Abstract
Objectives
There are growing concerns regarding radiation exposure in medical workers who perform interventional fluoroscopy procedures. Owing to the nature of certain interventional procedures, workers may be subjected to partial-body radiation exposure that is high enough to cause local damage. We aimed to investigate the level of radiation exposure in interventional radiologists in South Korea by performing cytogenetic biodosimetry, particularly focusing on partial-body exposure.
Methods
Interventional radiologists (n = 52) completed a questionnaire, providing information about their work history and practices. Blood samples were collected and processed for a dicentric chromosome assay. We determined Papworth’s U-value to assess the conformity of dicentrics with the Poisson distribution to estimate the partial-body exposures of the radiologists.
Results
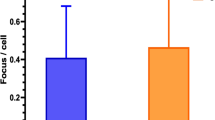
Radiologists had a higher number of dicentrics than the normal population and industrial radiographers. Indeed, subjects with a U-value of > 1.96, an indicator of heterogeneous exposure, were observed more frequently; 4.67 ± 0.81% of their body was irradiated at an average dose of 4.64 ± 0.67 Gy. Logistic regression analysis revealed that the total duration of all interventional procedures per week was associated with partial-body exposure levels.
Conclusions
Our findings suggest that interventional radiologists had greater chromosomal damages than those in other occupational groups, and their partial-body exposure levels might be high enough to cause local damage. Use of special dosimeters to monitor partial-body exposure, as well as restricting the time and frequency of interventional procedures, could help reduce occupational radiation exposure.
Key Points
• Interventional radiologists had a higher number of dicentrics than the normal population and industrial radiographers.
• The level of partial-body exposure of interventional radiologists might be high enough to cause occupational local damage such as a skin cancer in fingers.
• Restricting the duration and frequency of interventional procedures might be helpful in reducing occupational radiation exposure.


Similar content being viewed by others
Abbreviations
- DCA:
-
Dicentric chromosome analysis
- NDT:
-
Non-destructive testing
References
Miller DL (2008) Overview of contemporary interventional fluoroscopy procedures. Health Phys 95:638–644
Miller DL, Balter S, Schueler BA, Wagner LK, Strauss KJ, Vano E (2010) Clinical radiation management for fluoroscopically guided interventional procedures. Radiology 257:321–332
ICRP (2018) Occupational radiological protection in interventional procedures. ICRP Publication 139. Ann ICRP 47:1–118
Measurements NCoRPa (2010) Radiation dose management for fluoroscopically-guided interventional medical procedures. NCRP Report No 168. National Council on Radiation Protection and Measurements, Bethesda, Maryland
Padovani R, Le Heron J, Cruz-Suarez R et al (2011) International project on individual monitoring and radiation exposure levels in interventional cardiology. Radiat Prot Dosimetry 144:437–441
Zakeri F, Hirobe T (2010) A cytogenetic approach to the effects of low levels of ionizing radiations on occupationally exposed individuals. Eur J Radiol 73:191–195
Wiper A, Katira R, Roberts DH (2005) Images in cardiology. Interventional cardiology: it’s a hairy business. Heart 91:1432
Ciraj-Bjelac O, Rehani M, Minamoto A, Sim KH, Liew HB, Vano E (2012) Radiation-induced eye lens changes and risk for cataract in interventional cardiology. Cardiology 123:168–171
Jacob S, Boveda S, Bar O et al (2013) Interventional cardiologists and risk of radiation-induced cataract: results of a French multicenter observational study. Int J Cardiol 167:1843–1847
Roguin A, Goldstein J, Bar O, Goldstein JA (2013) Brain and neck tumors among physicians performing interventional procedures. Am J Cardiol 111:1368–1372
Smilowitz NR, Balter S, Weisz G (2013) Occupational hazards of interventional cardiology. Cardiovasc Revasc Med 14:223–228
Yoshinaga S, Mabuchi K, Sigurdson AJ, Doody MM, Ron E (2004) Cancer risks among radiologists and radiologic technologists: review of epidemiologic studies. Radiology 233:313–321
ICRP (2000) Avoidance of radiation injuries from medical interventional procedures. ICRP Publication 85. Ann ICRP 30:1–67
Sanchez RM, Vano E, Fernandez JM et al (2012) Staff doses in interventional radiology: a national survey. J Vasc Interv Radiol 23:1496–1501
Montoro A, Rodriguez P, Almonacid M et al (2005) Biological dosimetry in a group of radiologists by the analysis of dicentrics and translocations. Radiat Res 164:612–617
Bera G, Gellie G, Jamet E, Entine F, Michel X (2018) Eye lens radiation exposure of workers during medical interventional procedures and surgery. Radiat Prot Dosimetry 182:323–328
