Abstract
Objectives
A machine learning model was developed to evaluate the severity of aortic coarctation (CoA) in infants based on anatomical features measured on CTA.
Methods
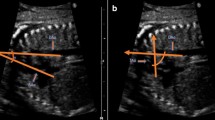
In total, 239 infant patients undergoing both thorax CTA and echocardiography were retrospectively reviewed. The patients were assigned to either mild or severe CoA group based on their pressure gradient on echocardiography. They were further divided into patent ductus arteriosus (PDA) and non-PDA groups. The anatomical features were measured on double-oblique multiplanar reconstructed CTA images. Then, the optimal features were identified by using the Boruta algorithm. Subsequently, the coarctation severity was classified using linear discriminant analysis (LDA). We further investigated the relationship between the anatomical features and re-coarctation using Cox regression.
Results
Four anatomical features showed significant differences between the mild and severe CoA groups, including the smallest aortic cross-sectional area indexed to body surface area (p < 0.001), the narrowest aortic diameter (CoA diameter) indexed to height (p < 0.001), the diameter of the descending aorta at the diaphragmatic level (p < 0.001) and weight (p = 0.005). With these features, accuracy of 88.6% and 90.2%, sensitivity of 65.0% and 72.1%, and specificity of 92.9% and 100% were obtained for classifying the CoA severity in the non-PDA and PDA groups, respectively. Moreover, CoA diameter indexed to weight was associated with the risk of re-coarctation.
Conclusions
CoA severity can be evaluated by using LDA with anatomical features. When quantifying the severity of CoA and risk of re-coarctation, both anatomical alternations at the CoA site and the growth of the patients need to be considered.
Key Points
• CTA is routinely ordered for infants with coarctation of the aorta; however, whether anatomical variations observed with CTA could be used to assess the severity of CoA remains unknown.
• Using the diameter and area of the coarctation site adjusted to body growth as features, the LDA model achieved an accuracy of 88.6% and 90.2% in differentiating between the mild and severe CoA patients in the non-PDA group and PDA group, respectively.
• The narrowest aortic diameter (CoA diameter) indexed to weight has a hazard ratio of 10.29 for re-coarctation.






Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the receiver operator characteristic curve
- BSA:
-
Body surface area
- CoA:
-
Aortic coarctation
- CoA diameter:
-
The narrowest aortic diameter
- CoA diameter/age:
-
CoA diameter indexed to age
- CoA diameter/height:
-
CoA diameter indexed to height
- CoA diameter/weight:
-
CoA diameter indexed to weight
- CoA/DAo ratio:
-
CoA diameter indexed to the diameter of the descending aorta at the diaphragmatic level
- Coarctation area/BSA:
-
The smallest aortic cross-sectional area indexed to body surface area
- CTA:
-
Computed tomography angiography
- LDA:
-
Linear discriminant analysis
- PDA:
-
Patent ductus arteriosus
- PH:
-
Pulmonary hypertension
- VSD:
-
Ventricular septal defect
References
Nance JW, Ringel RE, Fishman EK (2016) Coarctation of the aorta in adolescents and adults: a review of clinical features and CT imaging. J Cardiovasc Comput Tomogr 10:1–12
Bigdelian H, Sedighi M (2016) Repair of aortic coarctation in infancy: a 10-year clinical experience. Asian Cardiovasc Thorac Ann 24:417–421
Baumgartner H, Bonhoeffer P, De Groot NMS et al (2010) ESC guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J 31:2915–2957
Erbel R, Aboyans V, Boileau C et al (2014) 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult: the Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 35:2873–2926
Nielsen JC, Powell AJ, Gauvreau K, Marcus EN, Prakash A, Geva T (2005) Magnetic resonance imaging predictors of coarctation severity. Circulation 111:622–628
Abbruzzese PA, Aidala E (2007) Aortic coarctation: an overview. J Cardiovasc Med 8:123–128
Castaneda AR, Jonas RA, Mayer JE Jr, Hanley FL (1994) Cardiac surgery of the neonate and infant, 1st edn. WB Saunders, Philadelphia
Yang JC-T, Lin M-T, Jaw F-S et al (2015) Trends in the utilization of computed tomography and cardiac catheterization among children with congenital heart disease. J Formos Med Assoc 114:1061–1068
Muzzarelli S, Meadows AK, Ordovas KG et al (2011) Prediction of hemodynamic severity of coarctation by magnetic resonance imaging. Am J Cardiol 108:1335–1340
Pinzon JL, Burrows PE, Benson LN et al (1991) Repair of coarctation of the aorta in children: postoperative morphology. Radiology 180:199–203
Gutberlet M, Hosten N, Vogel M et al (2001) Quantification of morphologic and hemodynamic severity of coarctation of the aorta by magnetic resonance imaging. Cardiol Young 11:512–520
