Abstract
Objectives
We aimed to investigate the additional significance of cerebral small vessel disease (SVD) beyond collaterals in determining the clinical outcome after acute ischemic stroke (AIS).
Methods
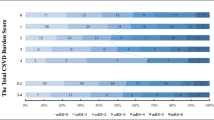
We retrospectively reviewed large vessel-involved stroke patients who had baseline CTA within 24 h after symptom onset and had an MRI scan 5 days after admission from October 1, 2018, to October 31, 2021. Collaterals and SVD markers (including atrophy, leukoaraiosis, lacunes, and perivascular space) were graded on CT angiography and MR images, respectively. Modified Rankin Scale (mRS) score at 90 days was recorded, and mRS ≤ 2 was regarded as a good clinical outcome. The associations between SVD markers, collaterals, and mRS were analyzed using logistic and causal mediation regression.
Results
We finally enrolled 119 patients (70 ± 13 years). The multivariable regression showed atrophy (evidence: OR 0.05 [95% CI 0.01–0.31], p = 0.002; severe: OR 0.08 [95% CI 0.01–0.44], p = 0.007) and evidence of lacune (OR 0.30 [95% CI 0.08–0.96], p = 0.049) were associated with poor clinical outcomes after correcting covariables. Collaterals mediated 25.74% of the effect of atrophy on poor clinical outcomes (p < 0.001), while lacune impacted clinical outcomes without collaterals’ mediation effect (p = 0.54). The classification model with atrophy and lacune had a significantly higher AUC than without markers to distinguish good and poor outcomes (p = 0.036).
Conclusions
Beyond collaterals, brain frailty, specifically assessed by atrophy and lacune, was essential in evaluating stroke patients and could additionally improve the stroke outcome prediction.
Key Points
• Beyond collaterals, brain frailty, specifically assessed by brain atrophy and lacune, was still an independent risk factor of unfavorable clinical outcomes after AIS.
• Adding brain atrophy and lacune into the model has an extra benefit in predicting stroke outcomes.
• The effect of atrophy on stroke outcomes was proportionally mediated through collaterals, but about three-quarters of the effect of brain atrophy and the total effect of lacune directly impacted stroke outcomes without a mediation effect of collaterals.




Similar content being viewed by others
Abbreviations
- ACME:
-
Average causal mediation effect
- ADE:
-
Average direct effect
- AIS:
-
Acute ischemic stroke
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- CTA:
-
Computed tomographic angiography
- EPVS:
-
Enlarged perivascular space
- FLAIR:
-
Fluid-attenuated inversion recovery
- IQR:
-
Interquartile range
- mRS:
-
Modified Rankin Scale
- NIHSS:
-
National Institutes of Health Stroke Scale
- OR:
-
Odds ratio
- ROC:
-
Receiver operating curve
- SVD:
-
Small vessel disease
References
Appleton JP, Woodhouse LJ, Adami A et al (2020) Imaging markers of small vessel disease and brain frailty, and outcomes in acute stroke. Neurology 94:e439–e452
Bu N, Khlif MS, Lemmens R et al (2021) Imaging markers of brain frailty and outcome in patients with acute ischemic stroke. Stroke 52:1004–1011
Cipolla MJ, Liebeskind DS, Chan SL (2018) The importance of comorbidities in ischemic stroke: impact of hypertension on the cerebral circulation. J Cereb Blood Flow Metab 38:2129–2149
De Havenon A, Haynor DR, Tirschwell DL et al (2017) Association of collateral blood vessels detected by arterial spin labeling magnetic resonance imaging with neurological outcome after ischemic stroke. JAMA Neurol 74:453–458
Farrell C, Chappell F, Armitage PA et al (2009) Development and initial testing of normal reference MR images for the brain at ages 65-70 and 75-80 years. Eur Radiol 19:177–183
Giurgiutiu DV, Yoo AJ, Fitzpatrick K et al (2015) Severity of leukoaraiosis, leptomeningeal collaterals, and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke. J Neurointerv Surg 7:326–330
Kim BJ, Lee SH (2015) Prognostic impact of cerebral small vessel disease on stroke outcome. J Stroke 17:101–110
Kongbunkiat K, Wilson D, Kasemsap N et al (2017) Leukoaraiosis, intracerebral hemorrhage, and functional outcome after acute stroke thrombolysis. Neurology 88:638–645
