Abstract
Objectives
To construct a predictive nomogram for differentiating malignant from benign ampullary strictures using contrast-enhanced computed tomography (CT) findings combined with clinical findings.
Methods
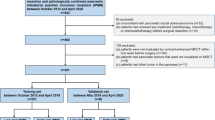
In this retrospective study, 152 patients with ampullary stricture (98 benign and 54 malignant) who underwent contrast-enhanced CT were included. Various imaging findings of the ampulla, bile duct, main pancreatic duct, and periampullary area were evaluated and clinical findings including the presence of jaundice, carbohydrate antigen 19-9 level, and history of cholecystectomy were collected. Among them, statistically significant findings were identified using univariable and multivariable logistic regression analyses. A nomogram was constructed to differentiate benign and malignant ampullary strictures and was internally validated.
Results
Multivariable analysis revealed that jaundice (odds ratio [OR]: 17.33, p < 0.001), presence of an ampullary mass (OR: 24.40, p < 0.001), non-similar enhancement of the ampulla to the duodenum (OR: 31.96, p = 0.003), and proportional dilatation of the bile duct (OR: 7.98, p = 0.001) were independent significant factors for predicting the malignant ampullary stricture, and were used to construct a nomogram. Among them, non-similar enhancement of the ampulla to the duodenum showed the highest OR and predictor point on the nomogram. The calibration plots showed excellent agreement between the predicted probabilities and the actual rates of malignant ampullary strictures, on internal validation.
Conclusions
Combination of clinical and imaging findings could aid in predicting malignant ampullary strictures using significant findings of jaundice, presence of ampullary mass, non-similar enhancement of the ampulla to the duodenum, and proportional dilatation of the bile duct.
Key Points
• The presence of jaundice, ampullary mass, non-similar enhancement of the ampulla, and proportional bile duct dilatation were significant findings for predicting malignant ampullary strictures.
• Non-similar enhancement of the ampulla to the duodenum was a significant feature with the highest odds ratio for differentiating benign and malignant ampullary strictures.
• The nomogram constructed using contrast-enhanced computed tomography imaging and clinical findings could aid in predicting malignant ampullary strictures.






Similar content being viewed by others
Abbreviations
- CA 19-9:
-
Carbohydrate antigen 19-9
- CBD:
-
Common bile duct
- CT:
-
Computed tomography
- EHD:
-
Extrahepatic bile duct
- IHD:
-
Intrahepatic bile duct
- MPD:
-
Main pancreatic duct
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- OR:
-
Odds ratio
- PPV:
-
Positive predictive value
References
Nikolaidis P, Hammond NA, Day K et al (2014) Imaging features of benign and malignant ampullary and periampullary lesions. Radiographics 34:624–641
Kim JHKM, Chung JJ, Lee WJ, Yoo HS, Lee JT (2002) Differential diagnosis of periampullary carcinomas at MR imaging. Radiographics 22:1335–1352
Ahn DH, Bekaii-Saab T (2014) Ampullary cancer: an overview. Am Soc Clin Oncol Educ Book. https://doi.org/10.14694/EdBook_AM.2014.34.112:112-115
Kamisawa T, Tu Y, Egawa N et al (2006) Clinicopathologic features of ampullary carcinoma without jaundice. J Clin Gastroenterol 40:162–166
Todoroki T, Koike N, Morishita Y et al (2003) Patterns and predictors of failure after curative resections of carcinoma of the ampulla of Vater. Ann Surg Oncol 10:1176–1183
Morris-Stiff G, Teli M, Jardine N, Puntis MCA (2009) CA19-9 antigen levels can distinguish between benign and malignant pancreaticobiliary disease. Hepatobiliary Pancreat Dis Int 8:620–626
