Abstract
Objectives
To investigate the predictive value of peritoneal carcinomatosis (PC) quantification by DWI in determining incomplete tumour debulking in ovarian carcinoma (OC).
Methods
Prospective patients with suspected stage III–IV or recurrent OC were recruited for DWI before surgery. PC on DWI was segmented semi-automatically by k-means clustering, retaining voxels with intermediate apparent diffusion coefficient (ADC) to quantify PC burden. A scoring system, functional peritoneal cancer index (fPCI), was proposed based on the segmentation of tumour volume in 13 abdominopelvic regions with additional point given to involvement of critical sites. ADC of the largest PC was recorded. The surgical complexity and outcomes (complete vs. incomplete tumour debulking) were documented. fPCI was correlated with surgical PCI (sPCI), surgical complexity, and its ability to predict incomplete tumour debulking.
Results
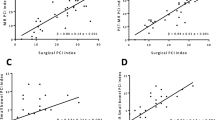
Fifty-three patients with stage III–IV or recurrent OC were included with a mean age of 56.1 ± 11.8 years old. Complete tumour debulking was achieved in 38/53 patients (71.7%). Significant correlation was found between fPCI and sPCI (r > 0.757, p < 0.001). Patients with high-fPCI (fPCI ≥ 6) had a high surgical complexity score (p = 0.043) with 84.2% received radical or supra-radical surgery. The mean fPCI was significantly higher in patients with incomplete tumour debulking than in those with complete debulking (10.27 vs. 4.71, p < 0.001). fPCI/ADC combined with The International Federation of Gynecology and Obstetrics stage achieved 92.5% accuracy in predicting incomplete tumour debulking (AUC 0.947).
Conclusions
DWI-derived fPCI offered a semi-automated estimation of PC burden. fPCI/ADC could predict the likelihood of incomplete tumour debulking with high accuracy.
Key Points
• Functional peritoneal cancer index (fPCI) derived from DWI offered a semi-automated estimation of tumour burden in ovarian carcinoma.
• fPCI was highly correlated with surgical PCI (sPCI).
• fPCI/ADC could predict the likelihood of incomplete tumour debulking with high accuracy.





Similar content being viewed by others
Abbreviations
- CA-125:
-
Cancer antigen-125
- CS:
-
Complexity score
- FIGO:
-
The International Federation of Gynecology and Obstetrics
- fPCI:
-
Functional peritoneal cancer index
- FTV:
-
Functional tumour volume
- IDS:
-
Interval debulking surgery
- NACT:
-
Neoadjuvant chemotherapy
- OC:
-
Ovarian carcinoma
- PC:
-
Peritoneal carcinomatosis
- sPCI:
-
Surgical peritoneal cancer index
- UDS:
-
Upfront debulking surgery
- VOI:
-
Volumes of interest
References
Dinkelspiel HE, Champer M, Hou J et al (2015) Long-term mortality among women with epithelial ovarian cancer. Gynecol Oncol 138:421–428
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J (2009) Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d’Investigateurs Nationaux Pour les Etudes des Cancers de l’Ovaire (GINECO). Cancer 115:1234–1244
Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ (2002) Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 20:1248–1259
Aletti GD, Dowdy SC, Gostout BS et al (2006) Aggressive surgical effort and improved survival in advanced-stage ovarian cancer. Obstet Gynecol 107:77–85
Wimberger P, Lehmann N, Kimmig R et al (2007) Prognostic factors for complete debulking in advanced ovarian cancer and its impact on survival. An exploratory analysis of a prospectively randomized phase III study of the Arbeitsgemeinschaft Gynaekologische Onkologie Ovarian Cancer Study Group (AGO-OVAR). Gynecol Oncol 106:69–74
Kehoe S, Hook J, Nankivell M et al (2015) Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet 386:249–257
Vergote I, Trope CG, Amant F et al (2010) Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med 363:943–953
Vergote I, Coens C, Nankivell M et al (2018) Neoadjuvant chemotherapy versus debulking surgery in advanced tubo-ovarian cancers: pooled analysis of individual patient data from the EORTC 55971 and CHORUS trials. Lancet Oncol 19:1680–1687
Querleu D, Planchamp F, Chiva L et al (2017) European Society of Gynaecological Oncology (ESGO) guidelines for ovarian cancer surgery. Int J Gynecol Cancer 27:1534–1542
