Abstract
Objectives
To quantitatively and qualitatively evaluate image quality in dual-layer CT (DLCT) compared to single-layer CT (SLCT) in the thorax, abdomen, and pelvis in a reduced-dose setting.
Methods
Intraindividual, retrospective comparisons were performed in 25 patients who received at least one acquisition of all three acquisition protocols SLCTlow (100 kVp), DLCThigh (120 kVp), and DLCTlow (120 kVp), all covering the venous-phase thorax, abdomen, and pelvis with matched CTDIvol between SLCTlow and DLCTlow. Reconstruction parameters were identical between all scans. Image quality was assessed quantitatively at 10 measurement locations in the thorax, abdomen, and pelvis by two independent observers, and subjectively with an intraindividual forced choice test between the three acquisitions. Dose-length product (DLP) and CTDIvol were extracted for dose comparison.
Results
Despite matched CTDIvol in acquisition protocols, CTDIvol and DLP were lower for SLCTlow compared to DLCTlow and DLCThigh (DLP 408.58, 444.68, 647.08 mGy·cm, respectively; p < 0.0004), as automated tube current modulation for DLCTlow reached the lower limit in the thorax (mean 66.1 mAs vs limit 65 mAs). Noise and CNR were comparable between SLCTlow and DLCTlow (p values, 0.29–0.51 and 0.05–0.20), but CT numbers were significantly higher for organs and vessels in the upper abdomen for SLCTlow compared to DLCTlow. DLCThigh had significantly better image quality (Noise and CNR). Subjective image quality was superior for DLCThigh, but no difference was found between SLCTlow and DLCTlow.
Conclusions
DLCTlow showed comparable image quality to SLCTlow, with the additional possibility of spectral post-processing. Further dose reduction seems possible by decreasing the lower limit of the tube current for the thorax.
Key Points
• Clinical use of reduced-dose DLCT is feasible despite the required higher tube potential.
• DLCT with reduced dose shows comparable objective and subjective image quality to reduced-dose SLCT.
• Further dose reduction in the thorax might be possible by adjusting mAs thresholds.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of dual-layer detector technology in computed tomography (CT) enabled the acquisition of spectral data for all performed scans without the need of an additional CT x-ray tube or additional acquisitions. Dual-layer spectral CT (DLCT) acquisitions allow material decomposition (virtual non-contrast, iodine-only imaging, and effective atomic numbers) as well as the calculation of virtual monoenergetic images. Several clinical studies have already been performed showing the advantages of DLCT for head CT for imaging intracerebral lesions and hemorrhage, for thoracic CT, for vertebral CT for differentiating bone lesions, and for abdominal CT angiographies for improved delineation of visceral arteries [1,2,3,4,5]. However, for the image acquisition of such data, a tube potential of either 140 kVp or 120 kVp is necessary to allow for spectral decomposition under the exploitation of the energy-specific x-ray absorption of different materials. In contrast to changes in tube current, changes in tube potential have a non-linear effect on radiation dose: in comparison to 80 kVp, the x-ray tube output (i.e., air kerma or exposure) is 1.5 times higher for 100 kVp, 2.5 times higher for 120 kVp, and 3.4 times higher for 140 kVp [6].
While patient radiation exposure has long been a topic of interest in CT, as CT accounts for 49–66% of overall patient radiation exposure, this interest has recently led to new regulations in the European Union via the EURATOM directive, with the deadline for implementation into federal law in 2018 [7, 8]. Based on surveys, diagnostic reference levels (DRLs) at the 75th percentile of dose distribution have been defined as the limits of appropriate practice for CT acquisitions. In our institution, acquisition protocols for the thorax, abdomen, and pelvis have been previously optimized to reduce patient radiation exposure beyond these legal requirements. This was achieved, in part, by reducing tube potential from 120 to 100 kVp for single-layer CT (SLCT), resulting in an average patient dose 60% below the federal DRL for the thorax, abdomen, and pelvis, which is a DLP of 1000 mGy·cm and a CTDIvol of 13 mGy.
