Abstract
Objectives
Minimum caseload standards for professionals examining breast screening mammograms vary from 480 (US) to 5000 (Europe). We measured the relationship between the number of women’s mammograms examined per year and reader performance.
Methods
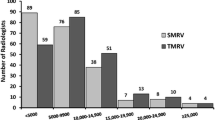
We extracted routine records from the English NHS Breast Screening Programme for readers examining between 1000 and 45,000 mammograms between April 2014 and March 2017. We measured the relationship between the volume of cases read and screening performance (cancer detection rate, recall rate, positive predictive value of recall (PPV) and discrepant cancers) using linear logistic regression. We also examined the effect of reader occupational group on performance.
Results
In total, 759 eligible mammography readers (445 consultant radiologists, 235 radiography advanced practitioners, 79 consultant radiographers) examined 6.1 million women’s mammograms during the study period. PPV increased from 12.9 to 14.4 to 17.0% for readers examining 2000, 5000 and 10000 cases per year respectively. This was driven by decreases in recall rates from 5.8 to 5.3 to 4.5 with increasing volume read, and no change in cancer detection rate (from 7.6 to 7.6 to 7.7). There was no difference in cancer detection rate with reader occupational group. Consultant radiographers had higher recall rate and lower PPV compared to radiologists (OR 1.105, p = 0.012; OR 0.874, p = 0.002, unadjusted).
Conclusion
Positive predictive value of screening increases with the total volume of cases examined per reader, through decreases in numbers of cases recalled with no concurrent change in numbers of cancers detected.
Key Points
• In the English Breast Screening Programme, readers who examined a larger number of cases per year had a higher positive predictive value, because they recalled fewer women for further tests but detected the same number of cancers.
• Reader type did not affect cancer detection rate, but consultant radiographers had a higher recall rate and lower positive predictive value than consultant radiologists, although this was not adjusted for length of experience.

Similar content being viewed by others
Abbreviations
- BSIS:
-
Breast Screening Information System
- CDR:
-
Cancer detection rate
- IQR:
-
Inter quartile range
- KC62:
-
National Health Service Breast Screening Programme Central Return Data Set
- NHSBSP:
-
National Health Service Breast Screening Programme
- OR:
-
Odds ratio
- PPV:
-
Positive predictive value
References
Mammography Quality Standards Act Regulations. U.S. Food & Drug Administration. https://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/Regulations/ucm110906.htm. Updated November 29, 2017. Accessed June 2020
BreastScreen Australia (2015) National accreditation standards.http://cancerscreening.gov.au/internet/screening/publishing.nsf/Content/br-accreditation/$File/standards.pdf. Accessed June 2020
Perry N, Broeders MJ, de Wolf C, Törnberg S, Holland R, von Karsa L (2006) European guidelines for quality assurance in breast cancer screening and diagnosis, 4th edn. Office for Official Publications of the European Communities, Luxembourg
Quality Assurance Guidelines for Breast Cancer Screening Radiology (2005) NHS Cancer Screening Programmes (NHSBSP Publication No 59)
Gur D, Bandos AI, Cohen CS et al (2008) The “laboratory effect” : comparing radiologists’ performance and variability during prospective clinical and laboratory mammography interpretation. Radiology 249(1):47–53
Buist DS, Anderson ML, Haneuse SJ et al (2011) Influence of annual interpretive volume on screening mammography performance in the United States. Radiology 259(1):72–84
Smith-Bindman R, Chu P, Miglioretti DL et al (2005) Physician predictors of mammographic accuracy. J Natl Cancer Inst 97(5):358–367
Théberge I, Chang SL, Vandal N et al (2014) Radiologist interpretive volume and breast cancer screening accuracy in a Canadian organized screening program. J Natl Cancer Inst 106(3):djt461
Cornford E, Reed J, Murphy A, Bennett R, Evans A (2011) Optimal screening mammography reading volumes; evidence from real life in the East Midlands region of the NHS Breast Screening Programme. Clin Radiol 66(2):103–107
Duncan KA, Scott NW (2011) Is film-reading performance related to the number of films read? The Scottish experience. Clin Radiol 66(2):99–102
