Abstract
Objectives
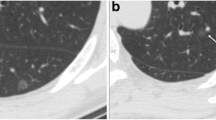
This study aimed to discuss whether a diameter of 3 cm is a threshold for diagnosing lung adenocarcinomas presenting with radiological pure ground-glass mass (PGGM, pure ground-glass opacity > 3 cm) as adenocarcinomas in situ or minimally invasive adenocarcinomas (AIS-MIAs). Another aim was to identify CT features and patient prognosis that differentiate AIS-MIAs from invasive adenocarcinomas (IACs) in patients with PGGMs.
Methods
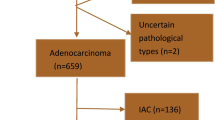
From June 2007 to October 2015, 69 resected PGGMs with HRCT and followed up for ≥ 5 years were included in this study and divided into AIS-MIA (n = 13) and IAC (n = 56) groups. Firth’s logistic regression model was performed to determine CT characteristics that helped distinguish IACs from AIS-MIAs. The discriminatory power of the significant predictors was tested with the area under the receiver operating characteristics curve (AUC). Disease recurrence was also evaluated.
Results
Univariable and multivariable analyses identified that the mean CT attenuation (odds ratio: 1.054, p = 0.0087) was the sole significant predictor for preoperatively discriminating IACs from AIS-MIAs in patients with PGGMs. The CT attenuation had an excellent differentiating accuracy (AUC: 0.981), with the optimal cut-off value at −600 HU (sensitivity: 87.5%; specificity: 100%). Additionally, no recurrence was observed in patients manifesting with PGGMs > 3 cm, and the 5-year recurrence-free survival and overall survival rates were both 100%, even in cases of IAC.
Conclusions
This study demonstrated that PGGMs > 3 cm could still be AIS-MIAs. When PGGMs are encountered in clinical practice, the CT value may be the only valuable parameter to preoperatively distinguish IACs from AIS-MIAs.
Key Points
• Patients with pure ground-glass opacity > 3 cm in diameter are rare but can be diagnosed as adenocarcinomas in situ or minimally invasive adenocarcinomas.
• The mean CT attenuation is the sole significant CT parameter that differentiates invasive adenocarcinoma from adenocarcinoma in situ or minimally invasive adenocarcinoma in patients with pure ground-glass opacity > 3 cm.
• Lung adenocarcinoma with pure ground-glass opacity > 3 cm has an excellent prognosis, even in cases of invasive adenocarcinoma.




Similar content being viewed by others
Abbreviations
- AAH:
-
Atypical adenomatous hyperplasia
- AIS:
-
Adenocarcinomas in situ
- AUC:
-
Area under the curve
- DFS:
-
Disease-free survival
- GGM:
-
Ground-glass mass
- GGN:
-
Ground-glass nodule
- GGO:
-
Ground-glass opacity
- HRCT:
-
High-resolution computed tomography
- HU:
-
Hounsfield unit
- IAC:
-
Invasive adenocarcinomas
- IASLC/ATS/ERS:
-
International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society
- LPA:
-
Lepidic-predominant adenocarcinomas
- LVI:
-
Lymphatic/vascular invasion
- MIA:
-
Minimally invasive adenocarcinomas
- PGGM:
-
Pure ground-glass mass
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- TNM:
-
Tumor, node, and metastasis
- VPI:
-
Visceral pleural invasion
References
Naidich DP, Bankier AA, MacMahon H et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 266:304–317
Zhou QJ, Zheng ZC, Zhu YQ et al (2017) Tumor invasiveness defined by IASLC/ATS/ERS classification of ground-glass nodules can be predicted by quantitative CT parameters. J Thorac Dis 9:1190–1200
Lee HY, Choi YL, Lee KS et al (2014) Pure ground-glass opacity neoplastic lung nodules: histopathology, imaging, and management. AJR Am J Roentgenol 202:W224–W233
Jin X, Zhao SH, Gao J et al (2015) CT characteristics and pathological implications of early stage (T1N0M0) lung adenocarcinoma with pure ground-glass opacity. Eur Radiol 25:2532–2540
Lim HJ, Ahn S, Lee KS et al (2013) Persistent pure ground-glass opacity lung nodules ≥ 10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 144:1291–1299
Zhao Q, Wang JW, Yang L, Xue LY, Lu WW (2019) CT diagnosis of pleural and stromal invasion in malignant subpleural pure ground-glass nodules: an exploratory study. Eur Radiol 29:279–286
Chang B, Hwang JH, Choi YH et al (2013) Natural history of pure ground-glass opacity lung nodules detected by low-dose CT scan. Chest 143:172–178
Li W, Zhou F, Wan Z et al (2019) Clinicopathologic features and lymph node metastatic characteristics in patients with adenocarcinoma manifesting as part-solid nodule exceeding 3cm in diameter. Lung Cancer 136:37–44
