Abstract
Objectives
We aimed to assess the prevalence of coexistence of coronary microvascular dysfunction (CMD) in patients with intermediate epicardial stenosis and to explore coronary computed tomography angiography (CCTA)–derived lesion-, vessel-, and cardiac fat–related characteristic findings associated with CMD.
Methods
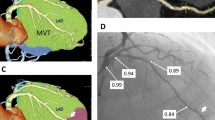
A retrospective cross-sectional single-center study included a total of 177 patients with intermediate stenosis in the left anterior descending artery (LAD) who underwent CCTA and invasive physiological measurements. The 320-slice CCTA analysis included qualitative and quantitative assessments of plaque, vessel, epicardial fat volume (ECFV) and epicardial fat attenuation (ECFA), and pericoronary fat attenuation (FAI). CMD was defined by the index of microcirculatory resistance (IMR) ≥ 25.
Results
In the entire cohort, median fractional flow reserve (FFR) and median IMR values were 0.77 (0.69–0.84) and 19.0 (13.7–27.7), respectively. The prevalence of CMD was 32.8 % (58/177) in the total cohort. The coexistence of CMD and functionally significant stenosis was 34.3 % (37/108), whereas CMD in nonsignificant intermediate stenosis was 30.4 % (21/69). CMD was significantly associated with greater lumen volume (p = 0.031), greater fibrofatty and necrotic component (FFNC) volume (p = 0.030), and greater ECFV (p = 0.030), but not with FAI (p = 0.832) and ECFA (p = 0.445). On multivariable logistic regression analysis, vessel volume, vessel lumen volume, lesion remodeling index, ECFV, and lesion FFNC volume were independent predictors of CMD.
Conclusions
The prevalence of CMD was about one-third in patients with intermediate stenosis in LAD regardless of the presence or absence of functional stenosis significance. The integrated CCTA assessment may help in the identification of CMD.
Key Points
• The coexistence of coronary microvascular dysfunction (CMD) and functionally significant stenosis was 34.3 %, whereas CMD in nonsignificant intermediate stenosis was 30.4 %.
• Coronary computed tomography angiography (CCTA)-derived CMD characteristics were vessel volume, vessel lumen volume, remodeling index, epicardial fat volume, and fibrofatty necrotic core volume.
• Integrated CCTA assessment may help identify the coexistence of CMD and epicardial stenosis.




Similar content being viewed by others
Abbreviations
- CABG:
-
Coronary artery bypass graft surgery
- CAD:
-
Coronary artery disease
- CCTA:
-
Coronary computed tomography angiography
- CFR:
-
Coronary flow reserve
- CMD:
-
Coronary microvascular dysfunction
- ECFA:
-
Epicardial fat attenuation
- ECFV:
-
Epicardial fat volume
- ESS:
-
Endothelial shear stress
- FFNC:
-
Fibrofatty and necrotic component
- FFR:
-
Fractional flow reserve
- IMR:
-
Index of microcirculatory resistance
- LAD:
-
Left anterior descending artery
- MVD:
-
Microvascular dysfunction
- PCI:
-
Percutaneous coronary intervention
References
Gupta A, Taqueti VR, van de Hoef TP et al (2017) Integrated noninvasive physiological assessment of coronary circulatory function and impact on cardiovascular mortality in patients with stable coronary artery disease. Circulation 136:2325–2336
Taqueti VR, Hachamovitch R, Murthy VL et al (2015) Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 131:19–27
Ziadi MC, Dekemp RA, Williams KA et al (2011) Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol 58:740–748
Jespersen L, Hvelplund A, Abildstrom SZ et al (2012) Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 33:734–744
Maddox TM, Stanislawski MA, Grunwald GK et al (2014) Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 312:1754–1763
Mathew RC, Bourque JM, Salerno M, Kramer CM (2020) Cardiovascular imaging techniques to assess microvascular dysfunction. JACC Cardiovasc Imaging 13:1577–1590
SCOT-HEART investigators (2015) CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 385:2383–2391
Douglas PS, Hoffmann U, Patel MR et al (2015) Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 372:1291–1300
Versteylen MO, Kietselaer BL, Dagnelie PC et al (2013) Additive value of semiautomated quantification of coronary artery disease using cardiac computed tomographic angiography to predict future acute coronary syndrome. J Am Coll Cardiol 61:2296–2305
