcinoma
- CRLM:
-
Colorectal liver metastases
- CT:
-
Computed tomography
- DEBIRI:
-
Irinotecan drug-eluting beads
- DEB-TACE:
-
Transarterial chemoembolization with drug-eluting beads
- DFS:
-
Disease-free survival
- HAI:
-
Hepatic arterial infusion
- LRFS:
-
Liver recurrence-free survival
- MDT:
-
Multi-disciplinary team
- MRI:
-
Magnetic resonance imaging
- ORR:
-
Overall response rate
- PSM:
-
Propensity-score matching
- PVI:
-
Portal vein infusion
- RECIST:
-
Response Evaluation Criteria In Solid Tumors
- RFA:
-
Radiofrequency ablation
- RFS:
-
Recurrence-free survival
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Gruber-Rouh T, Naguib NN, Eichler K et al (2014) Transarterial chemoembolization of unresectable systemic chemotherapy-refractory liver metastases from colorectal cancer: long-term results over a 10-year period. Int J Cancer 134:1225–1231
Van Cutsem E, Nordlinger B, Cervantes A (2010) Advanced colorectal cancer: ESMO Clinical Practice Guidelines for treatment. Ann Oncol 21(Suppl 5):v93–v97
Adam R (2003) Chemotherapy and surgery: new perspectives on the treatment of unresectable liver metastases. Ann Oncol 14(Suppl 2):ii13–ii16
Maeda Y, Shinohara T, Nagatsu A, Futakawa N, Hamada T (2016) Long-term outcomes of conversion hepatectomy for initially unresectable colorectal liver metastases. Ann Surg Oncol 23(Suppl 2):S242–S248
Folprecht G, Gruenberger T, Bechstein W et al (2014) Survival of patients with initially unresectable colorectal liver metastases treated with FOLFOX/cetuximab or FOLFIRI/cetuximab in a multidisciplinary concept (CELIM study). Ann Oncol 25:1018–1025
de Jong MC, Pulitano C, Ribero D et al (2009) Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg 250:440–448
Mitry E, Fields AL, Bleiberg H et al (2008) Adjuvant chemotherapy after potentially curative resection of metastases from colorectal cancer: a pooled analysis of two randomized trials. J Clin Oncol 26:4906–4911
Nordlinger B, Sorbye H, Glimelius B et al (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14:1208–1215
Lorenz M, Müller HH, Schramm H et al (1998) Randomized trial of surgery versus surgery followed by adjuvant hepatic arterial infusion with 5-fluorouracil and folinic acid for liver metastases of colorectal cancer. German Cooperative on Liver Metastases (Arbeitsgruppe Lebermetastasen). Ann Surg 228:756–762
Kemeny MM, Adak S, Gray B et al (2002) Combined-modality treatment for resectable metastatic colorectal carcinoma to the liver: surgical resection of hepatic metastases in combination with continuous infusion of chemotherapy--an intergroup study. J Clin Oncol 20:1499–1505
Fielding LP, Hittinger R, Grace RH, Fry JS (1992) Randomised controlled trial of adjuvant chemotherapy by portal-vein perfusion after curative resection for colorectal adenocarcinoma. Lancet 340:502–506
Liu Y, Chang W, Zhou B et al (2021) Conventional transarterial chemoembolization combined with systemic therapy versus systemic therapy alone as second-line treatment for unresectable colorectal liver metastases: randomized clinical trial. Br J Surg 108:373–379
Melchiorre F, Patella F, Pescatori L et al (2018) DEB-TACE: a standard review. Future Oncol 14:2969–2984
Huppert P, Wenzel T, Wietholtz H (2014) Transcatheter arterial chemoembolization (TACE) of colorectal cancer liver metastases by irinotecan-eluting microspheres in a salvage patient population. Cardiovasc Intervent Radiol 37:154–164
Ngo A, von Stempel C, Corbo B et al (2019) Transarterial chemoembolisation of colorectal liver metastases with irinotecan-loaded beads: a bi-institutional analysis of 125 treatments in 53 patients. Cardiovasc Intervent Radiol 42:979–990
Lv Y, Feng QY, Wei Y et al (2020) Benefits of multi-disciplinary treatment strategy on survival of patients with colorectal cancer liver metastasis. Clin Transl Med 10:e121
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Tang W, Ren L, Liu T et al (2020) Bevacizumab plus mFOLFOX6 versus mFOLFOX6 alone as first-line treatment for RAS mutant unresectable colorectal liver-limited metastases: the BECOME Randomized Controlled Trial. J Clin Oncol 38:3175–3184
