Abstract
Objective
To explore the value of computed tomography perfusion (CTP) imaging for evaluating the efficacy of encephaloduroarteriosynangiosis (EDAS) treatment of moyamoya syndrome (MMS).
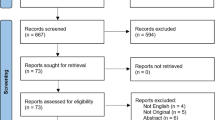
Methods
Forty-three patients with MMS (48 hemispheres) who received EDAS treatment were examined using CTP and DSA before and after surgery. CTP of the ipsilateral cortex, contralateral mirror area, and pons region were measured, and the relative cerebral blood flow (rCBF) and volume (rCBV), mean transit time (rMTT), and time-to-peak (rTTP) were calculated. Based on postoperative DSA, 48 hemispheres were apportioned to two groups based on rich (grades 2, 3) or poor (grades 0, 1) collateral vessel formation, and the pre- and post-operative differences in perfusion changes were compared. The association between clinical outcome, CTP, and the degree of DSA collateral vessels was explored.
Results
rCBF and rMTT significantly improved in both the poor and rich collateral vessel formation groups (n = 21 and 27, respectively), while rTTP significantly improved only in the latter. Postoperative CTP improved in the rich and the grade 1 collateral vessel groups (p < 0.01). The clinical improvement was consistent with the improvement of CTP (p = 0.07), but less consistent with the degree of collateral angiogenesis (p = 0.003).
Conclusion
CTP can quantitatively evaluate the improvement of brain tissue perfusion in the operated area after EDAS. Brain tissue perfusion in operated areas improved regardless of postoperative rich or poor collateral vessel formation observed via DSA. A significant improvement in rTTP in the operated area may indicate the formation of abundant collateral vessels.
Key Points
• CTP showed that brain tissue perfusion in the operated area after EDAS improved regardless of rich or poor collateral vessel formation observed via DSA.
• Significant improvement of rTTP in the operated area may indicate the formation of abundant collateral vessels.





Similar content being viewed by others
Abbreviations
- CBF:
-
Cerebral blood flow
- CBV:
-
Cerebral blood volume
- CTP:
-
Computed tomography perfusion
- DSA:
-
Digital subtraction angiography
- EDAS:
-
Encephaloduroarteriosynangiosis
- MCA:
-
Middle cerebral artery
- MMS:
-
Moyamoya syndrome
- mRS:
-
Modified Rankin scale
- MTT:
-
Mean transit time
- ROC:
-
Receiver operating characteristic
- TTP:
-
Time-to-peak
References
Research Committee on the Pathology and Treatment of Spontaneous Occlusion of the Circle of Willis; Health Labour Sciences Research Grant for Research on Measures for Infractable Diseases (2012) Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52(5):245–266. https://doi.org/10.2176/nmc.52.245
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360(12):1226–1237. https://doi.org/10.1056/NEJMra0804622
Jang DK, Lee KS, Rha HK et al (2017) Bypass surgery versus medical treatment for symptomatic moyamoya disease in adults. J Neurosurg 127(3):492–502. https://doi.org/10.3171/2016.8.jns152875
Hallemeier CL, Rich KM, Grubb RL Jr et al (2006) Clinical features and outcome in North American adults with moyamoya phenomenon. Stroke 37(6):1490–1496. https://doi.org/10.1161/01.STR.0000221787.70503.ca
Yamada S, Oki K, Itoh Y et al (2016) Effects of surgery and antiplatelet therapy in ten-year follow-up from the Registry Study of Research Committee on moyamoya disease in Japan. J Stroke Cerebrovasc Dis 25(2):340–349. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.10.003
Ren B, Zhang ZS, Liu WW et al (2016) Surgical outcomes following encephaloduroarteriosynangiosis in adult moyamoya disease associated with type 2 diabetes. J Neurosurg 125(2):308–314. https://doi.org/10.3171/2015.7.jns15218
Acker G, Fekonja L, Vajkoczy P (2018) Surgical management of moyamoya disease. Stroke 49(2):476–482. https://doi.org/10.1161/strokeaha.117.018563
Lee S, Rivkin MJ, Kirton A, deVeber G, Elbers J (2017) Moyamoya disease in children: results from the International Pediatric Stroke Study. J Child Neurol 32(11):924–929. https://doi.org/10.1177/0883073817718730
