Abstract
Objectives
Conventional spin-echo (SE) DWI leads to a fundamental trade-off depending on the b value: high b value provides better lesion contrast-to-noise ratio (CNR) by sacrificing signal-to-noise ratio (SNR), image quality, and quantitative reliability. A stimulated-echo (STE) DWI acquisition is evaluated for high-CNR imaging of prostate cancer while maintaining SNR and reliable apparent diffusion coefficient (ADC) mapping.
Methods
In this prospective, IRB-approved study, 27 patients with suspected prostate cancer (PCa) were scanned with three DWI sequences (SE b = 800 s/mm2, SE b = 1500 s/mm2, and STE b = 800 s/mm2) after informed consent was obtained. ROIs were drawn on biopsy-confirmed cancer and non-cancerous tissue to perform quantitative SNR, CNR, and ADC measurements. Qualitative metrics (SNR, CNR, and overall image quality) were evaluated by three experienced radiologists. Metrics were compared pairwise between the three acquisitions using a t test (quantitative metrics) and Wilcoxon rank test (qualitative metrics).
Results
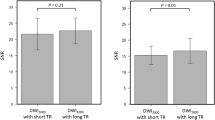
Quantitative measurements showed that STE DWI at b = 800 s/mm2 has significantly better SNR compared to SE DWI at b = 1500 s/mm2 (p < 0.0001) and comparable CNR to high-b value SE DWI at b = 1500 s/mm2 (p < 0.05) in the peripheral zone. Qualitative assessment showed preference to STE b = 800 s/mm2 in SNR and SE b = 1500 s/mm2 in CNR. The overall image quality and lesion detectability among most readers showed no significant preference between STE b = 800 s/mm2 and SE b = 1500 s/mm2. Further, STE DWI had similar ADC contrast between lesion and normal tissue as SE DWI at b = 800 s/mm2 (p = 0.90).
Conclusion
STE DWI has the potential to provide high-SNR, high-CNR imaging of prostate cancer while also enabling reliable ADC mapping.
Key Points
• Quantitative analysis showed that STE DWI at b = 800 s/mm2is able to achieve simultaneously high CNR, high SNR, and reliable ADC mapping, compared to SE b = 800 s/mm2and SE b = 1500 s/mm2.
• Qualitative assessment by three readers showed that STE DWI at b = 800 s/mm2has significantly higher SNR than SE b = 1500 s/mm2. No preference between SE b = 1500 s/mm2and STE b = 800 s/mm2was determined in terms of CNR with no missed lesions were found in both acquisitions.
• A single STE DWI acquisition at moderate b value (800–1000 s/mm2) may provide sufficient image quality and quantitative reliability for prostate cancer imaging within a shorter scan time, in place of two DWI acquisitions (one with moderate b value and one with high b value).






Similar content being viewed by others
Abbreviations
- CNR:
-
Contrast-to-noise radio
- PCa:
-
Prostate cancer
- PZ:
-
Peripheral zone
- SE:
-
Spin-echo
- SNR:
-
Signal-to-noise ratio
- STE:
-
Stimulated-echo
- TE:
-
Echo time
- TM:
-
Mixing time
- TZ:
-
Transition zone
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69(1):7–34
Turkbey B, Rosenkrantz AB, Haider MA et al (2019) Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2. Eur Urol 76(3):340–351
Ahmed HU, Bosaily AE, Brown LC et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389(10071):815–822
Langer DL, Van Der Kwast TH, Evans AJ, Trachtenberg J, Wilson BC, Haider MA (2009) Prostate cancer detection with multi-parametric MRI: logistic regression analysis of quantitative T2, diffusion-weighted imaging, and dynamic contrast-enhanced MRI. J Magn Reson Imaging 30(2):327–334
Tamada T, Kanomata N, Sone T et al (2014) High b value (2000 s/mm2) diffusion-weighted magnetic resonance imaging in prostate cancer at 3 tesla: comparison with 1000 s/mm2 for tumor conspicuity and discrimination of aggressiveness. PLoS One 9(5):3–10
Metens T, Miranda D, Absil J, Matos C (2012) What is the optimal b value in diffusion-weighted MR imaging to depict prostate cancer at 3T? Eur Radiol 22(3):703–709
Itajima KK, Aji YK, Uroda KK, Ugimura KS (2008) High b-value diffusion-weighted imaging in normal and malignant peripheral zone tissue of the prostate: effect of signal-to-noise ratio. Magn Reson Med Sci 7(2):93–99
Xi Y, Liu A, Olumba F et al (2018) Low-to-high b value DWI ratio approaches in multiparametric MRI of the prostate: feasibility, optimal combination of b values, and comparison with ADC maps for the visual presentation of prostate cancer. Quant Imaging Med Surg 8(6):557–567
Agarwal HK, Mertan FV, Sankineni S et al (2017) Optimal high b-value for diffusion weighted MRI in diagnosing high risk prostate cancers in the peripheral zone. J Magn Reson Imaging 45(1):125–131
Tamada T, Sone T, Jo Y, Yamamoto A, Ito K (2014) Diffusion-weighted MRI and its role in prostate cancer. NMR Biomed 27(1):25–38
Gatidis S, Schmidt H, Martirosian P, Nikolaou K, Schwenzer NF (2016) Apparent diffusion coefficient-dependent voxelwise computed diffusion-weighted imaging: an approach for improving SNR and reducing T2 shine-through effects. J Magn Reson Imaging 43(4):824–832
Shio KO, Kuda SO, Hinmoto HS (2016) Removing ambiguity caused by T2 shine-through using weighted diffusion subtraction (WDS). Magn Reson Med Sci 15(1):146–148
Merboldt KD, Hänicke W, Frahm J (1991) Diffusion imaging using stimulated echoes. Magn Reson Med 239:233–239
Zhang Y, Wells SA, Hernando D (2018) Stimulated echo based mapping (STEM) of T1, T2, and apparent diffusion coefficient: validation and protocol optimization. Magn Reson Med 81(1):167–181
Yu AC, Badve C, Ponsky LE et al (2017) Development of a combined MR fingerprinting and diffusion examination for prostate cancer. Radiology 283(3):729–738
Zhang Y, Wells SA, Roldán-alzate A, Hernando D (2019) Simultaneous T1, T2 and ADC mapping in prostate cancer and BPH using STimulated- Echo based Mapping (STEM). 27th ISMRM.