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:309–318 discussion 318-21
Weiser MR (2018) AJCC 8th Edition: Colorectal Cancer. Ann Surg Oncol 25:1454–1455
Hamashige S, Arquilla ER (2008) Common Terminology Criteria for Adverse Events v3.0 (CTCAE). Principles and Practice of Clinical Trial Medicine vol 42, pp 461–533
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Martin RC, Joshi J, Robbins K et al (2011) Hepatic intra-arterial injection of drug-eluting bead, irinotecan (DEBIRI) in unresectable colorectal liver metastases refractory to systemic chemotherapy: results of multi-institutional study. Ann Surg Oncol 18:192–198
Pernot S, Pellerin O, Artru P et al (2020) Intra-arterial hepatic beads loaded with irinotecan (DEBIRI) with mFOLFOX6 in unresectable liver metastases from colorectal cancer: a phase 2 study. Br J Cancer 123:518–524
Martin RC 2nd, Scoggins CR, Schreeder M et al (2015) Randomized controlled trial of irinotecan drug-eluting beads with simultaneous FOLFOX and bevacizumab for patients with unresectable colorectal liver-limited metastasis. Cancer 121:3649–3658
Akinwande O, Dendy M, Ludwig JM, Kim HS (2017) Hepatic intra-arterial injection of irinotecan drug eluting beads (DEBIRI) for patients with unresectable colorectal liver metastases: a systematic review. Surg Oncol 26:268–275
Zhao G, Liu S, Zhang Y et al (2021) Irinotecan eluting beads-transarterial chemoembolization using Callispheres® microspheres is an effective and safe approach in treating unresectable colorectal cancer liver metastases. Ir J Med Sci 191:1139–1145
Fiorentini G, Sarti D, Nani R, Aliberti C, Fiorentini C, Guadagni S (2020) Updates of colorectal cancer liver metastases therapy: review on DEBIRI. Hepat Oncol 7:Hep16
Ye L-C, Liu T-S, Ren L et al (2013) Randomized controlled trial of cetuximab plus chemotherapy for patients with KRAS wild-type unresectable colorectal liver-limited metastases. J Clin Oncol 31:1931–1938
Liu M, Wang K, Wang Y et al (2021) Short- and long-term outcomes of hepatectomy combined with intraoperative radiofrequency ablation for patients with multiple primarily unresectable colorectal liver metastases: a propensity matching analysis. HPB (Oxford) 23:1586–1594
van Amerongen MJ, van der Stok EP, Fütterer JJ et al (2016) Short term and long term results of patients with colorectal liver metastases undergoing surgery with or without radiofrequency ablation. Eur J Surg Oncol 42:523–530
Conci S, Ruzzenente A, Pedrazzani C et al (2021) Simultaneous approach for patients with synchronous colon and rectal liver metastases: impact of site of primary on postoperative and oncological outcomes. Eur J Surg Oncol 47:842–849
Bogach J, Wang J, Griffiths C et al (2020) Simultaneous versus staged resection for synchronous colorectal liver metastases: a population-based cohort study. Int J Surg 74:68–75
Funding
This study has received funding from The National Natural Science Foundation of China (81602035, 81472228, 82072653); The Shanghai Municipal Health Commission: Shanghai Outstanding Youth Specialist Training Program (Q2017-059); Clinical Science and Technology Innovation Project of Shanghai (SHDC12016104); Shanghai Engineering Research Center of Colorectal Cancer Minimally Invasive (17DZ2252600); Youth Fund of Zhongshan Hospital (2019ZSQN28).
Author information
Authors and Affiliations
Contributions
Yu Liu, Bo Zhou, Wentao Tang, and Donghao Xu contributed equally to this work.
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jianmin Xu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Donghao Xu (one of the authors) kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
-
retrospective (a propensity-score matching analysis)
-
observational
-
performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 174 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Y., Zhou, B., Tang, W. et al. Preoperative transarterial chemoembolization with drug-eluting beads (DEB-TACE) in patients undergoing conversional hepatectomy: a propensity-score matching analysis. Eur Radiol 33, 1022–1030 (2023). https://doi.org/10.1007/s00330-022-09063-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09063-0