Nie P, Wang X, Cheng Z et al (2012) The value of low-dose prospective ECG-gated dual-source CT angiography in the diagnosis of coarctation of the aorta in infants and children. Clin Radiol 67:738–745
Riquelme C, Laissy J-P, Menegazzo D et al (1999) MR imaging of coarctation of the aorta and its postoperative complications in adults: assessment with spin-echo and cine-MR imaging. Magn Reson Imaging 17:37–46
Takeda A, Murakami T (2008) Morphometric analysis of aortic coarctation: determination of the target vessel diameter required to relieve the pressure gradient. Circ J 72:1993–1997
Lu CW, Wang JK, Chang CI et al (2006) Noninvasive diagnosis of aortic coarctation in neonates with patent ductus arteriosus. J Pediatr 148:217–221
Dehaki MG, Ghavidel A, Givtaj N, Omrani G, Salehi S (2010) Recurrence rate of different techniques for repair of coarctation of aorta: a 10 years experience. Ann Pediatr Cardiol 3:123–126
Walhout RJ, Lekkerkerker JC, Oron GH, Hitchcock FJ, Meijboom EJ, Bennink GB (2003) Comparison of polytetrafluoroethylene patch aortoplasty and end-to-end anastomosis for coarctation of the aorta. J Thorac Cardiovasc Surg 126:521–528
Dodge-Khatami A, Backer CL, Mavroudis C (2000) Risk factors for recoarctation and results of reoperation: a 40-year review. J Card Surg 15:369–377
Bacha EA, Almodovar M, Wessel DL et al (2001) Surgery for coarctation of the aorta in infants weighing less than 2 kg. Ann Thorac Surg 71:1260–1264
Jia Q, Zhuang J, Jiang J, Li J, Huang M, Liang C (2017) Image quality of ct angiography using model-based iterative reconstruction in infants with congenital heart disease: comparison with filtered back projection and hybrid iterative reconstruction. Eur J Radiol 86:190–197
Huang M-P, Liang C-H, Zhao Z-J et al (2011) Evaluation of image quality and radiation dose at prospective ECG-triggered axial 256-slice multi-detector CT in infants with congenital heart disease. Pediatr Radiol 41:858–866
Blanke P, Schoepf UJ, Leipsic JA (2013) CT in transcatheter aortic valve replacement. Radiology 269:650–669
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317:1098
Kursa MB, Jankowski A, Rudnicki WR (2010) Boruta - a system for feature selection. Fund Inform 101:271–285
Kursa MB, Rudnicki WR (2018) Boruta: wrapper algorithm for all relevant feature selection. University of Warsaw, Warsaw Available via https://cran.r-project.org/src/contrib/Archive/Boruta/Boruta_5.3.0.tar.gz. Accessed 19 Mar 2018
Ye J, Li Q (2005) A two-stage linear discriminant analysis via QR-decomposition. IEEE Trans Pattern Anal Mach Intell 27:929–941
Kuhn M (2015) Caret: classification and regression training. Astrophysics Source Code Library. Available via https://cran.r-project.org/src/contrib/Archive/caret/caret_6.0-79.tar.gz. Accessed 29 Mar 2018
Betancur J, Rubeaux M, Fuchs TA et al (2017) Automatic valve plane localization in myocardial perfusion SPECT/CT by machine learning: anatomical and clinical validation. J Nucl Med 58:961–967
Marx GR, Allen HD (1986) Accuracy and pitfalls of Doppler evaluation of the pressure gradient in aortic coarctation. J Am Coll Cardiol 7:1379–1385
Mcelhinney DB, Yang S-G, Hogarty AN et al (2001) Recurrent arch obstruction after repair of isolated coarctation of the aorta in neonates and young infants: is low weight a risk factor? J Thorac Cardiovasc Surg 122:883–890
Soslow JH, Kavanaugh-McHugh A, Wang L et al (2013) A clinical prediction model to estimate the risk for coarctation of the aorta in the presence of a patent ductus arteriosus. J Am Soc Echocardiogr 26:1379–1387
Aguilar DC, Raff GW, Tancredi DJ, Griffin IJ (2015) Childhood growth patterns following congenital heart disease. Cardiol Young 25:1044–1053
Costello CL, Gellatly M, Daniel J, Justo RN, Weir K (2015) Growth restriction in infants and young children with congenital heart disease. Congenit Heart Dis 10:447–456
Funding
This study has received funding from the National Key Research and Development Program of China (Grant No. 2017YFA0205202), and partially funded by the National Natural Science Foundation of China (Grant No. U1401255), and Science and Technology Planning Project of Guangdong Province No.2014A020212228.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Liyu Huang, Xidian University.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
This study was approved by the ethics committee of Guangdong General Hospital (Guangdong General Hospital No. GDREC2014109H).
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 593 kb)
Rights and permissions
About this article
Cite this article
Yu, Y., Wang, Y., Yang, M. et al. Evaluating the severity of aortic coarctation in infants using anatomic features measured on CTA. Eur Radiol 31, 1216–1226 (2021). https://doi.org/10.1007/s00330-020-07238-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07238-1