Abstract
Objectives
To determine the association between statin therapy and knee MRI-detected subchondral bone marrow lesion (BML) longitudinal worsening in patients with Heberden’s nodes (HNs) as the hallmark of generalized osteoarthritis (OA) phenotype.
Methods
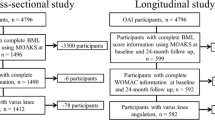
All participants gave informed consent, and IRB approved HIPAA-compliant protocol. We assessed the worsening in BML volume and number of affected subregions in the Osteoarthritis Initiative (OAI) participants with HNs at baseline clinical examination (HN+), using the semi-quantitative MRI Osteoarthritis Knee Scores at baseline and 24 months. Participants were classified according to baseline BML involvement as “no/minimal” (≤ 2/14 knee subregions affected and maximum BML score ≤ 1) or “moderate/severe.” Statin users and non-users were selected using 1:1 propensity-score (PS) matching for OA and cardiovascular disease (CVD)–related potential confounding variables. We assessed the association between statin use and increasing BML score and affected subregions using adjusted mixed-effect regression models.
Results
The PS-matched HN+ participants (63% female, aged 63.5 ± 8.5-year-old) with no/minimal and moderate/severe BML cohorts consisted of 332 (166:166, statin users: non-users) and 380 (190:190) knees, respectively. In the HN+ participants with no/minimal BML, statin use was associated with lower odds of both BML score worsening (odds ratio, 95% confidence interval: 0.62, 0.39–0.98) and increased number of affected subregions (0.54, 0.33–0.88). There was no such association in HN– participants or those HN+ participants with baseline moderate/severe BML.
Conclusion
In patients with CVD indications for statin therapy and generalized OA phenotype (HN+), statin use may be protective against the OA-related subchondral bone damage only in the subgroup of participants with no/minimal baseline BML.
Key Points
• Statin use may reduce the risk of subchondral bone damage in specific osteoarthritis patients with a generalized phenotype, minimal subchondral bone damage, and cardiovascular statin indications.

Similar content being viewed by others
Abbreviations
- BML:
-
Bone marrow lesion
- CVD:
-
Cardiovascular disease
- DMOAD:
-
Disease-modifying osteoarthritis drug
- HN:
-
Heberden’s node
- MIF:
-
Medication inventory form
- MOAKS:
-
MRI Osteoarthritis Knee Score
- OA:
-
Osteoarthritis
- OAI:
-
Osteoarthritis Initiative
- PS:
-
Propensity-score
- SAMS:
-
Statin-associated muscle symptoms
- SMD:
-
Standardized mean difference
References
Bijlsma JWJ, Berenbaum F, Lafeber FPJG (2011) Osteoarthritis: an update with relevance for clinical practice. Lancet 377:2115–2126
Farnaghi S, Prasadam I, Cai G et al (2017) Protective effects of mitochondria-targeted antioxidants and statins on cholesterolinduced osteoarthritis. FASEB J 31:356–367
Kadam UT, Blagojevic M, Belcher J (2013) Statin use and clinical osteoarthritis in the general population: a longitudinal study. J Gen Intern Med 28:943–949
Makris UE, Alvarez CA, Mortensen EM, Mansi IA (2018) Association of statin use with increased risk of musculoskeletal conditions: a retrospective cohort study. Drug Saf 41:939–950
Clockaerts S, Van Osch GJVM, Bastiaansen-Jenniskens YM et al (2012) Statin use is associated with reduced incidence and progression of knee osteoarthritis in the Rotterdam study. Ann Rheum Dis 71:642–647
Wang J, Dong J, Yang J, Wang Y, Liu J (2020) Association between statin use and incidence or progression of osteoarthritis: meta-analysis of observational studies. Osteoarthritis Cartilage 28:1170–1179
Valdes AM, Zhang W, Muir K, Maciewicz RA, Doherty S, Doherty M (2014) Use of statins is associated with a lower prevalence of generalised osteoarthritis. Ann Rheum Dis 73:943–945
Riddle DL, Moxley G, Dumenci L (2013) Associations between Statin use and changes in pain, function and structural progression: a longitudinal study of persons with knee osteoarthritis. Ann Rheum Dis 72:196–203
Michaëlsson K, Lohmander LS, Turkiewicz A, Wolk A, Nilsson P, Englund M (2017) Association between statin use and consultation or surgery for osteoarthritis of the hip or knee: a pooled analysis of four cohort studies. Osteoarthritis Cartilage 25:1804–1813
Mansi IA, Mortensen EM, Pugh MJ, Wegner M, Frei CR (2013) Incidence of musculoskeletal and neoplastic diseases in patients on statin therapy: results of a retrospective cohort analysis. Am J Med Sci 345:343–348
Eymard F, Parsons C, Edwards MH et al (2017) Statin use and knee osteoarthritis progression: results from a post-hoc analysis of the SEKOIA trial. Joint Bone Spine 85:609–614