With the installation of a novel DLCT, vendor’s recommended settings were applied including a tube potential of 120 kVp (acquisition protocol DLCThigh), which led to an increase in radiation exposure in comparison to previous reduced-dose SLCT protocols (acquisition protocol SLCTlow), albeit still remaining below the applicable diagnostic reference levels. After initial experience with DLCThigh, the tube current was reduced (acquisition protocol DLCTlow) to match the CTDIvol of the reduced-dose protocol previously performed on the SLCT scanner at 100 kVp (SLCTlow).
The aim of the study was to quantitatively and qualitatively compare the image quality and radiation exposure of the SLCT acquisition protocol with reduced dose, SLCTlow (41% of the national DRL), and the DLCT acquisition protocol with reduced dose, DLCTlow (44% of the DRL). Thus, by comparing DLCTlow and SLCTlow, we want to aid in the deployment of protocols with reduced dose in DLCT with image quality comparable to previous low-tube potential SLCTlow, while allowing to benefit from the spectral information in a clinical setting.
Material and methods
Ethics approval and consent
This retrospective study was approved by the institutional review board. The need for written informed consent was waived.
Patient selection
Ninety-six patients who underwent low-dose DLCT (DLCTlow) and previous low-dose SLCTlow with clinical indication for oncological staging, since October 2018, were screened for inclusion into the study (Fig. 1). Intensive care patients and obese patients were excluded from the study, as low-dose protocols are not routinely used in these circumstances and obese patients require adapted acquisition protocols to guarantee adequate image quality. Arterial-phase acquisitions or venous-phase examinations with additional arterial angiography phase were not considered for the study to ensure comparability of the evaluated acquisitions, as those are to prone to effects of contrast agent volume, injection speed of the contrast agent, and circulation and cardiac output. In consequence, only patients with a routine CT acquisition of the thorax, abdomen, and pelvis in the venous phase were included into the study. All patients received a similar total amount of contrast agent in all their examinations with a maximum intraindividual difference of 5 ml. Patients with diffuse liver parenchyma diseases (liver cirrhosis and liver metastases), liver perfusion deficit, or intracorporal metal implants (e.g., hip prosthesis or spinal hardware) were excluded from the study. Furthermore, non-standard CT examinations as defined by differences in the acquisition protocol were excluded from the study. In summary, 31 patients were included into the study, who previously underwent 51 SLCTlow examinations, 39 DLCThigh examinations, and 34 DLCTlow examinations with adjusted parameters (Fig. 1). The mean interval between the acquisitions with the different acquisition protocols was 224.6 ± 89.8 days (median, 190 days) between SLCTlow and DLCThigh and 182.2 ± 70.5 days (median, 183.5 days) between DLCThigh and DLCTlow. A subgroup of 25 patients had been examined with all three CT acquisition protocols and was used for qualitative analysis.
CT acquisition parameters
CT acquisitions were performed with a standard acquisition protocol for oncological staging covering the thorax, abdomen, and pelvis by a single continuous acquisition (all three scan protocols). Acquisition parameters of SLCTlow (iCT, Philips Healthcare), DLCTlow, and DLCThigh (IQon Spectral CT, Philips Healthcare) are shown in Table 1. SLCTlow was performed with a tube potential of 100 kVp, while all DLCTs were performed with a tube potential 120 kVp. For DLCThigh, standard acquisition settings were used as per the manufacturer’s presets. For DLCTlow, the automated tube current modulation (DoseRight 3D-DOM, Philips Healthcare) was adjusted by reducing dose right index (DRI) from 17 to 13 to match the SLCTlow protocol, achieving a similar predicted CTDIvol, as displayed when editing the acquisition protocol in the CT scanner interface (DLCTlow 7.5 mGy, SLCTlow 7.8 mGy). Accordingly, predicted average mAs was lower for DLCTlow (74 mAs) compared to DLCThigh (116 mAs).
Collimation (single collimation width 0.625 mm and total collimation width 40 mm) and pitch (0.798) was identical for all scans.