IAEA (2011) Cytogenetic dosimetry: applications in preparedness for and response to radiation emergencies. EPR-biodosimetry, IAEA, Vienna
Jang S, Lee JK, Cho M, Yang SS, Kim SH, Kim WT (2016) Consecutive results of blood cell count and retrospective biodosimetry: useful tools of health protection regulation for radiation workers. Occup Environ Med 73:694–700
Xu XS, Zhang LA, Sun QF, Qin YC, Yu NL (2018) Estimation of the occupational exposure dose for medical diagnostic X-ray workers in Jiangsu, China, using a retrospective dosimetry method. J Radiat Res 59:141–148
Salassidis K, Schmid E, Peter RU, Braselmann H, Bauchinger M (1994) Dicentric and translocation analysis for retrospective dose estimation in humans exposed to ionising radiation during the Chernobyl nuclear power plant accident. Mutat Res 311:39–48
Ko S, Chung HH, Cho SB et al (2017) Occupational radiation exposure and its health effects on interventional medical workers: study protocol for a prospective cohort study. BMJ Open 7:e018333
Seo S, Lim WY, Lee DN et al (2018) Assessing the health effects associated with occupational radiation exposure in Korean radiation workers: protocol for a prospective cohort study. BMJ Open 8:e017359
Lee Y, Seo S, Jin YW, Jang S (2020) Assessment of working environment and personal dosimeter-wearing compliance of industrial radiographers based on chromosome aberration frequencies. J Radiol Prot 40:151–164
Ainsbury EA, Lloyd DC (2010) Dose estimation software for radiation biodosimetry. Health Phys 98:290–295
Lee Y, Jin YW, Wilkins RC, Jang S (2019) Validation of the dicentric chromosome assay for radiation biological dosimetry in South Korea. J Radiat Res 60:555–563
Dolphin GW (1969) Biological dosimetry with particular reference to chromosome aberration analysis. A review of methodsHandling of Radiation Accidents (Proc Int Symp Vienna, 1969). IAEA, Vienna, pp 215–224
Zakeri F, Hirobe T, Akbari Noghabi K (2010) Biological effects of low-dose ionizing radiation exposure on interventional cardiologists. Occup Med (Lond) 60:464–469
Andreassi MG, Cioppa A, Botto N et al (2005) Somatic DNA damage in interventional cardiologists: a case-control study. FASEB J 19:998–999
Foti C, Padovani R, Trianni A et al (2008) Staff dosimetry in interventional cardiology: survey on methods and level of exposure. Radiat Prot Dosimetry 129:100–103
Hausler U, Czarwinski R, Brix G (2009) Radiation exposure of medical staff from interventional x-ray procedures: a multicentre study. Eur Radiol 19:2000–2008
Jang S, Jin YW, Lee WJ (2020) Estimating occupational radiation exposure using cytogenetic dosimetry in an interventional radiologist with skin cancer: a case report. J Vasc Interv Radiol 31:1960–1963
Miller DL, Vano E, Bartal G et al (2010) Occupational radiation protection in interventional radiology: a joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Cardiovasc Intervent Radiol 33:230–239
Bi J, Dai H, Feng J et al (2019) Rapid and high-throughput detection of peripheral blood chromosome aberrations in radiation workers. Dose Response 17:1559325819840852
Romm H, Ainsbury E, Barnard S et al (2013) Automatic scoring of dicentric chromosomes as a tool in large scale radiation accidents. Mutat Res 756:174–183
Acknowledgements
We are grateful to Ms. Su San Yang and Yang Hee Lee for their technical support during this study. We thank Dr. Ainsbury in Public Health England, UK, for kindly providing the Dose Estimate program.
Funding
This work was supported by the Korea Ministry of Health and Welfare and Center for Disease Control and Prevention (grant no. 2017E3600600) and the Nuclear Safety and Security Commission Republic of Korea (grant no. 1803014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Seongjae Jang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Comparison groups (normal population and industrial radiographers) have been previously reported in Jang et al (2016) and Lee et al (2020).
Jang S, Lee JK, Cho M, Yang SS, Kim SH, Kim WT (2016) Consecutive results of blood cell count and retrospective biodosimetry: useful tools of health protection regulation for radiation workers. Occup Environ Med 73:694-700
Lee Y, Seo S, Jin YW, Jang S (2020) Assessment of working environment and personal dosimeter-wearing compliance of industrial radiographers based on chromosome aberration frequencies. J Radiol Prot 40:151-164
The subjects were used to compare their chromosomal damages with those in interventional radiologists.
Methodology
• retrospective
• cross-sectional study
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, Y., Lee, W.J., Jin, Y.W. et al. Interventional radiologists have a higher rate of chromosomal damage due to occupational radiation exposure: a dicentric chromosome assay. Eur Radiol 31, 8256–8263 (2021). https://doi.org/10.1007/s00330-021-07883-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07883-0