Abstract
Objectives
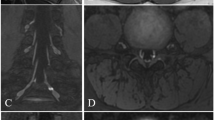
No routine imaging technology allows reliable visualization of nerve rootlets inside the spinal canal with positive contrast. The stronger MR signal at 7 T, with optimized protocols, may offer a solution. The purpose was to evaluate the potential of 3D Dual-Echo Steady-State (DESS) MR imaging of the cervical spine at 3 and 7 T in assessing the micro-anatomy of the nerve rootlets.
Materials/methods
This prospective study was approved by the local ethics committee. Twenty-one patients, clinically referred to cervical-spine MRI, underwent additional MR exams at 3 T and 7 T, each of which consisted of a single 3D-DESS series with equal acquisition times. Artifacts, visualization quality, and number of identified rootlets (C2 to C8) were rated by two musculoskeletal radiologists. Results were compared by Wilcoxon tests. Interobserver reliability was assessed using weighted κ statistics and intraclass correlation coefficient (ICC).
Results
Intraspinal rootlets could successfully be visualized at both field strengths. Rating differences for artifacts and quality of rootlet depiction were not significant for the two field strengths. The mean number of identified rootlets was larger for 7-T than for 3-T MR for every assessed nerve; however, this difference was not statistically significant using the Bonferroni correction (p values ranging from 0.002 to 0.53). Interobserver agreement was substantial to almost perfect (weighted κ values of 0.69 and 0.82). The ICC for the number of identified rootlets was 0.80.
Conclusion
Non-invasive 3D-DESS MR-imaging at 3 and 7 T has the potential to provide precise assessments of the micro-anatomy of intraspinal cervical nerve roots.
Key Points
• Cervical rootlets can be successfully visualized with positive contrast using 3D-DESS MR-imaging.
• 3D-DESS MR-imaging at 3 and 7 T provides precise assessments of the micro-anatomy of cervical nerves.
• The mean number of identified cervical rootlets using 3D-DESS was larger for 7 T than for 3 T MR; however, this difference was not statistically significant.





Similar content being viewed by others
Abbreviations
- CSF:
-
Cerebrospinal fluid
- DESS:
-
Dual echo steady state
- ICC:
-
Intraclass correlation coefficient
- MIP:
-
Maximum intensity projection
- MPR:
-
Multiplanar reformat
- SAR:
-
Specific absorption rate
- STIR :
-
Short tau inversion recovery
- TE:
-
Echo time
- TR:
-
Repetition time
References
Leijnse JN, D’Herde K (2016) Revisiting the segmental organization of the human spinal cord. J Anat 229(3):384–393
Alleyne CH, Cawley CM, Barrow DL, Bonner GD (1998) Microsurgical anatomy of the dorsal cervical nerve roots and the cervical dorsal root ganglion/ventral root complexes. Surg Neurol 50(3):213–218
Karatas A, Caglar S, Savas A, Elhan A, Erdogan A (2005) Microsurgical anatomy of the dorsal cervical rootlets and dorsal root entry zones. Acta Neurochir (Wien) 147(2):195–199 discussion 199
Carette S, Fehlings MG (2005) Clinical practice. Cervical radiculopathy. N Engl J Med 353(4):392–399
Caridi JM, Pumberger M, Hughes AP (2011) Cervical radiculopathy: a review. HSS J 7(3):265–272
Expert Panel on Neurological Imaging, Mc-Donald MA, Kirsch CFE, Amin BY et al (2019) ACR Appropriateness Criteria® cervical neck pain or cervical radiculopathy. J Am Coll Radiol 16(5S):S57–S76
Tharin BD, Kini JA, York GE, Ritter JL (2014) Brachial plexopathy: a review of traumatic and nontraumatic causes. AJR Am J Roentgenol 202(1):W67–W75