All examinations were conducted in craniocaudal direction and supine position, with automatic exposure control as described above. For all acquisitions, iohexol contrast agent (AccupaqueTM 350, GE Healthcare) was used. Contrast agent application was performed using a power injector with an injection rate of 3 ml/s. A routine biphasic contrast-injection scan protocol was used covering the thorax, abdomen, and pelvis in the venous phase. The first contrast agent injection and saline solution chaser bolus was followed by a 30-s break and a second contrast agent injection with a saline solution chaser bolus. Then the CT acquisition was performed 60 s after the second contrast agent injection. The combined acquisition of thorax and abdominal region in the venous phase achieves better delineation of the lymph nodes, thoracic wall, and mediastinal soft tissue with less artifacts than a thoracic arterial phase for oncological staging [9]. As previously stated, only patients who received a venous-phase CT acquisition of the thorax, abdomen, and pelvis were included in the study.
Image reconstruction and post-processing
For all examinations, axial series with a slice thickness of 3 mm and increment of 1.5 mm were reconstructed. Images were reconstructed with a vendor-specific iterative reconstruction algorithm, IMR at level 1 (Iterative Model Reconstruction, Philips Healthcare), soft-tissue setting, and a standard abdomen setting (window center/width 40/400 HU).
Dose and image analysis
Quantitative and qualitative analysis were performed by two radiologists with 7 and 6 years of experience in abdominal radiology. For quantitative analysis, all acquisitions were included. For qualitative analysis, the most recent examination of each acquisition protocol (SLCTlow, DLCThigh, and DLCTlow) was included and only patients that were scanned with all three acquisition protocols were included.
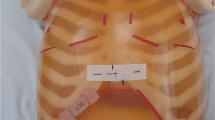
Patients’ anterior-posterior and lateral diameters were measured separately for the thorax at the level of tracheal bifurcation, the upper abdomen at the level of the portal vein, and the lower abdomen at the level of lumbar spine L4 (Fig. 2). Total scan lengths were calculated from the images.
Image examples of regions of interest (ROIs) used for the quantitative evaluation in the thorax at the height of the tracheal bifurcation (a), the upper abdomen at the height of the portal vein (b), and the lower abdomen at the level of the lumbar spine L4 (c). Rectangle for measurements of the lateral and anterior-posterior diameter of the torso
Quantitative image analysis was performed by placement of regions of interest (ROIs) in axial slices in the following positions (Fig. 2):
-
a)
Level of the tracheal bifurcation: in the subcutaneous fat, peripheral lung parenchyma, and air within the trachea
-
b)
Level of the portal vein: in the subcutaneous fat of the right upper abdomen, liver parenchyma, portal vein, aorta, and spleen
-
c)
Level of the lumbar spine L4: in the subcutaneous fat of the right lower abdomen and psoas muscle
For all three axial slices, the slice-specific tube current-exposure time product, lateral, and anterior-posterior torso diameter were determined. An in-house developed software was used for semiautomatic quantitative image quality analysis to maintain constant ROI area size of 50 mm2 in order to enhance reproducibility and time-efficient evaluation [10]. Noise was defined as the standard deviation (SD) of CT numbers of the subcutaneous fat on the right side of the ventral thorax or abdomen for improved comparability. Mean and SD of CT numbers were recorded and CNR was calculated as follows:
The following ROIs were used to calculate CNR in comparison to the subcutaneous fat on their respective axial slice: lung parenchyma (thorax), liver parenchyma (upper abdomen), and psoas muscle (lower abdomen).