Hoff SR, Myklebust TA, Lee CI, Hofvind S (2019) Influence of mammography volume on radiologists’ performance: results from BreastScreen Norway. Radiology 292:289–296
Department of Health (2000) The NHS Cancer plan: a plan for investment, a plan for reform. Department of Health, London Available via https://webarchive.nationalarchives.gov.uk/20130222181549/; http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4014513.pdf. Accessed 22nd November 2020
Public Health England (2016) Guidance on who can undertake arbitration. Public Health England, London Available via https://www.gov.uk/government/publications/breast-screening-arbitration-guidance. Accessed 22nd November 2020
Moss SM, Blanks RG, Bennett RL (2005) Is radiologists’ volume of mammography reading related to accuracy? A critical review of the literature. Clin Radiol 60:623–626
Elmore JG, Jackson SL, Abraham L et al (2009) Variability in interpretive performance at screening mammography and radiologists’ characteristics associated with accuracy. Radiology 253:641–651
Buist DS, Anderson ML, Smith RA et al (2014) Effect of radiologists’ diagnostic work-up volume on interpretive performance. Radiology 273:351–364
Rawashdeh M, Lee W, Bourne R et al (2013) Markers of good performance in mammography depend on number of annual readings. Radiology 269:61–67
van den Biggelaar FJHM, Nelemans PJ, Flobbe K (2008) Performance of radiographers in mammogram interpretation: a systematic review. Breast 17:87–92
Bennett RL, Sellars SJ, Blanks RG, Moss SM (2012) An observational study to evaluate the performance of units using two radiographers to read screening mammograms. Clin Radiol 67:114–121
Taylor-Phillips S, Wallis MG, Jenkinson D et al (2016) Effect of using the same vs different order for second readings of screening mammograms on rates of breast cancer detection. JAMA 315(18):1956–1965
Burnside ES, Park JM, Fine JP, Sisney GA (2005) The use of batch reading to improve the performance of screening mammography. AJR Am J Roentgenol 185(3):790–796
Brennan PC, Ganesan A, Eckstein MP et al (2019) Benefits of independent double reading in digital mammography: a theoretical evaluation of all possible pairing methodologies. Acad Radiol 26(6):717–723
Blanks RG, Given-Wilson RM, Cohen SL, Patnick J, Alison RJ, Wallis MG (2019) An analysis of 11.3 million screening tests examining the association between recall and cancer detection rates in th English NHS breast cancer screening programme. Eur Radiol 29(7):3812–3819
Burnside ES, Vulkan D, Blanks RG, Duffy SW (2018) Association between Screening Mammography Recall Rate and Interval Cancers in the UK Breast Cancer Service Screening Program: A Cohort Study. Radiology 288(1):47–54
Acknowledgements
The authors acknowledge Public Health England.
Funding
The analysis for this study was undertaken by Public Health England staff as part of the quality assurance function of the NHS Breast Screening Programme. STP is funded by the NIHR through a career development fellowship (NIHR-CDF-2016-09-018). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Eleanor Cornford
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Shan Cheung and Sian Taylor-Phillips kindly provided statistical advice for this manuscript. Both of these authors have significant statistical expertise.
Informed consent
Written informed consent was not required for this study because this analysis of de-identified data is classified as audit as part of the quality assurance function of the breast screening programme by Public Health England
Ethical approval
Institutional Review Board approval was not required because this analysis of de-identified data is classified as an audit as part of the quality assurance function of the breast screening programme by Public Health England and therefore did not require ethical committee review.
Methodology
• prospective
• observational
• national
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 213 kb)
Rights and permissions
About this article
Cite this article
Cornford, E., Cheung, S., Press, M. et al. Optimum screening mammography reading volumes: evidence from the NHS Breast Screening Programme. Eur Radiol 31, 6909–6915 (2021). https://doi.org/10.1007/s00330-021-07754-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07754-8