Ovrehus KA, Gaur S, Leipsic J et al (2018) CT-based total vessel plaque analyses improves prediction of hemodynamic significance lesions as assessed by fractional flow reserve in patients with stable angina pectoris. J Cardiovasc Comput Tomogr 12:344–349
Lee SE, Park HB, Xuan D et al (2019) Consistency of quantitative analysis of coronary computed tomography angiography. J Cardiovasc Comput Tomogr 13:48–54
Antonopoulos AS, Sanna F, Sabharwal N et al (2017) Detecting human coronary inflammation by imaging perivascular fat. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aal2658
Oikonomou EK, Marwan M, Desai MY et al (2018) Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet 392:929–939
Ford TJ, Ong P, Sechtem U et al (2020) Assessment of vascular dysfunction in patients without obstructive coronary artery disease: why, how, and when. JACC Cardiovasc Interv 13:1847–1864
Taylor AJ, Cerqueira M, Hodgson JM et al (2010) ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography. A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol 56:1864–1894
Leipsic J, Abbara S, Achenbach S et al (2014) SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 8:342–358
Maurovich-Horvat P, Ferencik M, Voros S, Merkely B, Hoffmann U (2014) Comprehensive plaque assessment by coronary CT angiography. Nat Rev Cardiol 11:390–402
Motoyama S, Ito H, Sarai M et al (2015) Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J Am Coll Cardiol 66:337–346
Lee JM, Choi KH, Koo BK et al (2019) Prognostic implications of plaque characteristics and stenosis severity in patients with coronary artery disease. J Am Coll Cardiol 73:2413–2424
Chang HJ, Lin FY, Lee SE et al (2018) Coronary atherosclerotic precursors of acute coronary syndromes. J Am Coll Cardiol 71:2511–2522
Heo R, Park HB, Lee BK et al (2016) Optimal boundary detection method and window settings for coronary atherosclerotic plaque volume analysis in coronary computed tomography angiography: comparison with intravascular ultrasound. Eur Radiol 26:3190–3198
Park HB, Lee BK, Shin S et al (2015) Clinical feasibility of 3D automated coronary atherosclerotic plaque quantification algorithm on coronary computed tomography angiography: comparison with intravascular ultrasound. Eur Radiol 25:3073–3083
Nakazato R, Shalev A, Doh JH et al (2013) Aggregate plaque volume by coronary computed tomography angiography is superior and incremental to luminal narrowing for diagnosis of ischemic lesions of intermediate stenosis severity. J Am Coll Cardiol 62:460–467
Gaur S, Ovrehus KA, Dey D et al (2016) Coronary plaque quantification and fractional flow reserve by coronary computed tomography angiography identify ischaemia-causing lesions. Eur Heart J 37:1220–1227
Oda S, Utsunomiya D, Funama Y et al (2016) Effect of iterative reconstruction on variability and reproducibility of epicardial fat volume quantification by cardiac CT. J Cardiovasc Comput Tomogr 10:150–155
Yong AS, Layland J, Fearon WF et al (2013) Calculation of the index of microcirculatory resistance without coronary wedge pressure measurement in the presence of epicardial stenosis. JACC Cardiovasc Interv 6:53–58
Lee JM, Layland J, Jung JH et al (2015) Integrated physiologic assessment of ischemic heart disease in real-world practice using index of microcirculatory resistance and fractional flow reserve: insights from the International Index of Microcirculatory Resistance Registry. Circ Cardiovasc Interv. https://doi.org/10.1161/CIRCINTERVENTIONS.115.002857
Stenstrom I, Maaniitty T, Uusitalo V et al (2017) Frequency and angiographic characteristics of coronary microvascular dysfunction in stable angina: a hybrid imaging study. Eur Heart J Cardiovasc Imaging 18:1206–1213
Ford TJ, Stanley B, Good R et al (2018) Stratified medical therapy using invasive coronary function testing in angina: the CorMicA trial. J Am Coll Cardiol 72:2841–2855
Crea F, Camici PG, Bairey Merz CN (2014) Coronary microvascular dysfunction: an update. Eur Heart J 35:1101–1111
Camici PG, d’Amati G, Rimoldi O (2015) Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol 12:48–62
Taqueti VR, Di Carli MF (2018) Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol 72:2625–2641