For qualitative image evaluation comparing SLCTlow, DLCThigh, and DLCTlow (Fig. 3), a forced choice method was used for a blinded and randomized side-by-side review. For randomization, both the order of patients and evaluated series were randomized by the statistician, who was not involved in qualitative image evaluation, using the random function of EXCEL (Microsoft). Two observers independently performed the qualitative analysis on conventional CT images reconstructed from all three acquisition protocols. First, images from all three acquisition protocols were separately ranked for three body regions covered by the acquisition protocols taking into account the following criteria [11]:
-
Thorax: noise in the subcutaneous fat of the right thorax, delineation of trachea, bronchi, and spinal cord
-
Upper abdomen: noise in the right-sided subcutaneous fat, delineation of portal vein, aorta, and spinal cord
-
Lower abdomen: noise in the right-sided subcutaneous fat, delineation of gluteal muscles, and spinal cord
Image examples from the same patient from conventional reduced-dose SLCTlow (column 1), DLCTlow (column 2), and DLCThigh (column 3) from thorax (a), upper abdomen (b), and pelvis (c). DLCThigh (column 2) showed best quantitative and qualitative analysis whereas SLCTlow (column 1) and DLCTlow (column 3) showed comparable results
Based on the rankings for the three body regions, unique ranks from 1 to 3 were allocated to the evaluated image series (i.e., observes were forced to choose which image has the best image quality compared to the others) as a total score, whereby a rank of 1 corresponded to the best image quality.
DLPs, CTDIvol, and overall tube current-time product were extracted from the patient’s dose report images sent to the picture archiving system. Size-specific dose estimates (SSDEs) for each patient and each body region were calculated according to the recommendations of the American Association of Physicsts in Medicine Task Group 204 [12]. CTDIvol and DLP are frequently used parameters for estimation of a patient’s radiation exposure. However, SSDE is a more precise method for the patient’s absorbed dose as it takes the patient’s size into account [13]. To calculate SSDE for the individual anatomical region, a region-specific CTDIvol,region was estimated by dividing the CTDIvol for the complete acquisition by the average tube current-time product and multiplying it with the tube current-time product of the representative axial slice of each region (Fig. 2):
The resulting estimated region-specific CTDIvol,region was multiplied with the recommended conversion coefficient depending on the lateral and AP diameter of the selected anatomical region [13].
Statistical analysis
Statistical analysis was performed using SAS Version 9.4 (SAS Institute Inc.) and SPSS Version 19.0 (IBM). Descriptive statistics were calculated, determining means and standard deviations for normal distributed data. CT numbers, image noise approximated by the standard deviation of measured CT numbers, and CNR were analyzed for differences depending on the CT scanner and the acquisition protocol using a mixed model for unbalanced analysis of variances for repeated measures.
Qualitative ratings of image quality were analyzed for differences depending on the CT scanner and the acquisition protocol using non-parametric tests (Friedman test stratified for patients and Wilcoxon signed-rank test in a multistage design).
For the evaluation of the inter-rater agreement of the quantitative analysis, the intraclass correlation coefficient (ICC) was used and for the qualitative analysis Cohen’s kappa was calculated and classified according to Landis and Koch [14]. The significance level for statistical testing was set at p < 0.05.
Results
Quantitative analysis
Although the average scan length of DLCTlow was significantly shorter than that for SLCTlow (p > 0.0001) with an average difference of 13.8 mm, DLP for DLCTlow was significantly higher due to higher CTDIvol of DLCTlow in comparison to SLCTlow (444.68 mGy·cm and 408.58 mGy·cm, respectively; p = 0.0004) (Table 2). CTDIvol of DLCTlow (6.57 mGy) was 30% lower than that of DLCThigh (9.34 mGy; p < 0.0001). Despite the efforts to match radiation dose, average CTDIvol was 14.4% higher for DLCTlow compared to SLCTlow (p < 0.0001). Similar to CTDIvol and DLP, the SSDE was lowest for SLCTlow while SSDE of DLCTlow was significantly less than DLCThigh for all body regions (p < 0.0001). DLCThigh had significantly higher CTDIvol (p < 0.0001) and higher DLP (p < 0.0001) resulting from higher tube potential in comparison to SLCTlow, despite comparable scan length to SLCTlow (p = 0.56).
A decrease of the mean lateral diameter of patients over time was observed, with a maximum difference/change of 10.3 mm (Table 3). There was also a statistically significant difference of both the lateral thoracic and lower abdominal diameter between the first (and earliest) examination with SLCTlow in comparison to the acquisitions with DLCThigh (p < 0.0006 and 0.0029, respectively), but the mean difference was only 5.6 mm (thorax) and 9.2 mm (lower abdomen). No significant differences in anterior-posterior (AP) diameter were observed for all three abdominal regions.
