Abstract
Purpose
Breast lesions classified as of “uncertain malignant potential” represent a heterogeneous group of abnormalities with an increased risk of associated malignancy. Clinical management of B3 lesions diagnosed on vacuum-assisted breast biopsy (VABB) is still challenging: surgical excision is no longer the only available treatment and VABB may be sufficient for therapeutic excision. The aim of the present study is to evaluate the positive predictive value (PPV) for malignancy in B3 lesions that underwent surgical excision, identifying possible upgrading predictive factors and characterizing the malignant lesions eventually diagnosed. These results are compared with a subset of patients with B3 lesions who underwent follow-up.
Methods
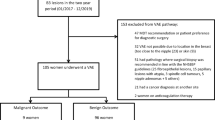
A total of 1250 VABBs were performed between January 2006 and December 2017 at our center. In total, 150 B3 cases were diagnosed and 68 of them underwent surgical excision. VABB findings were correlated with excision histology. A PPV for malignancy for each B3 subtype was derived.
Results
The overall PPV rate was 28%, with the highest upgrade rate for atypical ductal hyperplasia (41%), followed by classical lobular neoplasia (29%) and flat epithelial atypia (11%). Only two cases of carcinoma were detected in the follow-up cohort, both associated with atypical ductal hyperplasia at VABB.
Conclusion
Open surgery is recommended in case of atypical ductal hyperplasia while, for other B3 lesions, excision with VABB only may be an acceptable alternative if radio-pathological correlation is assessed, if all microcalcifications have been removed by VABB, and if the lesion lacks high-risk cytological features.
Key Points
• Surgical treatment is strongly recommended in case of ADH, while the upgrade rate in case of pure FEA, especially following complete microcalcification removal by VABB, may be sufficiently low to advice surveillance as a management strategy.
• The use of 11-G- or 8-G-needle VABB, resulting in possible complete diagnostic excision of the lesion, can be an acceptable alternative in case of RS, considering open surgery only for selected high-risk patients.
• LN management is more controversial: surgical excision may be recommended following classical LN diagnosis on breast biopsy if an additional B3 lesion is concurrently detected while in the presence of isolated LN with adequate radiological-pathological correlation follow-up alone could be an acceptable option.
Similar content being viewed by others
Abbreviations
- ADH:
-
Atypical ductal hyperplasia
- CNB:
-
Core needle biopsy
- FEA:
-
Flat epithelial atypia
- LN:
-
Classical lobular neoplasia
- PL:
-
Papillary lesions
- PPV:
-
Positive predictive value
- PT:
-
Benign phyllodes tumors
- RS:
-
Radial scars
- VABB:
-
Vacuum-assisted breast biopsy
References
Perry N, Broeders M, de Wolf C, Törnberg S, Holland R, von Karsa L (2008) European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition--summary document. Ann Oncol 19(4):614–622
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH, van de Vijver MJ (2012) WHO classification of tumours of the breast, 4th edn. International Agency for Research on Cancer, Lyon
Rakha EA, Shaaban AM, Haider SA et al (2013) Outcome of pure mucocele-like lesions diagnosed on breast core biopsy. Histopathology 62(6):894–898
Latronico A, Nicosia L, Faggian A et al (2018) Atypical ductal hyperplasia: our experience in the management and long term clinical follow-up in 71 patients. Breast 37:1–5
AGO (2016) Guidelines of the AGO breast committee: lesions of uncertain malignant potential (B3) (ADH, LIN, FEA, Papilloma, Radial Scar)
Alonso-Bartolomé P, Vega-Bolívar A, Torres-Tabanera M et al (2004) Sonographically guided 11-G directional vacuum-assisted breast biopsy as an alternative to surgical excision: utility and cost study in probably benign lesions. Acta Radiol 45(4):390–396
Hoon Tan P, Ellis I, Allison K et al (2020) The 2019 WHO classification of tumours of the breast. Histopathology. https://doi.org/10.1111/his.14091
Wolff AC, Hammond ME, Hicks DG et al (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31(31):3997–4013
Hahn M, Okamgba S, Scheler P et al (2008) Vacuum-assisted breast biopsy: a comparison of 11-gauge and 8-gauge needles in benign breast disease. World J Surg Oncol 6:51
Ruggirello I, Nori J, Desideri I et al (2017) Stereotactic vacuum-assisted breast biopsy: comparison between 11- and 8-gauge needles. Eur J Surg Oncol 43(12):2257–2260