Siasos G, Sara JD, Zaromytidou M et al (2018) Local low shear stress and endothelial dysfunction in patients with nonobstructive coronary atherosclerosis. J Am Coll Cardiol 71:2092–2102
Vergallo R, Papafaklis MI, Yonetsu T et al (2014) Endothelial shear stress and coronary plaque characteristics in humans: combined frequency-domain optical coherence tomography and computational fluid dynamics study. Circ Cardiovasc Imaging 7:905–911
Yamamoto E, Siasos G, Zaromytidou M et al (2017) Low endothelial shear stress predicts evolution to high-risk coronary plaque phenotype in the future: a serial optical coherence tomography and computational fluid dynamics study. Circ Cardiovasc Interv. https://doi.org/10.1161/CIRCINTERVENTIONS.117.005455
Milanese G, Silva M, Ledda RE et al (2020) Validity of epicardial fat volume as biomarker of coronary artery disease in symptomatic individuals: results from the ALTER-BIO registry. Int J Cardiol 314:20–24
Nappi C, Ponsiglione A, Acampa W et al (2019) Relationship between epicardial adipose tissue and coronary vascular function in patients with suspected coronary artery disease and normal myocardial perfusion imaging. Eur Heart J Cardiovasc Imaging 20:1379–1387
Fearon WF, Balsam LB, Farouque HM et al (2003) Novel index for invasively assessing the coronary microcirculation. Circulation 107:3129–3132
Lee BK, Lim HS, Fearon WF et al (2015) Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation 131:1054–1060
Kobayashi Y, Lee JM, Fearon WF et al (2017) Three-vessel assessment of coronary microvascular dysfunction in patients with clinical suspicion of ischemia: prospective observational study with the index of microcirculatory resistance. Circ Cardiovasc Interv. https://doi.org/10.1161/CIRCINTERVENTIONS.117.005445
Echavarria-Pinto M, van de Hoef TP, Nijjer S et al (2017) Influence of the amount of myocardium subtended to a coronary stenosis on the index of microcirculatory resistance. Implications for the invasive assessment of microcirculatory function in ischaemic heart disease. EuroIntervention 13:944–952
Murai T, Lee T, Yonetsu T et al (2013) Variability of microcirculatory resistance index and its relationship with fractional flow reserve in patients with intermediate coronary artery lesions. Circ J 77:1769–1776
Sugiyama T, Kanaji Y, Hoshino M et al (2020) Determinants of pericoronary adipose tissue attenuation on computed tomography angiography in coronary artery disease. J Am Heart Assoc. https://doi.org/10.1161/JAHA.120.016202
Funding
This study has received funding by an unrestricted research grant from St. Jude Medical (Abbott Vascular) (Santa Clara, CA, USA). The company had no role in study design, conduct, data analysis, or manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Tsunekazu Kakuta.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Dr. Bon-Kwon Koo received an institutional research grant from St. Jude Medical (Abbott Vascular) and Philips Volcano. Dr. Joo Myung Lee received a research grant from St. Jude Medical (Abbott Vascular) and Philips Volcano. All other authors declare that there is no conflict of interest relevant to the submitted work.
Statistics and biometry
One of the authors has significant statistical expertise.
Dr. Rikuta Hamaya kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
The present study is the substudy of the multicenter study CCTA-FFR Registry for Risk Prediction, Clinical Trial Registration Information: NCT04037163, and the study population was derived from the institutional CCTA registry of Tsuchiura Kyodo General Hospital, one of the cardiac centers that participated in the aforementioned international multicenter registry. Some study subjects have been previously reported in J Cardiovasc Comput Tomogr. 2020 Feb 6:S1934-5925(19)30733-6.
Methodology
• retrospective
• cross-sectional multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 29 kb)
Rights and permissions
About this article
Cite this article
Hoshino, M., Yang, S., Sugiyama, T. et al. Characteristic findings of microvascular dysfunction on coronary computed tomography angiography in patients with intermediate coronary stenosis. Eur Radiol 31, 9198–9210 (2021). https://doi.org/10.1007/s00330-021-07909-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07909-7