In general, the lowest tube current-time product was found for DLCTlow in all three regions, showing a statistically significant difference compared to DLCThigh in the lower and upper abdomen, but not in the thorax (Table 3). It has to be noted that for the thorax, the average tube current-time product of DLCTlow was 66.1 mAs, which is close to the minimum mAs of the tube current modulation preset at 65 mAs (Fig. 4). Also, mAs for the upper and lower abdomen was lowest for DLCTlow, at approximately 49–51% of SLCTlow.
Example of tube current-time product curves for the three evaluated acquisition protocols in one patient. Note the changes in tube current in the different anatomical regions caused by the automated exposure control, as well as the changes during the rotation of the x-ray tube around the patient table
There was no significant difference in noise between SLCTlow, DLCTlow, and DLCThigh for the thorax and upper abdomen (p between 0.08 and 0.61). No significant difference in noise was found between SLCTlow and DLCTlow in the lower abdomen (p = 0.51). In general, noise was lowest for DLCThigh, but the difference was only statistically significant in the lower abdomen (p < 0.05) (Table 4). No significant difference was found for CNR in the thorax and upper abdomen between SLCTlow and DLCTlow. In the lower abdomen, CNR for DLCTlow was significantly lower than that for DLCThigh, but no significant difference was found between DLCTlow and SLCTlow. As for CT numbers, highest values were observed for vessels, e.g. aorta and portal vein, in comparison to organ parenchyma due to the use of contrast agent (Table 5). CT numbers of vessels in SLCTlow were significantly higher than those for both DLCTlow and DLCThigh which can be attributed to higher CT numbers observed for contrast agents at the lower tube potential of 100 kVp versus 120 kVp. CT numbers for DLCThigh and DLCTlow in organ parenchyma did not show significant differences, except for the liver, which can show considerable contrast agent uptake, where the mean difference was 13.7 HU between SLCTlow and DLCThigh.
Qualitative analysis
No significant image quality differences were observed between SLCTlow and DLCTlow (p = 0.97). Overall, best image quality was observed for DLCThigh (mean rank ± SD, 1.62 ± 0.62) in comparison to SLCTlow (2.2 ± 0.71) and DLCTlow (2.18 ± 0.72) with p < 0.01 (Fig. 5).
ICC for quantitative inter-rater agreement was on average 0.89. Interobserver agreement for qualitative analysis was moderate with Cohen’s kappa of 0.42 according to the classification of Landis and Koch [14].
Discussion
The necessity to increase the tube potential to at least 120 kVp for spectral imaging with current DLCT results in an increase of patient radiation exposure, compared with conventional single-layer acquisitions performed at 100 kVp. As a compensation tube current-time product might be adapted to achieve equivalent CTDIvol to standard-, reduced-, or low-dose SLCT protocols. The results in this study show that patient radiation exposure can be restored to levels close to that of reduced-dose SLCT with comparable image quality by adjusting automated exposure control (i.e., DRI). Image quality was comparable between DLCTlow and SLCTlow despite the changes in tube potential and the resulting changes in tube current-time product. Thus, a notable dose reduction due to adjusted automatic exposure control can be achieved in DLCT protocols compared to standard protocols, but further reductions might be possible by fine-tuning the lower threshold for tube current-time product.
Previously, Van Ommen et al [15] had already shown that DLCT can be used for a broad range of applications without increasing patient radiation exposure compared to normal-dose SLCT. However, neither quantitative nor qualitative image quality was evaluated in this study. Another aspect of our study was the adaptation of DLCT to match previous low-dose SLCTlow with DLCTlow, which shows lower radiation doses than the current literature [15, 16]. Moreover, the results show that even further dose reduction could be possible, especially in the thorax region where the automated exposure control reached the lower threshold of tube current-time product set in the acquisition protocol. According to the presented results, further dose reduction might be achieved by reducing the lower limit of the tube current from 65 to 55 mAs. According to Nagayama et al [17], DLCT showed a lower radiation dose than SLCT at equal tube potential of 120 kVp. However, with regard to image quality of conventional DLCT images, which is currently still the most frequently used reconstruction in clinical settings, no comparison was made with SLCT. Conventional CT images of dose equivalent DLCT and SLCT were already compared in a phantom study showing higher CNR but higher noise for DLCT compared to SLCT for 80–140 kVp, which was partly in agreement with the results presented here [18]. It should also be noted that despite matched CTDIvol between SLCTlow and DLCTlow, as configured in the acquisition protocol (Table 1), the resulting CTDIvol for DLCTlow was higher than that for the SLCTlow (Table 2), which could be connected to the lower limit for the tube current mentioned above.