Liebeskind DS, Tomsick TA, Foster LD et al (2014) Collaterals at angiography and outcomes in the interventional management of stroke (IMS) III trial. Stroke 45:759–764
Lin MP, Brott TG, Liebeskind DS et al (2020) Collateral recruitment is impaired by cerebral small vessel disease. Stroke 1404–1410
Lin L, Yang J, Chen C et al (2021) Association of collateral status and ischemic core growth in patients with acute ischemic stroke. Neurology 96:e161–e170
Menon BK, D’Esterre CD, Qazi EM et al (2015) Multiphase CT angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology 275:510–520
Pedersen BK (2019) Physical activity and muscle–brain crosstalk. Nat Rev Endocrinol 15:383–392
Pedraza MI, De Lera M, Bos D et al (2020) Brain atrophy and the risk of futile endovascular reperfusion in acute ischemic stroke. Stroke 51:1514–1521
Raz N, Lindenberger U, Rodrigue KM et al (2005) Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb Cortex 15:1676–1689
Román LS, Menon BK, Blasco J et al (2018) Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol 17:895–904
Schirmer MD, Donahue KL, Nardin MJ et al (2020) Brain volume: an important determinant of functional outcome after acute ischemic stroke. Mayo Clin Proc 95:955–965
Staals J, Makin SDJ, Doubal FN, Dennis MS, Wardlaw JM (2014) Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology 83:1228–1234
Tan JC, Dillon WP, Liu S et al (2007) Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol 61:533–543
Ter Telgte A, Van Leijsen EMC, Wiegertjes K et al (2018) Cerebral small vessel disease: from a focal to a global perspective. Nat Rev Neurol 14:387–398
Vagal A, Aviv R, Sucharew H et al (2018) Collateral clock is more important than time clock for tissue fate a natural history study of acute ischemic strokes. Stroke 49:2102–2107
Van Swieten JC, Koudstaal PJ, Visser MC, Schouten H, Van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Van Swieten JC, Van Gijn J, Hijdra A, Koudstaal PJ (1990) Grading white matter lesions on CT and MRI: a simple scale. J Neurol Neurosurg Psychiatry 53:1080–1083
Wang Z, Xie J, Tang TY et al (2020) Collateral status at single-phase and multiphase CT angiography versus CT perfusion for outcome prediction in anterior circulation acute ischemic stroke. Radiology 296:393–400
Wardlaw JM, Smith EE, Biessels GJ et al (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12:822–838
Wardlaw JM, Smith C, Dichgans M (2013) Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol 12:483–497
Wardlaw JM, Sandercock P, Cohen G et al (2015) Association between brain imaging signs, early and late outcomes, and response to intravenous alteplase after acute ischaemic stroke in the third international stroke trial (IST-3): secondary analysis of a randomised controlled trial. Lancet Neurol 14:485–496
Wittfeld K, Jochem C, Dörr M et al (2020) Cardiorespiratory fitness and gray matter volume in the temporal, frontal, and cerebellar regions in the general population. Mayo Clin Proc 95:44–56
Wong SM, Jansen JFA, Zhang CE et al (2019) Blood-brain barrier impairment and hypoperfusion are linked in cerebral small vessel disease. Neurology 92:e1669–e1677
Zhu N, Jacobs RD, Schreiner JP et al (2015) Cardiorespiratory fitness and brain volume and white matter integrity: the CARDIA Study. Neurology 84:2347–2353
Funding
This study has received funding by Sheng-Hong Ju, Chun-Qiang Lu, and Tian-Yu Tang.
This research was supported by Natural Science Foundation of China (NSFC, No. 61821002, 81830053, 92059202, 82001779, and 82001780), the Key Research and Development Program of Jiangsu Province (BE2020717), and Nation Science Foundation of Jiangsu Province of China (BK20200361, and BK20200368).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Sheng-Hong Ju.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Yuan-Cheng Wang kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed in one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 2290 kb)
Rights and permissions
About this article
Cite this article
Zhou, JY., Shi, YB., Xia, C. et al. Beyond collaterals: brain frailty additionally improves prediction of clinical outcome in acute ischemic stroke. Eur Radiol 32, 6943–6952 (2022). https://doi.org/10.1007/s00330-022-08792-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08792-6