Dowdy SC, Mullany SA, Brandt KR, Huppert BJ, Cliby WA (2004) The utility of computed tomography scans in predicting suboptimal cytoreductive surgery in women with advanced ovarian carcinoma. Cancer 101:346–352
Memarzadeh S, Lee SB, Berek JS, Farias-Eisner R (2003) CA125 levels are a weak predictor of optimal cytoreductive surgery in patients with advanced epithelial ovarian cancer. Int J Gynecol Cancer 13:120–124
Fagotti A, Ferrandina G, Fanfani F et al (2006) A laparoscopy-based score to predict surgical outcome in patients with advanced ovarian carcinoma: a pilot study. Ann Surg Oncol 13:1156–1161
Pedro Antonio CC, Alvaro Jesus GR, Jose G et al (2019) Validation of a peritoneal surface disease severity score in stage IIIC-IV ovarian cancer treated with cytoreduction and hyperthermic intraperitoneal chemotherapy. Surg Oncol 28:57–61
Passot G, Dumont F, Goere D et al (2018) Multicentre study of laparoscopic or open assessment of the peritoneal cancer index (BIG-RENAPE). Br J Surg 105:663–667
Vergote I, Marquette S, Amant F, Berteloot P, Neven P (2005) Port-site metastases after open laparoscopy: a study in 173 patients with advanced ovarian carcinoma. Int J Gynecol Cancer 15:776–779
Bristow RE, Duska LR, Lambrou NC et al (2000) A model for predicting surgical outcome in patients with advanced ovarian carcinoma using computed tomography. Cancer 89:1532–1540
Nelson BE, Rosenfield AT, Schwartz PE (1993) Preoperative abdominopelvic computed tomographic prediction of optimal cytoreduction in epithelial ovarian carcinoma. J Clin Oncol 11:166–172
Qayyum A, Coakley FV, Westphalen AC, Hricak H, Okuno WT, Powell B (2005) Role of CT and MR imaging in predicting optimal cytoreduction of newly diagnosed primary epithelial ovarian cancer. Gynecol Oncol 96:301–306
Axtell AE, Lee MH, Bristow RE et al (2007) Multi-institutional reciprocal validation study of computed tomography predictors of suboptimal primary cytoreduction in patients with advanced ovarian cancer. J Clin Oncol 25:384–389
Gemer O, Gdalevich M, Ravid M et al (2009) A multicenter validation of computerized tomography models as predictors of non- optimal primary cytoreduction of advanced epithelial ovarian cancer. Eur J Surg Oncol 35:1109–1112
Chong GO, Jeong SY, Lee YH et al (2019) The ability of whole-body SUVmax in F-18 FDG PET/CT to predict suboptimal cytoreduction during primary debulking surgery for advanced ovarian cancer. J Ovarian Res 12:12
Ebina Y, Watari H, Kaneuchi M et al (2014) Impact of FDG PET in optimizing patient selection for cytoreductive surgery in recurrent ovarian cancer. Eur J Nucl Med Mol Imaging 41:446–451
Risum S, Hogdall C, Loft A et al (2008) Prediction of suboptimal primary cytoreduction in primary ovarian cancer with combined positron emission tomography/computed tomography--a prospective study. Gynecol Oncol 108:265–270
Vargas HA, Burger IA, Goldman DA et al (2015) Volume-based quantitative FDG PET/CT metrics and their association with optimal debulking and progression-free survival in patients with recurrent ovarian cancer undergoing secondary cytoreductive surgery. Eur Radiol 25:3348–3353
Koh DM, Collins DJ (2007) Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol 188:1622–1635
Michielsen K, Vergote I, Op de Beeck K et al (2014) Whole-body MRI with diffusion-weighted sequence for staging of patients with suspected ovarian cancer: a clinical feasibility study in comparison to CT and FDG-PET/CT. Eur Radiol 24:889–901
Low RN, Sebrechts CP, Barone RM, Muller W (2009) Diffusion-weighted MRI of peritoneal tumors: comparison with conventional MRI and surgical and histopathologic findings--a feasibility study. AJR Am J Roentgenol 193:461–470
Low RN, Barone RM, Lucero J (2014) Comparison of MRI and CT for predicting the peritoneal cancer index (PCI) preoperatively in patients being considered for cytoreductive surgical procedures. Ann Surg Oncol. https://doi.org/10.1245/s10434-014-4041-7
Sugarbaker PH (1999) Successful management of microscopic residual disease in large bowel cancer. Cancer Chemother Pharmacol 43(Suppl):S15–S25
Pomel C, Dauplat J (2004) Management of malignant epithelial tumors of the ovary. J Chir (Paris) 141:277–284