In general, the aspect of patient radiation exposure in spectral imaging has already been discussed in previous studies. No radiation dose increase is necessary for dual-source, dual-energy scans without compromises in image quality of the thorax and abdomen [19,20,21]. Rapid voltage switching dual-energy acquisition has shown ambiguous results. Singh et al showed dose equivalence to dual-source, dual-energy acquisition but with inferior image quality whereas other authors state that rapid voltage switching acquisition results in higher patient’s radiation [22, 23].
One limitation of the study is that the patients included in the quantitative evaluation were not scanned with all acquisition protocols, as 6 out of 31 patients were only scanned with two of the three protocols. As the quantitative evaluation did not rely on pairwise comparisons, but used an unbalanced design instead, it was possible to include patients where one of the acquisitions was missing as well as to include multiple acquisitions of the same patient. This was done to increase the statistical power of the results, as the overall number of patients included in this study was relatively low, which is another limitation. Because of the limited number of patients, the transferability of the obtained results to clinical practice may be limited as well. One of the reasons for the limited number of patients in this study is the restriction to a single acquisition protocol, which, even though it is the most frequently used acquisition protocol at that CT scanner, limits the overall number of eligible patients and also limits the transferability of the obtained results to other acquisition protocols. However, comparing different protocols at once would have led to an unnecessary complexity of the evaluation, as additional variables would have to be considered. This is also true for the inclusion of arterial-phase imaging, which is more susceptible to changes in patient habitus, cardiac output, and underlying disease (e.g., differences in enhancement patterns for different tumors, as evident in pancreatic carcinoma [24]). While the results achieved in this study are specific for the acquisition protocol and body region, and obtained from a limited number of patients, and reductions in patient radiation exposure may be larger or smaller for other protocols or patient collectives, which has to be the subject of further evaluation in the future, we do expect that the results are nonetheless fairly generalizable, as we chose to evaluate a single, widely applicable acquisition protocol that makes up the bulk of acquisitions at the evaluated CT scanner. Even though there is no clear consensus on the definition of low dose, with an average patient dose of 60% below the applicable DRL, the evaluated acquisition protocol in this study qualifies as “reduced dose” [25].
Another limitation of this study and the DLCT acquisition protocols with increased tube potential might be the inferior conspicuity of vessel structures at higher tube potential, as mean photon energies closer to the k-edge of iodine provide improved image contrast [26]. However, with the additional possibility of spectral post-processing provided by DLCT, vessel delineation might be improved with virtual monochromatic images at lower virtual photon energies [27]. Furthermore, only conventional images of DLCT were analyzed in this study, even though spectral imaging was the main reason for the tube potential increase. Nonetheless, the number of potential spectral post-processing applications is very large and the quantification of the potential benefit from the additional spectral information for clinical routine is beyond the scope of this study.
Regarding the results, the inter-reader agreement for qualitative analysis was found to be moderate. However, this might be a consequence of the forced choice method used for evaluation combined with the low number of available choice (3 images). In consequence, a disagreement of ranking for one patient always consists of at least two further mismatches, resulting in a moderate Cohen’s kappa. As all CT images were of diagnostic quality, the forced choice method was able to provide a side-by-side comparison, allowing to identify even small differences in image quality that might otherwise remain hidden with more conventional methods, like rating image quality on a Likert scale. Moreover, the quantitative analysis found differences in the delineation of vasculature as shown by the differences in CT numbers measured in the vessels. These differences did not lead to significant differences in subjective image quality, as delineation of vasculature is but one aspect of overall image quality. While Singh et al or Tabari et al [22, 28] suggest to link the evaluation of image quality to the clinical task of lesion detection, this approach was not applicable to this study as not all patients had lesions in all three evaluated body regions. In consequence, future studies may evaluate different aspects of image quality to provide a more complete evaluation for different clinical tasks.