Alessandrino F, Ivanovic AM, Yee EU, Radulovic D, Souza D, Mortele KJ (2015) MDCT and MRI of the ampulla of Vater. Part I: technique optimization, normal anatomy, and epithelial neoplasms. Abdom Imaging 40:3274–3291
Alessandrino F, Souza D, Ivanovic AM, Radulovic D, Yee EU, Mortele KJ (2015) MDCT and MRI of the ampulla of Vater. Part II: non-epithelial neoplasms, benign ampullary disorders, and pitfalls. Abdom Imaging 40:3292–3312
Angthong W, Jiarakoop K, Tangtiang K (2018) Differentiation of benign and malignant ampullary obstruction by multi-row detector CT. Jpn J Radiol 36:477–488
Chang S, Lim JH, Choi D, Kim SK, Lee WJ (2007) Differentiation of ampullary tumor from benign papillary stricture by thin-section multidetector CT. Abdom Imaging 33:457–462
Chung YE, Kim M-J, Kim HM et al (2011) Differentiation of benign and malignant ampullary obstructions on MR imaging. Eur J Radiol 80:198–203
Andersson M, Kostic S, Johansson M, Lundell L, Asztely M, Hellstrom M (2005) MRI combined with MR cholangiopancreatography versus helical CT in the evaluation of patients with suspected periampullary tumors: a prospective comparative study. Acta Radiol 46:16–27
Jang KM, Kim SH, Lee SJ, Park HJ, Choi D, Hwang J (2013) Added value of diffusion-weighted MR imaging in the diagnosis of ampullary carcinoma. Radiology 266:491–501
Heinzow HS, Kammerer S, Rammes C, Wessling J, Domagk D, Meister T (2014) Comparative analysis of ERCP, IDUS, EUS and CT in predicting malignant bile duct strictures. World J Gastroenterol 20:10495–10503
Ridtitid W, Schmidt SE, Al-Haddad MA et al (2015) Performance characteristics of EUS for locoregional evaluation of ampullary lesions. Gastrointest Endosc 81:380–388
Amin MB, Edge S, Greene F et al (2017) AJCC cancer staging manual, 8th. Springer International Publishing, New York
Gondal B, Aronsohn A (2016) A systematic approach to patients with jaundice. Semin Intervent Radiol 33:253–258
Kim TU, Kim S, Lee JW et al (2008) Ampulla of Vater: comprehensive anatomy, MR imaging of pathologic conditions, and correlation with endoscopy. Eur J Radiol 66:48–64
Lee JM, Boll DT (2018) Disease of the Gallbladder and Biliary Tree. In: Hodler J, Kubik-Huch RA, von Schulthess GK (eds) Diseases of the Abdomen and Pelvis 2018-2021: Diagnostic Imaging - IDKD Book. Springer, Cham (CH), pp 49–56
Kim SW, Kim SH, Lee DH et al (2017) Isolated Main Pancreatic Duct Dilatation: CT Differentiation Between Benign and Malignant Causes. AJR Am J Roentgenol 209:1046–1055
Kim S, Lee NK, Lee JW et al (2007) CT evaluation of the bulging papilla with endoscopic correlation. Radiographics 27:1023–1038
Tsen A, Barbara M, Rosenkranz L (2018) Dilemma of elevated CA 19-9 in biliary pathology. Pancreatology 18:862–867
Wu DS, Chen WX, Wang XD, Acharya R, Jiang XH (2012) Pancreaticobiliary duct changes of periampullary carcinomas: quantitative analysis at MR imaging. Eur J Radiol 81:2112–2117
Acknowledgements
This work was supported by the Soonchunhyang University Research Fund. We thank Ji Eun Moon, MS (Department of Biostatistics, Clinical Trial Center, Soonchunhyang University College of Medicine, Bucheon Hospital) for the statistical analysis of this study.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Seo-Youn Choi, M.D.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
This work was supported by the Department of Biostatistics of our institusion.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 1181 kb)
Rights and permissions
About this article
Cite this article
Lee, J.E., Choi, SY., Lee, M.H. et al. Differentiating between benign and malignant ampullary strictures: a prediction model using a nomogram based on CT imaging and clinical findings. Eur Radiol 32, 7566–7577 (2022). https://doi.org/10.1007/s00330-022-08856-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08856-7