Abstract
Objectives
To investigate CT imaging features associated with poor clinical outcome after corticosteroid treatment in patients diagnosed with cryptogenic organizing pneumonia (COP) and connective tissue disease–related organizing pneumonia (CTD-OP) and to assess the difference in CT findings and treatment responses between COP and CTD-OP.
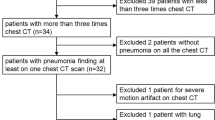
Methods
Chest CT images from 166 patients (COP, 131; CTD-OP, 35) with pathologically proven organizing pneumonia were reviewed by two thoracic radiologists. The type, distribution pattern, and extent of parenchymal abnormalities, along with other associated imaging features, were assessed for each patient. Logistic regression analyses were used to identify features associated with poor clinical outcomes such as residual disease (RD) and disease relapse. The differences between COP and CTD-OP were also analyzed.
Results
Consolidation involving more than 10% of parenchyma (hazard ratio [HR], 2.27), detectable bronchiectasis (HR, 3.59), and diagnosis of CTD-OP (HR, 4.31) were associated with a higher risk of RD after adjustments for patient age and sex. More than 10% consolidation involvement (HR, 2.54) and diagnosis of CTD-OP (HR, 6.42) were also associated with a higher risk of disease relapse. Compared with COP, CTD-OP demonstrated a greater extent of parenchymal abnormalities, especially consolidation, and was less likely to show a peribronchovascular distribution pattern.
Conclusion
Bronchiectasis and a greater extent of consolidation were associated with RD, with the latter also being associated with disease relapse. Compared with COP, CTD-OP was associated with worse treatment outcomes and demonstrated a greater extent of parenchymal abnormalities, which were also less likely to show a peribronchovascular pattern.
Key Points
• The presence of bronchiectasis and a high parenchymal involvement of consolidation on initial chest CT were associated with a worse response to corticosteroids in patients with organizing pneumonia.
• Connective tissue disease–related organizing pneumonia (CTD-OP) was associated with worse treatment outcomes than its idiopathic counterpart cryptogenic organizing pneumonia (COP).
• Compared with COP, CTD-OP generally demonstrated a greater extent of parenchymal abnormalities, especially consolidation, and was less likely to show a peribronchovascular distribution pattern.


Similar content being viewed by others
Abbreviations
- COP:
-
Cryptogenic organizing pneumonia
- CR:
-
Complete recovery
- CTD:
-
Connective tissue disease
- CTD-OP:
-
Connective tissue disease–related organizing pneumonia
- DLCO:
-
Diffusion capacity for carbon monoxide
- FVC:
-
Forced vital capacity
- GGO:
-
Ground-glass opacity
- HR:
-
Hazard ratio
- HRCT:
-
High-resolution computed tomography
- LN:
-
Lymph node
- OP:
-
Organizing pneumonia
- PFT:
-
Pulmonary function test
- RD:
-
Residual disease
- TLC:
-
Total lung capacity
References
Cottin V, Cordier JF (2012) Cryptogenic organizing pneumonia. Semin Respir Crit Care Med 33:462–475
Cordier JF (2000) Organising pneumonia. Thorax 55:318–328
Faria IM, Zanetti G, Barreto MM et al (2015) Organizing pneumonia: chest HRCT findings. J Bras Pneumol 41:231–237
Lee JW, Lee KS, Lee HY et al (2010) Cryptogenic organizing pneumonia: serial high-resolution CT findings in 22 patients. AJR Am J Roentgenol 195:916–922
Lee KS, Kullnig P, Hartman TE, Muller NL (1994) Cryptogenic organizing pneumonia: CT findings in 43 patients. AJR Am J Roentgenol 162:543–546
Oikonomou A, Hansell DM (2002) Organizing pneumonia: the many morphological faces. Eur Radiol 12:1486–1496
Johkoh T, Muller NL, Cartier Y et al (1999) Idiopathic interstitial pneumonias: diagnostic accuracy of thin-section CT in 129 patients. Radiology 211:555–560
Kim SJ, Lee KS, Ryu YH et al (2003) Reversed halo sign on high-resolution CT of cryptogenic organizing pneumonia: diagnostic implications. AJR Am J Roentgenol 180:1251–1254
Torrealba JR, Fisher S, Kanne JP et al (2018) Pathology-radiology correlation of common and uncommon computed tomographic patterns of organizing pneumonia. Hum Pathol 71:30–40