Pena-Nogales O, Zhang Y, Wang X et al (2018) Optimized diffusion-weighting gradient waveform design (ODGD) formulation for motion compensation and concomitant gradient nulling. Magn Reson Med 81:989–1003
Aja-Fernandez S, Pieciak T, Vegas-Sanchez-Ferrero G (2015) Spatially variant noise estimation in MRI: a homomorphic approach. Med Image Anal 20:184–197
Gudbjartsson H, Patz S (1995) The racian distribution of noisy MRI data. Magn Reson Med 34(6):910–914
Mm S, Kitajima K, Takahashi S et al (2012) Clinical utility of apparent diffusion coefficient values obtained using high b-value when diagnosing prostate cancer using 3 tesla MRI: comparison between ultra-high b-value (2000 s/mm2) and standard high b-value (1000 s/mm2). J Magn Reson Imaging 205:198–205
Ueno Y, Kitajima K, Sugimura K et al (2013) Ultra-high b-value diffusion-weighted MRI for the detection of prostate cancer with 3-T MRI. J Magn Reson Imaging 38(1):154–160
Kim CK, Park BK, Kim B (2010) High-b-value diffusion weighted imaging at 3 T to detect prostate cancer: comparisons between b values of 1000 and 2000 s/mm2. AJR Am J Roentgenol 194(1):33–37
Chenevert TL, Lauren D, Taylor JMG et al (2000) Diffusion magnetic resonance imaging: an early surrogate marker of therapeutic efficacy in brain tumors. J Natl Cancer Inst 92(24):2029–2036
Vederine FE, Wessa M, Leboyer M, Houenou J (2011) A meta-analysis of whole-brain diffusion tensor imaging studies in bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry 35(8):1820–1826
Galbán CJ, Hoff BA, Chenevert TL, Ross BD (2017) Diffusion MRI in early cancer therapeutic response assessment. NMR Biomed 30(3). https://doi.org/10.1002/nbm.3458
Feuerlein S, Davenport MS, Krishnaraj A, Merkle EM, Gupta RT (2015) Computed high b-value diffusion-weighted imaging improves lesion contrast and conspicuity in prostate cancer. Prostate Cancer Prostatic Dis 18:155–160
Ning P, Shi D, Sonn GA et al (2018) The impact of computed high b-value images on the diagnostic accuracy of DWI for prostate cancer: a receiver operating characteristics analysis. Sci Rep 8(1):1–9
Barrett T, Priest AN, Lawrence EM et al (2015) Ratio of tumor to normal tissue apparent diffusion coefficient as a method for quantifying DWI of the prostate. AJR Am J Roentgenol 205(6):585–593
Kim CK, Park BK, Kim B (2010) Diffusion-weighted MRI at 3 T for the evaluation of prostate cancer. AJR Am J Roentgenol 194(6):1461–1469
Teruel JR, Cho GY, Moccaldi Rt M et al (2017) Stimulated echo diffusion tensor imaging (STEAM-DTI) with varying diffusion times as a probe of breast tissue. J Magn Reson Imaging 45(1):84–93
von Deuster C, Stoeck CT, Genet M, Atkinson D, Kozerke S (2016) Spin echo versus stimulated echo diffusion tensor imaging of the in vivo human heart. Magn Reson Med 76(3):862–872
Lemberskiy G, Rosenkrantz AB, Veraart J, Taneja SS, Novikov DS, Fieremans E (2017) Time-dependent diffusion in prostate cancer. Invest Radiol 52(7):405–411
Lemberskiy G, Fieremans E, Veraat J, Deng F-M, Rosenkrantz AB, Novikov DS (2018) Characterization of prostate microstructure using water diffusion and NMR relaxation. Front Phys 118(24):6072–6078
Acknowledgments
The authors acknowledge research support from GE Healthcare.
Funding
The authors state that this work has not received any NIH funding.
UW Madison receives research support from GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Diego Hernando, PhD.
Conflict of interest
Dr. Shane Wells is a consultant of Ethicon, Inc.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in an ISMRM abstract.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 465 kb)
Rights and permissions
About this article
Cite this article
Zhang, Y., Wells, S.A., Triche, B.L. et al. Stimulated-echo diffusion-weighted imaging with moderate b values for the detection of prostate cancer. Eur Radiol 30, 3236–3244 (2020). https://doi.org/10.1007/s00330-020-06689-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06689-w