Chodick G, Amital H, Shalem Y et al (2010) Persistence with statins and onset of rheumatoid arthritis: a population-based cohort study. PLoS Med 7:e1000336–e1000336
Veronese N, Koyanagi A, Stubbs B et al (2019) Statin use and knee osteoarthritis outcomes: a longitudinal cohort study. Arthritis Care Res (Hoboken) 71:1052–1058
Kuusalo L, Felson DT, Wang N et al (2021) Metabolic osteoarthritis - relation of diabetes and cardiovascular disease with knee osteoarthritis. Osteoarthritis Cartilage 29:230–234
Hall AJ, Stubbs B, Mamas MA, Myint PK, Smith TO (2016) Association between osteoarthritis and cardiovascular disease: systematic review and meta-analysis. Eur J Prev Cardiol 23:938–946
Corti MC, Rigon C (2003) Epidemiology of osteoarthritis: prevalence, risk factors and functional impact. Aging Clin Exp Res 15:359–363
Fernandes GS, Valdes AM (2015) Cardiovascular disease and osteoarthritis: common pathways and patient outcomes. Eur J Clin Invest 45:405–414
Ong KL, Wu BJ, Cheung BMY, Barter PJ, Rye K-A (2013) Arthritis: its prevalence, risk factors, and association with cardiovascular diseases in the United States, 1999 to 2008. Ann Epidemiol 23:80–86
Plumb MS, Aspden RM (2004) High levels of fat and (n-6) fatty acids in cancellous bone in osteoarthritis. Lipids Health Dis 3:12
Findlay DM (2007) Vascular pathology and osteoarthritis. Rheumatology 46:1763–1768
Kadam UT (2004) Clinical comorbidity in patients with osteoarthritis: a case-control study of general practice consulters in England and Wales. Ann Rheum Dis 63:408–414
Dore D, Quinn S, Ding C et al (2010) Natural history and clinical significance of MRI-detected bone marrow lesions at the knee: a prospective study in community dwelling older adults. Arthritis Res Ther 12:R223
Wang Y, Jones G, Hill C et al (2020) Effect of atorvastatin on knee structure and pain in patients with knee osteoarthritis: a randomised controlled trial. Osteoarthritis Cartilage 28:S478–S479
Wang Y, Jones G, Hill C et al (2021) Effect of atorvastatin on knee cartilage volume in patients with symptomatic knee osteoarthritis: results from a randomised placebo-controlled trial. Arthritis Rheumatol. https://doi.org/10.1002/art.41760
Haj-Mirzaian A, Mohajer B, Guermazi A et al (2019) Statin use and knee osteoarthritis outcome measures according to the presence of Heberden nodes: results from the Osteoarthritis Initiative. Radiology 293:190557
Kellgren JH, Moore R (1952) Generalized osteoarthritis and Heberden’s nodes. BMJ 1:181–187
Irlenbusch U, Dominick G (2006) Investigations in generalized osteoarthritis. Part 2: Special histological features in generalized osteoarthritis (histological investigations in Heberden’s nodes using a histological score). Osteoarthritis Cartilage 14:428–434
Nelson AE, Smith MW, Golightly YM, Jordan JM (2014) “Generalized osteoarthritis”: a systematic review. Semin Arthritis Rheum 43:713–720
(2016) Overview and Description of Central Image Assessments. Available via https://nda.nih.gov/binaries/content/documents/ndacms/resources/oai/oai-image-assessment-overview/oai-image-assessment-overview/ndacms:resource. Accessed 04/25/2021 2021
Aboulenain S, Saber AY (2021) Primary OsteoarthritisStatPearls. StatPearls Publishing. Copyright © 2021, StatPearls Publishing LLC., Treasure Island (FL)
Hoaglund FT (2013) Primary osteoarthritis of the hip: a genetic disease caused by European genetic variants. J Bone Joint Surg Am 95:463–468
Hunter DJ, Guermazi A, Lo GH et al (2011) Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis Cartilage 19:990–1002
Collins JE, Losina E, Nevitt MC et al (2016) Semiquantitative imaging biomarkers of knee osteoarthritis progression: data From the Foundation for the National Institutes of Health Osteoarthritis Biomarkers Consortium. Arthritis Rheumatol 68:2422–2431
Schisterman EF, Cole SR, Platt RW (2009) Overadjustment Bias and Unnecessary Adjustment in Epidemiologic Studies. Epidemiology 20:488–495
Blagojevic M, Jinks C, Jeffery A, Jordan KP (2010) Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage 18:24–33
Kovari E, Kaposi A, Bekes G et al (2020) Comorbidity clusters in generalized osteoarthritis among female patients: a cross-sectional study. Semin Arthritis Rheum 50:183–191
Haj-Mirzaian A, Mohajer B, Guermazi A et al (2019) Heberden’s nodes and knee osteoarthritis–related osseous structural damage: exploratory study from the osteoarthritis initiative. Arthritis Rheumatol 71:935–940
Smith DA, Galin I (2006) Statin therapy for native and peri-interventional coronary heart disease. Curr Mol Med 6:589–602
Jackevicius CA, Mamdani M, Tu JV (2002) Adherence with statin therapy in elderly patients with and without acute coronary syndromes. ACC Curr J Rev 11:36
Wei MY, Ito MK, Cohen JD, Brinton EA, Jacobson TA (2013) Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol 7:472–483
