Abstract
Objectives
To develop and validate an ultrasound elastography radiomics nomogram for preoperative evaluation of the axillary lymph node (ALN) burden in early-stage breast cancer.
Methods
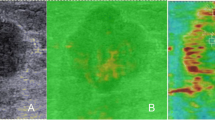
Data of 303 patients from hospital #1 (training cohort) and 130 cases from hospital #2 (external validation cohort) between Jun 2016 and May 2019 were enrolled. Radiomics features were extracted from shear-wave elastography (SWE) and corresponding B-mode ultrasound (BMUS) images. The minimum redundancy maximum relevance and least absolute shrinkage and selection operator algorithms were used to select ALN status–related features. Proportional odds ordinal logistic regression was performed using the radiomics signature together with clinical data, and an ordinal nomogram was subsequently developed. We evaluated its performance using C-index and calibration.
Results
SWE signature, US-reported LN status, and molecular subtype were independent risk factors associated with ALN status. The nomogram based on these variables showed good discrimination in the training (overall C-index: 0.842; 95%CI, 0.773–0.879) and the validation set (overall C-index: 0.822; 95%CI, 0.765–0.838). For discriminating between disease-free axilla (N0) and any axillary metastasis (N + (≥ 1)), it achieved a C-index of 0.845 (95%CI, 0.777–0.914) for the training cohort and 0.817 (95%CI, 0.769–0.865) for the validation cohort. The tool could also discriminate between low (N + (1–2)) and heavy metastatic ALN burden (N + (≥ 3)), with a C-index of 0.827 (95%CI, 0.742–0.913) in the training cohort and 0.810 (95%CI, 0.755–0.864) in the validation cohort.
Conclusion
The radiomics model shows favourable predictive ability for ALN staging in patients with early-stage breast cancer, which could provide incremental information for decision-making.
Key Points
• Radiomics analysis helps radiologists to evaluate the axillary lymph node status of breast cancer with accuracy.
• This multicentre retrospective study showed that radiomics nomogram based on shear-wave elastography provides incremental information for risk stratification.
• Treatment can be given with more precision based on the model.






Similar content being viewed by others
Abbreviations
- ALN:
-
Axillary lymph node
- AUC:
-
Area under the receiver operating characteristic curve
- BMUS:
-
B-mode ultrasound
- CI:
-
Confidence interval
- HER2:
-
Human epidermal growth factor receptor 2
- IHC:
-
Immunohistochemical
- LASSO:
-
Least absolute shrinkage and selection operator
- MRMR:
-
Minimum redundancy maximum relevance
- SLN:
-
Sentinel lymph node
- SWE:
-
Shear-wave elastography
References
Ahmed M, Purushotham AD, Douek M (2014) Novel techniques for sentinel lymph node biopsy in breast cancer: a systematic review. Lancet Oncol 15:e351–e362
Cardoso F, Kyriakides S, Ohno S et al (2019) Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 30:1194–1220
Giuliano AE, Ballman KV, McCall L et al (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis. JAMA 318:918
Giuliano AE, Hunt KK, Ballman KV et al (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305:569–575
Zheng X, Yao Z, Huang Y et al (2020) Deep learning radiomics can predict axillary lymph node status in early-stage breast cancer. Nat Commun 11:1236
Lim GH, Upadhyaya VS, Acosta HA et al (2018) Preoperative predictors of high and low axillary nodal burden in Z0011 eligible breast cancer patients with a positive lymph node needle biopsy result. Eur J Surg Oncol 44:945–950
Chu KU, Turner RR, Hansen NM, Brennan MB, Giuliano AE (1999) Sentinel node metastasis in patients with breast carcinoma accurately predicts immunohistochemically detectable nonsentinel node metastasis. Ann Surg Oncol 6:756–761
Kamath VJ, Giuliano R, Dauway EL et al (2001) Characteristics of the sentinel lymph node in breast cancer predict further involvement of higher-echelon nodes in the axilla: a study to evaluate the need for complete axillary lymph node dissection. Arch Surg 136:688–692
Kim GR, Choi JS, Han BK et al (2018) Preoperative axillary US in early-stage breast cancer: potential to prevent unnecessary axillary lymph node dissection. Radiology 288:55–63
Youk JH, Kwak JY, Lee E, Son EJ, Kim JA (2020) Grayscale ultrasound radiomic features and shear-wave elastography radiomic features in benign and malignant breast masses. Ultraschall Med 41:390–396
Berg WA, Cosgrove DO, Doré CJ et al (2012) Shear-wave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Radiology 262:435–449
Evans A, Rauchhaus P, Whelehan P et al (2014) Does shear wave ultrasound independently predict axillary lymph node metastasis in women with invasive breast cancer? Breast Cancer Res Treat 143:153–157
Zhao Q, Sun JW, Zhou H et al (2018) Pre-operative conventional ultrasound and sonoelastography evaluation for predicting axillary lymph node metastasis in patients with malignant breast lesions. Ultrasound Med Biol 44:2587–2595