Kim T, Oh CW, Bang JS, Kim JE, Cho WS (2016) Moyamoya disease: treatment and outcomes. J Stroke 18(1):21–30. https://doi.org/10.5853/jos.2015.01739
Kuroda S, Houkin K (2012) Bypass surgery for moyamoya disease: concept and essence of sugical techniques. Neurol Med Chir (Tokyo) 52(5):287–294. https://doi.org/10.2176/nmc.52.287
Jeon JP, Kim JE, Cho WS, Bang JS, Son YJ, Oh CW (2018) Meta-analysis of the surgical outcomes of symptomatic moyamoya disease in adults. J Neurosurg 128(3):793–799. https://doi.org/10.3171/2016.11.jns161688
Gonzalez NR, Dusick JR, Connolly M et al (2015) Encephaloduroarteriosynangiosis for adult intracranial arterial steno-occlusive disease: long-term single-center experience with 107 operations. J Neurosurg 123(3):654–661. https://doi.org/10.3171/2014.10.jns141426
Park SE, Kim JS, Park EK, Shim KW, Kim DS (2018) Direct versus indirect revascularization in the treatment of moyamoya disease. J Neurosurg 129(2):480–489. https://doi.org/10.3171/2017.5.jns17353
Kuroda S, Nakayama N, Yamamoto S et al (2020) Late (5-20 years) outcomes after STA-MCA anastomosis and encephalo-duro-myo-arterio-pericranial synangiosis in patients with moyamoya disease. J Neurosurg:1–8. https://doi.org/10.3171/2019.12.jns192938
Liu P, Han C, Li DS, Lv XL, Li YX, Duan L (2016) Hemorrhagic moyamoya disease in children: clinical, angiographic features, and long-term surgical outcome. Stroke 47(1):240–243. https://doi.org/10.1161/strokeaha.115.010512
Choi JW, Chong S, Phi JH et al (2020) Postoperative symptomatic cerebral infarction in pediatric moyamoya disease: risk factors and clinical outcome. World Neurosurg 136:e158–e164. https://doi.org/10.1016/j.wneu.2019.12.072
Ogawa S, Abe H, Katsuta T et al (2017) Early and noninvasive evaluation using superficial temporal artery duplex ultrasonography after indirect bypass for adult ischemic moyamoya disease. Acta Neurochir 159(3):577–582. https://doi.org/10.1007/s00701-016-3073-0
Riordan CP, Storey A, Cote DJ, Smith ER, Scott RM (2019) Results of more than 20 years of follow-up in pediatric patients with moyamoya disease undergoing pial synangiosis. J Neurosurg Pediatr:1–7. https://doi.org/10.3171/2019.1.peds18457
Bao XY, Zhang Y, Wang QN et al (2018) Long-term outcomes after encephaloduroarteriosynangiosis in adult patients with moyamoya disease presenting with ischemia. World Neurosurg 115:e482–e489. https://doi.org/10.1016/j.wneu.2018.04.076
Macyszyn L, Attiah M, Ma TS et al (2017) Direct versus indirect revascularization procedures for moyamoya disease: a comparative effectiveness study. J Neurosurg 126(5):1523–1529. https://doi.org/10.3171/2015.8.jns15504
Duan L, Bao XY, Yang WZ et al (2012) Moyamoya disease in China: its clinical features and outcomes. Stroke 43(1):56–60. https://doi.org/10.1161/strokeaha.111.621300
Starke RM, Komotar RJ, Hickman ZL et al (2009) Clinical features, surgical treatment, and long-term outcome in adult patients with moyamoya disease. Clinical article. J Neurosurg 111(5):936–942. https://doi.org/10.3171/2009.3.jns08837
Wang QN, Bao XY, Zhang Y, Zhang Q, Li DS, Duan L (2019) Encephaloduroarteriosynangiosis for hemorrhagic moyamoya disease: long-term outcome of a consecutive series of 95 adult patients from a single center. J Neurosurg 130(6):1898–1905. https://doi.org/10.3171/2017.12.jns172246
Pandey P, Steinberg GK (2011) Outcome of repeat revascularization surgery for moyamoya disease after an unsuccessful indirect revascularization. Clinical article. J Neurosurg 115(2):328–336. https://doi.org/10.3171/2011.3.jns101908
Yoo M, Jin SC, Jin SJ, Choi BS (2015) Salvage STA-MCA bypass surgery in an adult moyamoya patient after failed indirect revascularization surgery. Br J Neurosurg 29(6):868–870. https://doi.org/10.3109/02688697.2015.1071336
Abla AA, Gandhoke G, Clark JC et al (2013) Surgical outcomes for moyamoya angiopathy at barrow neurological institute with comparison of adult indirect encephaloduroarteriosynangiosis bypass, adult direct superficial temporal artery-to-middle cerebral artery bypass, and pediatric bypass: 154 revascularization surgeries in 140 affected hemispheres. Neurosurgery 73(3):430–439. https://doi.org/10.1227/neu.0000000000000017