Travis WD, Brambilla E, Noguchi M et al (2011) International Association for the Study of Lung Cancer / American Thoracic Society / European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6(2):244–285
Travis WD, Asamura H, Bankier AA et al (2016) The IASLC lung cancer staging project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol 11:1204–1223
Travis WD, Brambilla E, Nicholson AG et al (2015) The 2015 World Health Organization classification of lung tumors. J Thorac Oncol 10:1243–1260
Kadota K, Villena-Vargas J, Yoshizawa A et al (2014) Prognostic significance of adenocarcinoma in situ, minimally invasive adenocarcinoma, and nonmucinous lepidic predominant invasive adenocarcinoma of the lung in patients with stage I disease. Am J Surg Pathol 38:448–460
Borczuk AC, Qian F, Kazeros A (2009) Invasive size is an independent predictor of survival in pulmonary adenocarcinoma. Am J Surg Pathol 33:462–469
Maeshima AM, Tochigi N, Yoshida A, Asamura H, Tsuta K, Tsuda H (2010) Histological scoring for small lung adenocarcinomas 2 cm or less in diameter: a reliable prognostic indicator. J Thorac Oncol 5:333–339
Eguchi T, Kondo R, Kawakami S et al (2014) Computed tomography attenuation predicts the growth of pure ground-glass nodules. Lung Cancer 84:242–247
Firth D (1993) Bias reduction of maximum likelihood estimates. Biometrika 80:27–38
Heinze G, Schemper M (2002) A solution to the problem of separation in logistic regression. Stat Med 21:2409–2419
Aoki T, Tomoda Y, Watanabe H et al (2001) Peripheral lung adenocarcinoma: correlation of thin-section CT findings with histologic prognostic factors and survival. Radiology 220:803–809
Yang ZG, Sone S, Takashima S et al (2001) High-resolution CT analysis of small peripheral lung adenocarcinomas revealed on screening helical CT. AJR Am J Roentgenol 176:1399–1407
Noguchi M (2010) Stepwise progression of pulmonary adenocarcinoma--clinical and molecular implications. Cancer Metastasis Rev 29:15–21
Eguchi T, Kadota K, Park BJ, Travis WD, Jones DR, Adusumilli PS (2014) The new IASLC-ATS-ERS lung adenocarcinoma classification: what the surgeon should know. Semin Thorac Cardiovasc Surg 26:210–222
Yanagawa N, Shiono S, Abiko M, Ogata SY, Sato T, Tamura G (2013) New IASLC/ATS/ERS classification and invasive tumor size are predictive of disease recurrence in stage I lung adenocarcinoma. J Thorac Oncol 8:612–618
Sasada S, Nakayama H, Miyata Y et al (2015) Comparison of malignant grade between pure and partially invasive types of early lung adenocarcinoma. Ann Thorac Surg 99:956–960
Chao L, Yi-Sheng H, Yu C et al (2014) Relevance of EGFR mutation with micropapillary pattern according to the novel IASLC/ATS/ERS lung adenocarcinoma classification and correlation with prognosis in Chinese patients. Lung Cancer 86:164–169
Sumiyoshi S, Yoshizawa A, Sonobe M et al (2013) Pulmonary adenocarcinomas with micropapillary component significantly correlate with recurrence, but can be well controlled with EGFR tyrosine kinase inhibitors in the early stages. Lung Cancer 81:53–59
Ghaly G, Rahouma M, Kamel MK et al (2017) Clinical predictors of nodal metastases in peripherally clinical T1a N0 non-small cell lung cancer. Ann Thorac Surg 104:1153–1158
Aokage K, Miyoshi T, Ishii G et al (2018) Influence of ground glass opacity and the corresponding pathological findings on survival in patients with clinical stage I non-small cell lung cancer. J Thorac Oncol 13:533–542
Acknowledgements
The authors gratefully acknowledge the help of Mr. Aijun You (Research Center for Translational Medicine, Shanghai East Hospital, Tongji University School of Medicine), who kindly provided statistical guidance for this manuscript.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Wei Li.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Aijun You kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• cross-sectional study/diagnostic or prognostic study/observational /
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 321 kb)
Rights and permissions
About this article
Cite this article
Sun, K., Xie, H., Zhao, J. et al. A clinicopathological study of lung adenocarcinomas with pure ground-glass opacity > 3 cm on high-resolution computed tomography. Eur Radiol 32, 174–183 (2022). https://doi.org/10.1007/s00330-021-08115-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08115-1