Piubello Q, Parisi A, Eccher A, Barbazeni G, Franchini Z, Iannucci A (2009) Flat epithelial atypia on core needle biopsy: which is the right management? Am J Surg Pathol 33(7):1078–1084
Rakha EA, Ho BC, Naik V et al (2011) Outcome of breast lesions diagnosed as lesion of uncertain malignant potential (B3) or suspicious of malignancy (B4) on needle core biopsy, including detailed review of epithelial atypia. Histopathology 58(4):626–632
Rageth CJ, O'Flynn EA, Comstock C et al (2016) First International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 159(2):203–213
Rageth CJ, O'Flynn EAM, Pinker K et al (2019) Second International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 174(2):279–296
Calhoun BC, Sobel A, White RL et al (2015) Management of flat epithelial atypia on breast core biopsy may be individualized based on correlation with imaging studies. Mod Pathol 28(5):670–676
Hayes BD, O’Doherty A, Quinn CM (2009) Correlation of needle core biopsy with excision histology in screen-detected B3 lesions: the Merrion Breast Screening Unit experience. J Clin Pathol 62(12):1136–1140
Noske A, Pahl S, Fallenberg E et al (2010) Flat epithelial atypia is a common subtype of B3 breast lesions and is associated with noninvasive cancer but not with invasive cancer in final excision histology. Hum Pathol 41(4):522–527
Mayer S, Kayser G, Rücker G et al (2017) Absence of epithelial atypia in B3-lesions of the breast is associated with decreased risk for malignancy. Breast 31:144–149
Linda A, Zuiani C, Bazzocchi M, Furlan A, Londero V (2008) Borderline breast lesions diagnosed at core needle biopsy: can magnetic resonance mammography rule out associated malignancy? Preliminary results based on 79 surgically excised lesions. Breast 17(2):125–131
Londero V, Zuiani C, Linda A, Girometti R, Bazzocchi M, Sardanelli F (2012) High-risk breast lesions at imaging-guided needle biopsy: usefulness of MRI for treatment decision. AJR Am J Roentgenol 199(2):W240–W250
Bertani V, Urbani M, La Grassa M et al (2020) Atypical ductal hyperplasia: breast DCE-MRI can be used to reduce unnecessary open surgical excision. Eur Radiol. https://doi.org/10.1007/s00330-020-06701-3
Ancona A, Capodieci M, Galiano A, Mangieri F, Lorusso V, Gatta G (2011) Vacuum-assisted biopsy diagnosis of atypical ductal hyperplasia and patient management. Radiol Med 116(2):276–291
Rageth CJ, Rubenov R, Bronz C et al (2019) Atypical ductal hyperplasia and the risk of underestimation: tissue sampling method, multifocality, and associated calcification significantly influence the diagnostic upgrade rate based on subsequent surgical specimens. Breast Cancer 26(4):452–458
Nguyen CV, Albarracin CT, Whitman GJ, Lopez A, Sneige N (2011) Atypical ductal hyperplasia in directional vacuum-assisted biopsy of breast microcalcifications: considerations for surgical excision. Ann Surg Oncol 18(3):752–761
McGhan LJ, Pockaj BA, Wasif N, Giurescu ME, McCullough AE, Gray RJ (2012) Atypical ductal hyperplasia on core biopsy: an automatic trigger for excisional biopsy? Ann Surg Oncol 19(10):3264–3269
Menes TS, Rosenberg R, Balch S, Jaffer S, Kerlikowske K, Miglioretti DL (2014) Upgrade of high-risk breast lesions detected on mammography in the Breast Cancer Surveillance Consortium. Am J Surg 207(1):24–31
Kohr JR, Eby PR, Allison KH et al (2010) Risk of upgrade of atypical ductal hyperplasia after stereotactic breast biopsy: effects of number of foci and complete removal of calcifications. Radiology 255(3):723–730
Khoury T, Chen X, Wang D et al (2015) Nomogram to predict the likelihood of upgrade of atypical ductal hyperplasia diagnosed on a core needle biopsy in mammographically detected lesions. Histopathology 67(1):106–120
Deshaies I, Provencher L, Jacob S et al (2011) Factors associated with upgrading to malignancy at surgery of atypical ductal hyperplasia diagnosed on core biopsy. Breast 20(1):50–55
Rakha EA, Lee AH, Jenkins JA, Murphy AE, Hamilton LJ, Ellis IO (2011) Characterization and outcome of breast needle core biopsy diagnoses of lesions of uncertain malignant potential (B3) in abnormalities detected by mammographic screening. Int J Cancer 129(6):1417–1424
Mesurolle B, Perez JC, Azzumea F et al (2014) Atypical ductal hyperplasia diagnosed at sonographically guided core needle biopsy: frequency, final surgical outcome, and factors associated with underestimation. AJR Am J Roentgenol 202(6):1389–1394
Tsuchiya K, Mori N, Schacht DV et al (2017) Value of breast MRI for patients with a biopsy showing atypical ductal hyperplasia (ADH). J Magn Reson Imaging 46(6):1738–1747