Warren JR, Falster MO, Fox D, Jorm L (2013) Factors influencing adherence in long-term use of statins. Pharmacoepidemiol Drug Saf 22:1298–1307
Mauskop A, Borden WB (2011) Predictors of Statin Adherence. Curr Cardiol Rep 13:553
Parkinson L, Waters DL, Franck L (2017) Systematic review of the impact of osteoarthritis on health outcomes for comorbid disease in older people. Osteoarthritis Cartilage 25:1751–1770
Mann DM, Allegrante JP, Natarajan S, Halm EA, Charlson M (2007) Predictors of Adherence to Statins for Primary Prevention. Cardiovasc Drugs Ther 21:311–316
Vinker S, Shani M, Baevsky T, Elhayany A (2008) Adherence with statins over 8 years in a usual care setting. Am J Manag Care 14:388–392
Mercado C, DeSimone AK, Odom E et al (2015) Prevalence of cholesterol treatment eligibility and medication use among adults—United States, 2005–2012. 64:1305–1311
Roemer FW, Guermazi A, Collins JE et al (2016) Semi-quantitative MRI biomarkers of knee osteoarthritis progression in the FNIH biomarkers consortium cohort − Methodologic aspects and definition of change. BMC Musculoskelet Disord 17:466
Boudreau DM, Daling JR, Malone KE, Gardner JS, Blough DK, Heckbert SR (2004) A validation study of patient interview data and pharmacy records for antihypertensive, statin, and antidepressant medication use among older women. Am J Epidemiol 159:308–317
Danaei G, Tavakkoli M, Hernan MA (2012) Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol 175:250–262
Force USPST (2016) Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA 316:1997–2007
(2015) New Indications and a Sense of (Re)purpose. EBioMedicine 2:1257–1258
Acknowledgements
The authors would like to thank the participants and staff involved in OAI, FNIH, and POMA projects. Several grants and direct or in-kind contributions provide the publicly available data from the FNIH OA Biomarkers Consortium Project, including AbbVie, Amgen, Arthritis Foundation, Artialis; Bioiberica, BioVendor, DePuy, Flexion Therapeutics, GSK, IBEX, IDS, Merck Serono, Quidel, Rottapharm | Madaus, Sanofi, Stryker, the Pivotal OAI MRI Analyses (POMA) study, NIH HHSN2682010000 21C, and the Osteoarthritis Research Society International. The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners. PGC is supported in part through the UK NIHR Leeds Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the funding partners and sponsors.
Funding
This research was supported by the NIH National Institute of Aging (NIA) under Award Number P01AG066603 and NIH National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) under Award Number R01AR079620-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Shadpour Demehri.
Conflict of interest
FWR is chief marketing officer and shareholder of Boston Imaging Core Lab (BICL), LLC, and consultant to Calibr – California Institute of Biomedical Research and Grünenthal GmbH. AG is a shareholder of BICL and consultant to Pfizer, TissueGene, Merck Serono, Novartis, Regeneron, and AstraZeneca. FB reports personal fees from AstraZeneca, Boehringer, Bone Therapeutics, CellProthera, Expanscience, Galapagos, Gilead, Grunenthal, GSK, Eli Lilly, Merck Sereno, MSD, Nordic, Nordic Bioscience, Novartis, Pfizer, Roche, Sandoz, Sanofi, Servier, UCB, Peptinov, 4P Pharma, grants from TRB Chemedica, non-financial support from 4 Moving Biotech, outside the submitted work. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in the osteoarthritis initiative (OAI) study. Written informed consent was not directly required for this study, since we have used the data of the OAI study.
Ethical approval
Institutional Review Board approval was obtained. The study has received ethics board approval by the institutional review board at the University of California, San Francisco (OAI Coordinating Center; Approval Number: 10-00532), and all enrolled subjects gave informed consent.
Study subjects or cohorts overlap
Osteoarthritis Initiative (OAI) is a well-known publicly available dataset. Some study subjects or cohorts have been previously reported in studies published using the OAI and/or FNIH study. The list of studies on the OAI dataset can be found in the online address of https://nda.nih.gov/oai/publications.
Methodology
• retrospective
• case-control
• multicenter study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mohajer, B., Guermazi, A., Conaghan, P.G. et al. Statin use and MRI subchondral bone marrow lesion worsening in generalized osteoarthritis: longitudinal analysis from Osteoarthritis Initiative data. Eur Radiol 32, 3944–3953 (2022). https://doi.org/10.1007/s00330-021-08471-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08471-y