Youk JH, Son EJ, Kim JA, Gweon HM (2017) Pre-operative evaluation of axillary lymph node status in patients with suspected breast cancer using shear wave elastography. Ultrasound Med Biol 43:1581–1586
Bi WL, Hosny A, Schabath MB et al (2019) Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J Clin 69:127–157
Yu F, Wang J, Ye X et al (2019) Ultrasound-based radiomics nomogram: a potential biomarker to predict axillary lymph node metastasis in early-stage invasive breast cancer. Eur J Radiol 119:108658
Han L, Zhu Y, Liu Z et al (2019) Radiomic nomogram for prediction of axillary lymph node metastasis in breast cancer. Eur Radiol 29:3820–3829
Koelliker SL, Chung MA, Mainiero MB, Steinhoff MM, Cady B (2008) Axillary lymph nodes: US-guided fine-needle aspiration for initial staging of breast cancer-correlation with primary tumor size. Radiology 246:81–89
Curigliano G, Burstein HJ, Winer EP et al (2017) De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol 28:1700–1712
Zhou J, Zhan W, Chang C et al (2014) Breast lesions: evaluation with shear wave elastography, with special emphasis on the “stiff rim” sign. Radiology 272:63–72
van Griethuysen J, Fedorov A, Parmar C et al (2017) Computational radiomics system to decode the radiographic phenotype. Cancer Res 77:e104–e107
Sauerbrei W, Royston P, Binder H (2007) Selection of important variables and determination of functional form for continuous predictors in multivariable model building. Stat Med 26:5512–5528
Alba AC, Agoritsas T, Walsh M et al (2017) Discrimination and calibration of clinical prediction models: users’ guides to the medical literature. JAMA 318:1377–1384
Pencina MJ, Fine JP, D’Agostino RB (2017) Discrimination slope and integrated discrimination improvement - properties, relationships and impact of calibration. Stat Med 36:4482–4490
Harrell FE (2015) Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Springer, New York
Farrell TPJ, Adams NC, Stenson M et al (2015) The Z0011 Trial: is this the end of axillary ultrasound in the pre-operative assessment of breast cancer patients? Eur Radiol 25:2682–2687
Krag D, Weaver D, Ashikaga T et al (1998) The sentinel node in breast cancer–a multicenter validation study. N Engl J Med 339:941–946
Krag DN, Anderson SJ, Julian TB et al (2007) Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomized phase III trial. Lancet Oncol 8:881–888
Pesek S, Ashikaga T, Krag LE, Krag D (2012) The false-negative rate of sentinel node biopsy in patients with breast cancer: a meta-analysis. World J Surg 36:2239–2251
Goldhirsch A, Winer EP, Coates AS et al (2013) Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol 24:2206–2223
Van Calster B, VandenBempt I, Drijkoningen M et al (2009) Axillary lymph node status of operable breast cancers by combined steroid receptor and HER-2 status: triple positive tumours are more likely lymph node positive. Breast Cancer Res Tr 113:181–187
Voduc KD, Cheang MCU, Tyldesley S et al (2010) Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol 28:1684–1691
Pinker K, Chin J, Melsaether AN, Morris EA, Moy L (2018) Precision medicine and radiogenomics in breast cancer: new approaches toward diagnosis and treatment. Radiology 287:732–747
Lam SW, Jimenez CR, Boven E (2014) Breast cancer classification by proteomic technologies: current state of knowledge. Cancer Treat Rev 40:129–138
Huber KE, Carey LA, Wazer DE (2009) Breast cancer molecular subtypes in patients with locally advanced disease: impact on prognosis, patterns of recurrence, and response to therapy. Semin Radiat Oncol 19:204–210
Guiu S, Michiels S, André F et al (2012) Molecular subclasses of breast cancer: how do we define them? The IMPAKT 2012 Working Group Statement. Ann Oncol 23:2997–3006
Acknowledgements
The authors thank all radiologists of the two hospitals for assisting with collection of the imaging data used in this study. The manuscript has been published as a preprint (DOI:https://doi.org/10.21203/rs.3.rs-75554/v1, LICENSE: under a CC BY 4.0 License), but is not being considered for publication by any other journal.
Funding
This work was supported by the project funded by the China Postdoctoral Science Foundation (2020M682422), Wuhan Science and Technology Bureau (No. 2017060201010181), and Health Commission of Hubei Province (WJ2019M077, WJ2019H227).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Professor Xin-Wu Cui.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• multicentre study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jiang, M., Li, CL., Luo, XM. et al. Radiomics model based on shear-wave elastography in the assessment of axillary lymph node status in early-stage breast cancer. Eur Radiol 32, 2313–2325 (2022). https://doi.org/10.1007/s00330-021-08330-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08330-w