Abstract
Objectives
To assess the longitudinal changes of microvascular function in different myocardial regions after myocardial infarction (MI) using myocardial blood flow derived by dynamic CT perfusion (CTP-MBF), and compare CTP-MBF with the results of cardiac magnetic resonance (CMR) and histopathology.
Methods
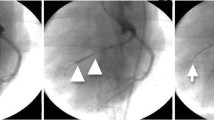
The CTP scanning was performed in a MI porcine model 1 day (n = 15), 7 days (n = 10), and 3 months (n = 5) following induction surgery. CTP-MBF was measured in the infarcted myocardium, penumbra, and remote myocardium, respectively. CMR perfusion and histopathology were performed for validation.
Results
From baseline to follow-up scans, CTP-MBF presented a stepwise increase in the infarcted myocardium (68.51 ± 11.04 vs. 86.73 ± 13.32 vs. 109.53 ± 26.64 ml/100 ml/min, p = 0.001) and the penumbra (104.92 ± 29.29 vs. 120.32 ± 24.74 vs. 183.01 ± 57.98 ml/100 ml/min, p = 0.008), but not in the remote myocardium (150.05 ± 35.70 vs. 166.66 ± 38.17 vs. 195.36 ± 49.64 ml/100 ml/min, p = 0.120). The CTP-MBF correlated with max slope (r = 0.584, p < 0.001), max signal intensity (r = 0.357, p < 0.001), and time to max (r = − 0.378, p < 0.001) by CMR perfusion. Moreover, CTP-MBF defined the infarcted myocardium on triphenyl tetrazolium chloride staining (AUC: 0.810, p < 0.001) and correlated with microvascular density on CD31 staining (r = 0.561, p = 0.002).
Conclusion
CTP-MBF could quantify the longitudinal changes of microvascular function in different regions of the post-MI myocardium, which demonstrates good agreement with contemporary CMR and histopathological findings.
Key Points
• The CT perfusion–based myocardial blood flow (CTP-MBF) could quantify the microvascular impairment in different myocardial regions after myocardial infarction (MI) and track its recovery over time.
• The assessment of CTP-MBF is in good agreement with contemporary cardiac MRI and histopathological findings, which potentially facilitates a rapid approach for pathophysiological insights following MI.





Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery disease
- CMR:
-
Cardiac magnetic resonance
- CTA:
-
CT angiography
- CTP:
-
CT perfusion
- H&E:
-
Hematoxylin-eosin
- LGE:
-
Late gadolinium enhancement
- MBF:
-
Myocardial blood flow
- MI:
-
Myocardial infarction
- ROI:
-
Region of interest
- SI:
-
Signal intensity
- SPECT:
-
Single-photon emission computed tomography
- TTC:
-
Triphenyl tetrazolium chloride
- TTM:
-
Time to maximum signal intensity
References
Symons R, Pontone G, Schwitter J et al (2018) Long-term incremental prognostic value of cardiovascular magnetic resonance after ST-segment elevation myocardial infarction: a study of the collaborative registry on CMR in STEMI. JACC Cardiovasc Imaging 11(6):813–825
de Waha S, Patel MR, Granger CB et al (2017) Relationship between microvascular obstruction and adverse events following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: an individual patient data pooled analysis from seven randomized trials. Eur Heart J 38(47):3502–3510
Borlotti A, Jerosch-Herold M, Liu D et al (2019) Acute microvascular impairment post-reperfused STEMI is reversible and has additional clinical predictive value: A CMR OxAMI Study. JACC Cardiovasc Imaging 12(9):1783–1793
Bethke A, Shanmuganathan L, Andersen GØ et al (2019) Microvascular perfusion in infarcted and remote myocardium after successful primary PCI: angiographic and CMR findings. Eur Radiol 29(2):941–950
Danad I, Szymonifka J, Twisk JWR et al (2017) Diagnostic performance of cardiac imaging methods to diagnose ischaemia-causing coronary artery disease when directly compared with fractional flow reserve as a reference standard: a meta-analysis. Eur Heart J 38(13):991–998
Gupta A, Taqueti VR, van de Hoef TP et al (2017) Integrated noninvasive physiological assessment of coronary circulatory function and impact on cardiovascular mortality in patients with stable coronary artery disease. Circulation 136(24):2325–2336
Gould KL, Johnson NP, Roby AE et al (2019) Regional, artery-specific thresholds of quantitative myocardial perfusion by PET associated with reduced myocardial infarction and death after revascularization in stable coronary artery disease. J Nucl Med 60(3):410–417
Danad I, Szymonifka J, Schulman-Marcus J, Min JK (2016) Static and dynamic assessment of myocardial perfusion by computed tomography. Eur Heart J Cardiovasc Imaging 17(8):836–844
Takx RAP, Celeng C, Schoepf UJ (2018) CT myocardial perfusion imaging: ready for prime time? Eur Radiol 28(3):1253–1256
Feger S, Rief M, Zimmermann E et al (2015) Patient satisfaction with coronary CT angiography, myocardial CT perfusion, myocardial perfusion MRI, SPECT myocardial perfusion imaging and conventional coronary angiography. Eur Radiol 25(7):2115–2124