Conclusion
Overall, image quality of DLCTlow was comparable to SLCTlow and a low-dose acquisition was possible using dual-layer technique, which has the additional benefit of providing spectral information. With DLCTlow, CTDIvol could be reduced by 28% compared to DLCThigh, but remained above that of SLCTlow. Further reduction of patient radiation exposure for the thorax seems possible.
Abbreviations
- AP:
-
Anterior-posterior
- CNR:
-
Contrast-to-noise ratio
- CT:
-
Computed tomography
- CTDIvol :
-
Volumetric computed tomography dose index
- DLCT:
-
Dual-layer spectral CT
- DLP:
-
Dose-length product
- DRI:
-
Dose right index
- DRL:
-
Diagnostic reference levels
- ICC:
-
Intraclass-correlation coefficient
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- SLCT:
-
Single-layer CT
- SSDE:
-
Size-specific dose estimate
- VMSI:
-
Virtual monochromatic spectral imaging
References
Hickethier T, Byrtus J, Hauger M et al (2018) Utilization of virtual mono-energetic images (MonoE) derived from a dual-layer spectral detector CT (SDCT) for the assessment of abdominal arteries in venous contrast phase scans. Eur J Radiol 99:28–33
Doerner J, Luetkens JA, Iuga AI et al (2018) Poly-energetic and virtual mono-energetic images from a novel dual-layer spectral detector CT: optimization of window settings is crucial to improve subjective image quality in abdominal CT angiographies. Abdom Radiol (NY) 43:742–750
Doerner J, Hauger M, Hickethier T et al (2017) Image quality evaluation of dual-layer spectral detector CT of the chest and comparison with conventional CT imaging. Eur J Radiol 93:52–58
Borggrefe J, Neuhaus VF, Le Blanc M et al (2019) Accuracy of iodine density thresholds for the separation of vertebral bone metastases from healthy-appearing trabecular bone in spectral detector computed tomography. Eur Radiol 29:3253–3261
Lennartz S, Laukamp KR, Neuhaus V et al (2018) Dual-layer detector CT of the head: initial experience in visualization of intracranial hemorrhage and hypodense brain lesions using virtual monoenergetic images. Eur J Radiol 108:177–183
Huda W, Scalzetti EM, Levin G (2000) Technique factors and image quality as functions of patient weight at abdominal CT. Radiology 217:430–435
Mettler FA Jr, Bhargavan M, Faulkner K et al (2009) Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources--1950-2007. Radiology 253:520–531
Strahlenschutz Bf Röntgendiagnostik: Häufigkeit und Strahlenexposition. Available via https://www.bfs.de/DE/themen/ion/anwendung-medizin/diagnostik/roentgen/haeufigkeit-exposition.html. Accessed 30 Nov 2019
Garcia-Garrigos E, Arenas-Jimenez JJ, Sanchez-Paya J (2018) Best protocol for combined contrast-enhanced thoracic and abdominal CT for lung cancer: a single-institution randomized crossover clinical trial. AJR Am J Roentgenol 210:1226–1234
Pahn G, Skornitzke S, Schlemmer HP, Kauczor HU, Stiller W (2016) Toward standardized quantitative image quality (IQ) assessment in computed tomography (CT): a comprehensive framework for automated and comparative IQ analysis based on ICRU report 87. Phys Med 32:104–115
Gur D, Rubin DA, Kart BH et al (1997) Forced choice and ordinal discrete rating assessment of image quality: a comparison. J Digit Imaging 10:103–107
American Association of Physicists in Medicine (AAPM) Task Group 204 (2011): Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. Available via https://www.aapm.org/pubs/reports/RPT_204.pdf. Accessed 20 Dec 2019
Brink JA, Morin RL (2012) Size-specific dose estimation for CT: how should it be used and what does it mean? Radiology 265:666–668
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