Kronenburg A, Bulder MMM, Bokkers RPH et al (2019) Cerebrovascular reactivity measured with ASL perfusion MRI, Ivy Sign, and regional tissue vascularization in moyamoya. World Neurosurg 125:e639–e650. https://doi.org/10.1016/j.wneu.2019.01.140
Chen Y, Xu W, Guo X et al (2016) CT perfusion assessment of moyamoya syndrome before and after direct revascularization (superficial temporal artery to middle cerebral artery bypass). Eur Radiol 26(1):254–261. https://doi.org/10.3171/2017.5.jns1735310.1007/s00330-015-3802-4
Zhang J, Wang J, Geng D, Li Y, Song D, Gu Y (2013) Whole-brain CT perfusion and CT angiography assessment of Moyamoya disease before and after surgical revascularization: preliminary study with 256-slice CT. PLoS One 8(2):e57595. https://doi.org/10.1371/journal.pone.0057595
Ravindra VM, Kralik SF, Griauzde J, Gadgil N, LoPresti MA, Lam S (2020) Preoperative computed tomography perfusion in pediatric moyamoya disease: a single-institution experience. J Neurosurg Pediatr:1–8. https://doi.org/10.3171/2019.10.peds19450
Dai DW, Zhao WY, Zhang YW et al (2013) Role of CT perfusion imaging in evaluating the effects of multiple burr hole surgery on adult ischemic Moyamoya disease. Neuroradiology 55(12):1431–1438. https://doi.org/10.1007/s00234-013-1291-1
Matsushima T, Inoue T, Suzuki SO, Fujii K, Fukui M, Hasuo K (1992) Surgical treatment of moyamoya disease in pediatric patients--comparison between the results of indirect and direct revascularization procedures. Neurosurgery 31(3):401–405. https://doi.org/10.1227/00006123-199209000-00003
Zhao Y, Li J, Lu J et al (2019) Predictors of neoangiogenesis after indirect revascularization in moyamoya disease: a multicenter retrospective study. J Neurosurg:1–11. https://doi.org/10.4103/1673-5374.24923410.3171/2018.9.jns181562
Matsushima Y, Fukai N, Tanaka K et al (1981) A new surgical treatment of moyamoya disease in children: a preliminary report. Surg Neurol 15(4):313–320. https://doi.org/10.1016/s0090-3019(81)80017-1
Lin N, Aronson JP, Manjila S, Smith ER, Scott RM (2014) Treatment of Moyamoya disease in the adult population with pial synangiosis. J Neurosurg 120(3):612–617. https://doi.org/10.3171/2013.11.jns131027
Yun TJ, Cheon JE, Na DG et al (2009) Childhood moyamoya disease: quantitative evaluation of perfusion MR imaging--correlation with clinical outcome after revascularization surgery. Radiology 251(1):216–223. https://doi.org/10.1148/radiol.2511080654
Dusick JR, Gonzalez NR, Martin NA (2011) Clinical and angiographic outcomes from indirect revascularization surgery for Moyamoya disease in adults and children: a review of 63 procedures. Neurosurgery 68(1):34–43; discussion 43. https://doi.org/10.1227/NEU.0b013e3181fc5ec2
Sasaki M, Kudo K, Honjo K, Hu JQ, Wang HB, Shintaku K (2011) Prediction of infarct volume and neurologic outcome by using automated multiparametric perfusion-weighted magnetic resonance imaging in a primate model of permanent middle cerebral artery occlusion. J Cereb Blood Flow Metab 31(2):448–456. https://doi.org/10.1038/jcbfm.2010.106
Laiwalla AN, Kurth F (2017) Evaluation of encephaloduroarteriosynangiosis efficacy using probabilistic independent component analysis applied to dynamic susceptibility contrast perfusion MRI. AJNR Am J Neuroradiol 38(3):507–514. https://doi.org/10.3174/ajnr.A5041
Ha JY, Choi YH (2019) Arterial spin labeling MRI for quantitative assessment of cerebral perfusion before and after cerebral revascularization in children with moyamoya disease. Korean J Radiol 20(6):985–996. https://doi.org/10.3348/kjr.2018.0651
Funding
This study was supported by the Shandong Provincial Development Program of Medical Science and Technology (No. 2016WS0185), and the Jining Key Research and Development Program (No. 2017SMNS012).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Deguo Liu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 609 kb)
Rights and permissions
About this article
Cite this article
Guo, X., Yuan, X., Gao, L. et al. Encephaloduroarteriosynangiosis (EDAS) treatment of moyamoya syndrome: evaluation by computed tomography perfusion imaging. Eur Radiol 31, 8364–8373 (2021). https://doi.org/10.1007/s00330-021-07960-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07960-4