Forgeard C, Benchaib M, Guerin N et al (2008) Is surgical biopsy mandatory in case of atypical ductal hyperplasia on 11-gauge core needle biopsy? A retrospective study of 300 patients. Am J Surg 196(3):339–345
Prowler VL, Joh JE, Acs G et al (2014) Surgical excision of pure flat epithelial atypia identified on core needle breast biopsy. Breast 23(4):352–356
Villa A, Chiesa F, Massa T et al (2013) Flat epithelial atypia: comparison between 9-gauge and 11-gauge devices. Clin Breast Cancer 13(6):450–454
Dialani V, Venkataraman S, Frieling G, Schnitt SJ, Mehta TS (2014) Does isolated flat epithelial atypia on vacuum-assisted breast core biopsy require surgical excision? Breast J 20(6):606–614
Bianchi S, Bendinelli B, Castellano I et al (2012) Morphological parameters of flat epithelial atypia (FEA) in stereotactic vacuum-assisted needle core biopsies do not predict the presence of malignancy on subsequent surgical excision. Virchows Arch 461(4):405–417
Peres A, Barranger E, Becette V, Boudinet A, Guinebretiere JM, Cherel P (2012) Rates of upgrade to malignancy for 271 cases of flat epithelial atypia (FEA) diagnosed by breast core biopsy. Breast Cancer Res Treat 133(2):659–666
Lavoué V, Roger CM, Poilblanc M et al (2011) Pure flat epithelial atypia (DIN 1a) on core needle biopsy: study of 60 biopsies with follow-up surgical excision. Breast Cancer Res Treat 125(1):121–126
Chivukula M, Bhargava R, Tseng G, Dabbs DJ (2009) Clinicopathologic implications of “flat epithelial atypia” in core needle biopsy specimens of the breast. Am J Clin Pathol 131(6):802–808
Darvishian F, Singh B, Simsir A, Ye W, Cangiarella JF (2009) Atypia on breast core needle biopsies: reproducibility and significance. Ann Clin Lab Sci 39(3):270–276
Ingegnoli A, d'Aloia C, Frattaruolo A et al (2010) Flat epithelial atypia and atypical ductal hyperplasia: carcinoma underestimation rate. Breast J 16(1):55–59
Verschuur-Maes AH, van Deurzen CH, Monninkhof EM, van Diest PJ (2012) Columnar cell lesions on breast needle biopsies: is surgical excision necessary? A systematic review. Ann Surg 255(2):259–265
Morrow M, Schnitt SJ, Norton L (2015) Current management of lesions associated with an increased risk of breast cancer. Nat Rev Clin Oncol 12(4):227–238
Meroni S, Bozzini AC, Pruneri G et al (2014) Underestimation rate of lobular intraepithelial neoplasia in vacuum-assisted breast biopsy. Eur Radiol 24(7):1651–1658
Dabbs DJ (2012) Breast pathology, 1st edn. Elsevier
D’Alfonso TM, Wang K, Chiu YL, Shin SJ (2013) Pathologic upgrade rates on subsequent excision when lobular carcinoma in situ is the primary diagnosis in the needle core biopsy with special attention to the radiographic target. Arch Pathol Lab Med 137(7):927–935
Wen X, Cheng W (2013) Nonmalignant breast papillary lesions at core-needle biopsy: a meta-analysis of underestimation and influencing factors. Ann Surg Oncol 20(1):94–101
Kim MJ, Kim SI, Youk JH et al (2011) The diagnosis of non-malignant papillary lesions of the breast: comparison of ultrasound-guided automated gun biopsy and vacuum-assisted removal. Clin Radiol 66(6):530–535
Mosier AD, Keylock J, Smith DV (2013) Benign papillomas diagnosed on large-gauge vacuum-assisted core needle biopsy which span <1.5 cm do not need surgical excision. Breast J 19(6):611–617
Youk JH, Kim MJ, Son EJ, Kwak JY, Kim EK (2012) US-guided vacuum-assisted percutaneous excision for management of benign papilloma without atypia diagnosed at US-guided 14-gauge core needle biopsy. Ann Surg Oncol 19(3):922–928
Calhoun BC, Collins LC (2016) Recommendations for excision following core needle biopsy of the breast: a contemporary evaluation of the literature. Histopathology. 68(1):138–151
Ditsch N, Untch M, Thill M et al (2019) AGO recommendations for the diagnosis and treatment of patients with early breast cancer: update 2019. Breast Care (Basel) 14(4):224–245
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor name
The scientific guarantor of this publication is Di Giulio Giuseppe.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and Biometry
No complex statistical methods were necessary for this paper
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was not required because it is a retrospective study.
Methodology
• retrospective
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lucioni, M., Rossi, C., Lomoro, P. et al. Positive predictive value for malignancy of uncertain malignant potential (B3) breast lesions diagnosed on vacuum-assisted biopsy (VAB): is surgical excision still recommended?. Eur Radiol 31, 920–927 (2021). https://doi.org/10.1007/s00330-020-07161-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07161-5