Yoshikawa T, Hayashi N, Yamamoto S et al (2006) Brachial plexus injury: clinical manifestations, conventional imaging findings, and the latest imaging techniques. Radiographics. 26(Suppl 1):S133–S143
Expert Panel on Neurologic Imaging, Bykowski J, Aulino JM, Berger KL et al (2017) ACR Appropriateness Criteria® Plexopathy. J Am Coll Radiol 14(5S):S225–S233
Expert Panel on Neurological Imaging and Musculoskeletal Imaging, Beckmann NM, West OC, Nunez D et al (2019) ACR Appropriateness Criteria® suspected spine trauma. J Am Coll Radiol 16(5S):S264–S285
Wade RG, Takwoingi Y, Wormald JCR et al (2019) MRI for detecting root avulsions in traumatic adult brachial plexus injuries: a systematic review and meta-analysis of diagnostic accuracy. Radiology. 293(1):125–133
Chhabra A, Thawait GK, Soldatos T et al (2013) High-resolution 3 T MR neurography of the brachial plexus and its branches, with emphasis on 3D imaging. AJNR Am J Neuroradiol 34(3):486–497
Yang J, Qin B, Fu G et al (2014) Modified pathological classification of brachial plexus root injury and its MR imaging characteristics. J Reconstr Microsurg 30(3):171–178
Lee JH, Cheng K-L, Choi YJ, Baek JH (2017) High-resolution imaging of neural anatomy and pathology of the neck. Korean J Radiol 18(1):180–193
Barry RL, Vannesjo SJ, By S, Gore JC, Smith SA (2018) Spinal cord MRI at 7T. Neuroimage. 168:437–451
Sigmund EE, Suero GA, Hu C et al (2012) High-resolution human cervical spinal cord imaging at 7 T. NMR Biomed 25(7):891–899
Yoon D, Biswal S, Rutt B, Lutz A, Hargreaves B (2018) Feasibility of 7T MRI for imaging fascicular structures of peripheral nerves. Muscle Nerve 57(3):494–498
Hardy PA, Recht MP, Piraino D, Thomasson D (1996) Optimization of a dual echo in the steady state (DESS) free-precession sequence for imaging cartilage. J Magn Reson Imaging 6(2):329–335
Peterfy CG, Schneider E, Nevitt M (2008) The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage 16(12):1433–1441
Chaudhari AS, Black MS, Eijgenraam S et al (2018) 5-Minute knee MRI for simultaneous morphometry and T2 relaxometry of cartilage and meniscus and for semi-quantitative radiological assessment using double-echo in steady-state at 3T. J Magn Reson Imaging 47(5):1328–1341
Schleich C, Hesper T, Hosalkar HS et al (2017) 3D double-echo steady-state sequence assessment of hip joint cartilage and labrum at 3 Tesla: comparative analysis of magnetic resonance imaging and intraoperative data. Eur Radiol 27(10):4360–4371
Qin Y, Zhang J, Li P, Wang Y (2011) 3D double-echo steady-state with water excitation MR imaging of the intraparotid facial nerve at 1.5T: a pilot study. AJNR Am J Neuroradiol 32(7):1167–1172
Shin AY, Spinner RJ, Steinmann SP, Bishop AT (2005) Adult traumatic brachial plexus injuries. J Am Acad Orthop Surg 13(6):382
Terzis JK, Kostopoulos VK (2007) The surgical treatment of brachial plexus injuries in adults. Plast Reconstr Surg 119(4):73e–92e
Rankine JJ (2004) Adult traumatic brachial plexus injury. Clin Radiol 59(9):767–774
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Daniel Nanz.
Conflict of interest
Balgrist University Hospital of Zurich as well as Balgrist Campus AG each has a research agreement with Siemens Healthcare AG.
Statistics and biometry
One of the authors has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Galley, J., Sutter, R., Germann, C. et al. High-resolution in vivo MR imaging of intraspinal cervical nerve rootlets at 3 and 7 Tesla. Eur Radiol 31, 4625–4633 (2021). https://doi.org/10.1007/s00330-020-07557-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07557-3