Lazor R, Vandevenne A, Pelletier A, Leclerc P, Court-Fortune I, Cordier JF (2000) Cryptogenic organizing pneumonia. Characteristics of relapses in a series of 48 patients. The Groupe d'Etudes et de Recherche sur les Maladles “Orphelines” Pulmonaires (GERM"O"P). Am J Respir Crit Care Med 162:571–577
Nizami IY, Kissner DG, Visscher DW, Dubaybo BA (1995) Idiopathic bronchiolitis obliterans with organizing pneumonia. An acute and life-threatening syndrome. Chest 108:271–277
Yoo JW, Song JW, Jang SJ et al (2011) Comparison between cryptogenic organizing pneumonia and connective tissue disease-related organizing pneumonia. Rheumatology (Oxford) 50:932–938
Chung MP, Nam BD, Lee KS et al (2018) Serial chest CT in cryptogenic organizing pneumonia: evolutional changes and prognostic determinants. Respirology 23:325–330
Onishi Y, Kawamura T, Nakahara Y et al (2017) Factors associated with the relapse of cryptogenic and secondary organizing pneumonia. Respir Investig 55:10–15
Yoshinouchi T, Ohtsuki Y, Kubo K, Shikata Y (1995) Clinicopathological study on two types of cryptogenic organizing pneumonitis. Respir Med 89:271–278
Tabaj GC, Fernandez CF, Sabbagh E, Leslie KO (2015) Histopathology of the idiopathic interstitial pneumonias (IIP): a review. Respirology 20:873–883
Douglas WW, Tazelaar HD, Hartman TE et al (2001) Polymyositis-dermatomyositis-associated interstitial lung disease. Am J Respir Crit Care Med 164:1182–1185
Epler GR, Colby TV, McLoud TC, Carrington CB, Gaensler EA (1985) Bronchiolitis obliterans organizing pneumonia. N Engl J Med 312:152–158
Kaushik P, Cooper ES, Banda VR, Vatsavai SR, Kaushik R (2005) Bronchiolitis obliterans with organizing pneumonia in rheumatoid arthritis--a fatal case and short review of literature. Rheumatol Int 25:391–393
Kim EA, Lee KS, Johkoh T et al (2002) Interstitial lung diseases associated with collagen vascular diseases: radiologic and histopathologic findings. Radiographics 22 Spec No:S151–S165
Taylor JG, Bolster MB (2003) Bronchiolitis obliterans with organizing pneumonia associated with scleroderma and scleroderma spectrum diseases. J Clin Rheumatol 9:239–245
Drakopanagiotakis F, Paschalaki K, Abu-Hijleh M et al (2011) Cryptogenic and secondary organizing pneumonia: clinical presentation, radiographic findings, treatment response, and prognosis. Chest 139:893–900
Vasu TS, Cavallazzi R, Hirani A, Sharma D, Weibel SB, Kane GC (2009) Clinical and radiologic distinctions between secondary bronchiolitis obliterans organizing pneumonia and cryptogenic organizing pneumonia. Respir Care 54:1028–1032
(2000) American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med 161:646–664
Hansell DM, Bankier AA, MacMahon H, McLoud TC, Muller NL, Remy J (2008) Fleischner Society: glossary of terms for thoracic imaging. Radiology 246:697–722
Zare Mehrjardi M, Kahkouee S, Pourabdollah M (2017) Radio-pathological correlation of organizing pneumonia (OP): a pictorial review. Br J Radiol 90:20160723
Lee JS, Lynch DA, Sharma S, Brown KK, Muller NL (2003) Organizing pneumonia: prognostic implication of high-resolution computed tomography features. J Comput Assist Tomogr 27:260–265
Elicker B, Pereira CA, Webb R, Leslie KO (2008) High-resolution computed tomography patterns of diffuse interstitial lung disease with clinical and pathological correlation. J Bras Pneumol 34:715–744
Lee SM, Seo JB, Yun J et al (2019) Deep learning applications in chest radiography and computed tomography: current state of the art. J Thorac Imaging 34:75–85
Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: images are more than pictures, they are data. Radiology 278:563–577
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Eun Jin Chae.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Cho, Y.H., Chae, E.J., Song, J.W. et al. Chest CT imaging features for prediction of treatment response in cryptogenic and connective tissue disease–related organizing pneumonia. Eur Radiol 30, 2722–2730 (2020). https://doi.org/10.1007/s00330-019-06651-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06651-5