van Ommen F, de Jong H, Dankbaar JW, Bennink E, Leiner T, Schilham AMR (2019) Dose of CT protocols acquired in clinical routine using a dual-layer detector CT scanner: a preliminary report. Eur J Radiol 112:65–71
Haneder S, Siedek F, Doerner J et al (2018) Thoracic-abdominal imaging with a novel dual-layer spectral detector CT: intra-individual comparison of image quality and radiation dose with 128-row single-energy acquisition. Acta Radiol 59:1458–1465
Nagayama Y, Nakaura T, Oda S et al (2018) Dual-layer detector CT of chest, abdomen, and pelvis with a one-third iodine dose: image quality, radiation dose, and optimal monoenergetic settings. Clin Radiol 73:1058 e1021–1058 e1029
van Ommen F, Bennink E, Vlassenbroek A et al (2018) Image quality of conventional images of dual-layer SPECTRAL CT: a phantom study. Med Phys 45:3031–3042
Schenzle JC, Sommer WH, Neumaier K et al (2010) Dual energy CT of the chest: how about the dose? Invest Radiol 45:347–353
Uhrig M, Simons D, Kachelriess M, Pisana F, Kuchenbecker S, Schlemmer HP (2016) Advanced abdominal imaging with dual energy CT is feasible without increasing radiation dose. Cancer Imaging 16:15
Siegel MJ, Curtis WA, Ramirez-Giraldo JC (2016) Effects of dual-energy technique on radiation exposure and image quality in pediatric body CT. AJR Am J Roentgenol 207:826–835
Singh R, Sharma A, McDermott S et al (2019) Comparison of image quality and radiation doses between rapid kV-switching and dual-source DECT techniques in the chest. Eur J Radiol 119:108639
Johnson TR (2012) Dual-energy CT: general principles. AJR Am J Roentgenol 199:S3–S8
Boland GW, O'Malley ME, Saez M, Fernandez-del-Castillo C, Warshaw AL, Mueller PR (1999) Pancreatic-phase versus portal vein-phase helical CT of the pancreas: optimal temporal window for evaluation of pancreatic adenocarcinoma. AJR Am J Roentgenol 172:605–608
Bankier AA, Kressel HY (2012) Through the looking glass revisited: the need for more meaning and less drama in the reporting of dose and dose reduction in CT. Radiology 265:4–8
Alkadhi H, Schindera ST (2011) State of the art low-dose CT angiography of the body. Eur J Radiol 80:36–40
Zopfs D, Lennartz S, Laukamp K et al (2018) Improved depiction of atherosclerotic carotid artery stenosis in virtual monoenergetic reconstructions of venous phase dual-layer computed tomography in comparison to polyenergetic reconstructions. Eur J Radiol 100:36–42
Tabari A, Ramandeep S, Khera RD et al (2019) Can fully iterative reconstruction technique enable routine abdominal CT at less than 1 mSv? Eur J Radiol Open 6:225–230
Acknowledgements
Dr. Thuy Duong Do was supported by a grant from the Medical Faculty of the University of Heidelberg.
Funding
Open Access funding provided by Projekt DEAL. This study has received funding by the Medical Faculty of the University of Heidelberg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Stephan Skornitzke.
Conflict of interest
Stephan Skornitzke has ownership interests in investment funds containing stock of healthcare companies. Dr. Wolfram Stiller is a member of the CT Advisory Board of Philips Medical Systems. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Dr. Stephan Skornitzke has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Study subjects or cohorts have not been previously reported.
Methodology
• Retrospective
• Experimental
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Do, T.D., Rheinheimer, S., Kauczor, HU. et al. Image quality evaluation of dual-layer spectral CT in comparison to single-layer CT in a reduced-dose setting. Eur Radiol 30, 5709–5719 (2020). https://doi.org/10.1007/s00330-020-06894-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06894-7