Winter WE 3rd, Maxwell GL, Tian C et al (2008) Tumor residual after surgical cytoreduction in prediction of clinical outcome in stage IV epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol 26:83–89
Gong NJ, Wong CS, Chu YC, Guo H, Huang B, Chan Q (2013) Increasing the accuracy of volume and ADC delineation for heterogeneous tumor on diffusion-weighted MRI: correlation with PET/CT. Int J Radiat Oncol Biol Phys 87:407–413
Winfield JM, Wakefield JC, Dolling D et al (2019) Diffusion-weighted MRI in advanced epithelial ovarian cancer: apparent diffusion coefficient as a response marker. Radiology 293:374–383
Tentes AA, Tripsiannis G, Markakidis SK et al (2003) Peritoneal cancer index: a prognostic indicator of survival in advanced ovarian cancer. Eur J Surg Oncol 29:69–73
Engbersen MP, Van TSI, Lok C et al (2019) MRI with diffusion-weighted imaging to predict feasibility of complete cytoreduction with the peritoneal cancer index (PCI) in advanced stage ovarian cancer patients. Eur J Radiol 114:146–151
Gadelhak B, Tawfik AM, Saleh GA et al (2019) Extended abdominopelvic MRI versus CT at the time of adnexal mass characterization for assessing radiologic peritoneal cancer index (PCI) prior to cytoreductive surgery. Abdom Radiol (NY) 44:2254–2261
Horowitz NS, Miller A, Rungruang B et al (2015) Does aggressive surgery improve outcomes? Interaction between preoperative disease burden and complex surgery in patients with advanced-stage ovarian cancer: an analysis of GOG 182. J Clin Oncol 33:937–943
Harter P, Hahmann M, Lueck HJ et al (2009) Surgery for recurrent ovarian cancer: role of peritoneal carcinomatosis: exploratory analysis of the DESKTOP I Trial about risk factors, surgical implications, and prognostic value of peritoneal carcinomatosis. Ann Surg Oncol 16:1324–1330
Kyriazi S, Collins DJ, Messiou C et al (2011) Metastatic ovarian and primary peritoneal cancer: assessing chemotherapy response with diffusion-weighted MR imaging--value of histogram analysis of apparent diffusion coefficients. Radiology 261:182–192
Klumpp B, Schwenzer NF, Gatidis S et al (2014) Assessment of relapse in patients with peritoneal carcinomatosis after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy using F-18-FDG-PET/CT. Rofo 186:359–366
Yu X, Lee EY, Lai V, Chan Q (2014) Correlation between tissue metabolism and cellularity assessed by standardized uptake value and apparent diffusion coefficient in peritoneal metastasis. J Magn Reson Imaging 40:99–105
Espada M, Garcia-Flores JR, Jimenez M et al (2013) Diffusion-weighted magnetic resonance imaging evaluation of intra-abdominal sites of implants to predict likelihood of suboptimal cytoreductive surgery in patients with ovarian carcinoma. Eur Radiol 23:2636–2642
Michielsen K, Dresen R, Vanslembrouck R et al (2017) Diagnostic value of whole body diffusion-weighted MRI compared to computed tomography for pre-operative assessment of patients suspected for ovarian cancer. Eur J Cancer 83:88–98
Funding
Dr. Elaine YP Lee, Dr. Edward S Hui and Prof. Hextan YS Ngan were investigators of the research grant from Health and Medical Research Fund, Hong Kong (No. 03143616), which supported this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Elaine YP LEE.
Conflict of Interest
Dr. Elaine YP Lee, Dr. Edward S Hui and Prof. Hextan YS Ngan were investigators of the research grant from Health and Medical Research Fund, Hong Kong (No. 03143616), which supported this study. The rest of authors have no conflicts of interest to declare.
Statistics and Biometry
No complex statistical methods were necessary for this paper.
Informed Consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical Approval
This prospective cohort study was approved by local Institutional Research Ethics Committee (HKU/HA HKW IRB UW 15-536).
Methodology
• prospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, E.Y.P., An, H., Perucho, J.A.U. et al. Functional tumour burden of peritoneal carcinomatosis derived from DWI could predict incomplete tumour debulking in advanced ovarian carcinoma. Eur Radiol 30, 5551–5559 (2020). https://doi.org/10.1007/s00330-020-06887-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06887-6