Pursnani A, Lee AM, Mayrhofer T et al (2015) Early resting myocardial computed tomography perfusion for the detection of acute coronary syndrome in patients with coronary artery disease. Circ Cardiovasc Imaging 8(3):e002404. https://doi.org/10.1161/CIRCIMAGING.114.002404
Pontone G, Andreini D, Guaricci AI et al (2018) Quantitative vs. qualitative evaluation of static stress computed tomography perfusion to detect haemodynamically significant coronary artery disease. Eur Heart J Cardiovasc Imaging 19(11):1244–1252
Nakamura S, Kitagawa K, Goto Y et al (2019) Incremental prognostic value of myocardial blood flow quantified with stress dynamic computed tomography perfusion imaging. JACC Cardiovasc Imaging 12(7 Pt 2):1379–1387
Chen MY, Rochitte CE, Arbab-Zadeh A et al (2017) Prognostic value of combined CT angiography and myocardial perfusion imaging versus invasive coronary angiography and nuclear stress perfusion imaging in the prediction of major adverse cardiovascular events: the CORE320 multicenter study. Radiology 284(1):55–65
Van Rosendael AR, Dimitriu-Leen AC, de Graaf MA et al (2017) Impact of computed tomography myocardial perfusion following computed tomography coronary angiography on downstream referral for invasive coronary angiography, revascularization and, outcome at 12 months. Eur Heart J Cardiovasc Imaging 18(9):969–977
Tanabe Y, Kido T, Uetani T et al (2016) Differentiation of myocardial ischemia and infarction assessed by dynamic computed tomography perfusion imaging and comparison with cardiac magnetic resonance and single-photon emission computed tomography. Eur Radiol 26(11):3790–3801
Yim NY, Kim YH, Choi S et al (2009) Multidetector-row computed tomographic evaluation of myocardial perfusion in re-perfused chronic myocardial infarction: value of color-coded perfusion map in a porcine model. Int J Cardiovasc Imaging 25(Suppl 1):65–74
Bamberg F, Marcus RP, Becker A et al (2014) Dynamic myocardial CT perfusion imaging for evaluation of myocardial ischemia as determined by MR imaging. JACC Cardiovasc Imaging 7(3):267–277
Kidambi A, Motwani M, Uddin A et al (2017) Myocardial extracellular volume estimation by CMR predicts functional recovery following acute MI. JACC Cardiovasc Imaging 10(9):989–999
Liu D, Borlotti A, Viliani D et al (2017) CMR Native T1 Mapping allows differentiation of reversible versus irreversible myocardial damage in ST-segment-elevation myocardial infarction: an OxAMI study (Oxford Acute Myocardial Infarction). Circ Cardiovasc Imaging 10(8):e005986. https://doi.org/10.1161/CIRCIMAGING.116.005986
Eitel I, Pöss J, Jobs A et al (2015) Left ventricular global function index assessed by cardiovascular magnetic resonance for the prediction of cardiovascular events in ST-elevation myocardial infarction. J Cardiovasc Magn Reson 17:62
Li R, Yang ZG, Wen LY et al (2016) Regional myocardial microvascular dysfunction in cardiac amyloid light-chain amyloidosis: assessment with 3 T cardiovascular magnetic resonance. J Cardiovasc Magn Reson 18:16
van Assen M, Lavra F, Schoepf UJ et al (2019) Iodine quantification based on rest/stress perfusion dual energy CT to differentiate ischemic, infarcted and normal myocardium. Eur J Radiol 112:136–143
Krumm P, Martirosian P, Rath D et al (2016) Signal decay mapping of myocardial edema using dual-contrast fast spin-echo MRI. J Magn Reson Imaging 44(1):186–193
Robbers LF, Delewi R, Nijveldt R et al (2013) Myocardial infarct heterogeneity assessment by late gadolinium enhancement cardiovascular magnetic resonance imaging shows predictive value for ventricular arrhythmia development after acute myocardial infarction. Eur Heart J Cardiovasc Imaging 14(12):1150–1158
Zou J, Fei Q, Xiao H et al (2019) VEGF-A promotes angiogenesis after acute myocardial infarction through increasing ROS production and enhancing ER stress-mediated autophagy. J Cell Physiol 234(10):17690–17703
Robbers LF, Eerenberg ES, Teunissen PF et al (2013) Magnetic resonance imaging-defined areas of microvascular obstruction after acute myocardial infarction represent microvascular destruction and haemorrhage. Eur Heart J 34(30):2346–2353
Bulluck H, Chan MHH, Paradies V et al (2018) Impact of cardioprotective therapies on the edema-based area at risk by CMR in reperfused STEMI. J Am Coll Cardiol 71(24):2856–2858
Meinel FG, De Cecco CN, Schoepf UJ et al (2014) First-arterial-pass dual-energy CT for assessment of myocardial blood supply: do we need rest, stress, and delayed acquisition? Comparison with SPECT. Radiology 270(3):708–716
Vincenti G, Masci PG, Monney P et al (2017) Stress perfusion CMR in patients with known and suspected CAD: prognostic value and optimal ischemic threshold for revascularization. JACC Cardiovasc Imaging 10(5):526–537
Cheng AS, Pegg TJ, Karamitsos TD et al (2007) Cardiovascular magnetic resonance perfusion imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol 49(25):2440–2449
Chiribiri A, Leuzzi S, Conte MR et al (2015) Rest perfusion abnormalities in hypertrophic cardiomyopathy: correlation with myocardial fibrosis and risk factors for sudden cardiac death. Clin Radiol 70(5):495–501
Scherer K, Hammel J, Sellerer T et al (2019) Dynamic quantitative iodine myocardial perfusion imaging with dual-layer CT using a porcine model. Sci Rep 9(1):16046
Poulter R, Wood DA, Starovoytov A, Smith S, Chitsaz M, Mayo J (2019) Development of a porcine model of coronary stenosis using fully percutaneous techniques suitable for performing cardiac computed tomography, CT-perfusion imaging and fractional flow reserve. Heart Lung Circ 28(8):1292–1300
Pelgrim GJ, Duguay TM, Stijnen JM et al (2017) Analysis of myocardial perfusion parameters in an ex-vivo porcine heart model using third generation dual-source CT. J Cardiovasc Comput Tomogr 11(2):141–147
Pelgrim GJ, Das M, van Tuijl S et al (2017) Validation of myocardial perfusion quantification by dynamic CT in an ex-vivo porcine heart model. Int J Cardiovasc Imaging 33(11):1821–1830
Hubbard L, Lipinski J, Ziemer B et al (2018) Comprehensive assessment of coronary artery disease by using first-pass analysis dynamic CT Perfusion: validation in a swine model. Radiology 286(1):93–102
George RT, Jerosch-Herold M, Silva C et al (2007) Quantification of myocardial perfusion using dynamic 64-detector computed tomography. Invest Radiol 42(12):815–822
Bamberg F, Hinkel R, Schwarz F et al (2012) Accuracy of dynamic computed tomography adenosine stress myocardial perfusion imaging in estimating myocardial blood flow at various degrees of coronary artery stenosis using a porcine animal model. Invest Radiol 47(1):71–77
So A, Wisenberg G, Teefy P et al (2018) Functional CT assessment of extravascular contrast distribution volume and myocardial perfusion in acute myocardial infarction. Int J Cardiol 266:15–23
So A, Hsieh J, Li JY, Hadway J, Kong HF, Lee TY (2012) Quantitative myocardial perfusion measurement using CT perfusion: a validation study in a porcine model of reperfused acute myocardial infarction. Int J Cardiovasc Imaging 28(5):1237–1248
Levi J, Eck BL, Fahmi R et al (2019) Calibration-free beam hardening correction for myocardial perfusion imaging using CT. Med Phys 46(4):1648–1662
Li Y, Speidel MA, Francois CJ, Chen GH (2017) Radiation dose reduction in CT myocardial perfusion imaging using SMART-RECON. IEEE Trans Med Imaging 36(12):2557–2568
Gong C, Han C, Gan G et al (2017) Low-dose dynamic myocardial perfusion CT image reconstruction using pre-contrast normal-dose CT scan induced structure tensor total variation regularization. Phys Med Biol 62(7):2612–2635
van Assen M, Pelgrim GJ, De Cecco CN et al (2019) Intermodel disagreement of myocardial blood flow estimation from dynamic CT perfusion imaging. Eur J Radiol 110:175–180
Engblom H, Xue H, Akil S et al (2017) Fully quantitative cardiovascular magnetic resonance myocardial perfusion ready for clinical use: a comparison between cardiovascular magnetic resonance imaging and positron emission tomography. J Cardiovasc Magn Reson 19(1):78
Funding
This work was supported by the National Natural Science Foundation of China (81471721, 81471722, 81641169, 81771887, 81771897, 81901712, and 81971586); the Program for New Century Excellent Talents in University (No. NCET-13-0386); the Program for Young Scholars and Innovative Research Team in Sichuan Province (No. 2017TD0005) of China; the Applied and Fundamental Study of Sichuan Province (No. 2017JY0026); and 1·3·5 project for disciplines of excellence, West China Hospital, Sichuan University (No. ZYGD18013).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Zhi-gang Yang.
Conflict of interest
One of the authors of this manuscript (Xiao-yue Zhou) is an employee of Siemens Healthcare. The remaining authors declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Approval from the institutional animal care committee was obtained.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• experimental
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 94 kb)
Rights and permissions
About this article
Cite this article
Yang, Mx., Xu, Hy., Zhang, L. et al. Myocardial perfusion assessment in the infarct core and penumbra zones in an in-vivo porcine model of the acute, sub-acute, and chronic infarction. Eur Radiol 31, 2798–2808 (2021). https://doi.org/10.1007/s00330-020-07220-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07220-x