Abstract
Objectives
To identify MRI features that are helpful for the differentiation of gallbladder neuroendocrine tumors (GB-NETs) from gallbladder adenocarcinomas (GB-ADCs) and to evaluate their prognostic values.
Methods
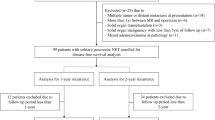
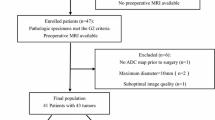
Between January 2008 and December 2018, we retrospectively enrolled patients who underwent MRI for GB malignancy. Two radiologists independently assessed the MRI findings and reached a consensus. Significant MRI features, which distinguish GB-NETs from GB-ADCs, were identified. Cox regression analyses were performed to find MRI features that were prognostic for overall survival.
Results
There were 63 patients with GB-NETs (n = 21) and GB-ADCs (n = 42). Compared with GB-ADCs, GB-NETs more frequently demonstrated the following MRI features: well-defined margins, intact overlying mucosa, and thick rim contrast enhancement and/or diffusion restriction (ps < 0.001). Liver metastases were more common and demonstrated thick rim contrast enhancement and diffusion restriction in GB-NETs (ps < 0.001). Lymph node (LN) metastasis showed thick rim diffusion restriction more often in GB-NETs than in GB-ADCs (p = 0.009). On quantitative analysis, the sizes of the GB mass and metastatic LNs in GB-NETs were larger than those in GB-ADCs (p = 0.002 and p = 0.010, respectively). The ratio of apparent diffusion coefficient values between the lesion and the spleen was lower in the GB mass, liver metastases, and LN metastases of GB-NETs than those of GB-ADCs (p < 0.001, p = 0.017, and p < 0.001, respectively). Survival analysis revealed that a large metastatic LN (hazard ratio 1.737; 95% confidence interval, 1.112–2.712) was the only poor prognostic factor (p = 0.015).
Conclusion
Several MRI features aided in differentiating between GB-NETs and GB-ADCs. A large metastatic LN was associated with poor survival.
Key Points
• Compared with gallbladder adenocarcinomas (GB-ADCs), neuroendocrine tumors (GB-NETs) and their metastases to the liver and lymph nodes more frequently demonstrated a thick rim appearance on contrast-enhanced MRI and diffusion-weighted images.
• The ratio of apparent diffusion coefficient values between the lesion and the spleen was significantly lower for the primary mass, liver metastases, and lymph node metastases of GB-NETs than for those of GB-ADCs.
• A large metastatic lymph node was the only poor prognostic factor for overall survival in patients with GB-NETs and GB-ADCs.






Similar content being viewed by others
Abbreviations
- ADC:
-
Adenocarcinoma
- GB:
-
Gallbladder
- LN:
-
Lymph node
- NET:
-
Neuroendocrine tumor
- OS:
-
Overall survival
References
Duffy A, Capanu M, Abou-Alfa GK et al (2008) Gallbladder cancer (GBC): 10-year experience at Memorial Sloan-Kettering Cancer Centre (MSKCC). J Surg Oncol 98:485–489
American Cancer Society (2017) Cancer Facts & Figures 2017. Atlanta: American Cancer Society
Eltawil KM, Gustafsson BI, Kidd M, Modlin IM (2010) Neuroendocrine tumors of the gallbladder: an evaluation and reassessment of management strategy. J Clin Gastroenterol 44:687–695
Choe J, Kim KW, Kim HJ et al (2019) What is new in the 2017 World Health Organization classification and 8th American Joint Committee on cancer staging system for pancreatic neuroendocrine neoplasms? Korean J Radiol 20:5–17
Oronsky B, Ma PC, Morgensztern D, Carter CA (2017) Nothing but NET: a review of neuroendocrine tumors and carcinomas. Neoplasia 19:991–1002
Soin S, Pannu BS, Myint PT, Dhillon AS (2018) Large cell neuroendocrine carcinoma and adenocarcinoma of gallbladder with concomitant hepatitis C infection. BMJ Case Rep 2018
Jun SR, Lee JM, Han JK, Choi BI (2006) High-grade neuroendocrine carcinomas of the gallbladder and bile duct: report of four cases with pathological correlation. J Comput Assist Tomogr 30:604–609
Adachi T, Haraguchi M, Irie J et al (2016) Gallbladder small cell carcinoma: a case report and literature review. Surg Case Rep 2:71
Wolin EM (2012) The expanding role of somatostatin analogs in the management of neuroendocrine tumors. Gastrointest Cancer Res 5:161–168
Nikou GC, Lygidakis NJ, Toubanakis C et al (2005) Current diagnosis and treatment of gastrointestinal carcinoids in a series of 101 patients: the significance of serum chromogranin-A, somatostatin receptor scintigraphy and somatostatin analogues. Hepatogastroenterology 52:731–741
Kim TH, Kim SH, Lee KB, Han JK (2017) Outcome and CT differentiation of gallbladder neuroendocrine tumours from adenocarcinomas. Eur Radiol 27:507–517
Ayabe RI, Wach M, Ruff S et al (2019) Primary gallbladder neuroendocrine. Insights into a Rare Histology Using a Large National Database. Ann Surg Oncol 26:3577–3585
Smith EH (1991) Complications of percutaneous abdominal fine-needle biopsy. Radiology 178:253–258
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD (2009) Liver biopsy. Hepatology 49:1017–1044
Joo I, Lee JY, Baek JH et al (2014) Preoperative differentiation between T1a and >/=T1b gallbladder cancer: combined interpretation of high-resolution ultrasound and multidetector-row computed tomography. Eur Radiol 24:1828–1834
Yoshimitsu K, Nishihara Y, Okamoto D et al (2012) Magnetic resonance differentiation between T2 and T1 gallbladder carcinoma: significance of subserosal enhancement on the delayed phase dynamic study. Magn Reson Imaging 30:854–859
Kim SJ, Lee JM, Kim H, Yoon JH, Han JK, Choi BI (2013) Role of diffusion-weighted magnetic resonance imaging in the diagnosis of gallbladder cancer. J Magn Reson Imaging 38:127–137
Jeon SK, Lee JM, Joo I et al (2018) Magnetic resonance with diffusion-weighted imaging improves assessment of focal liver lesions in patients with potentially resectable pancreatic cancer on CT. Eur Radiol 28:3484–3493
Lee JH, Han SS, Hong EK et al (2019) Predicting lymph node metastasis in pancreatobiliary cancer with magnetic resonance imaging: a prospective analysis. Eur J Radiol 116:1–7
Ansari NA, Ramalho M, Semelka RC, Buonocore V, Gigli S, Maccioni F (2015) Role of magnetic resonance imaging in the detection and characterization of solid pancreatic nodules: an update. World J Radiol 7:361–374
American College of Radiology (ACR) Liver Imaging Reporting and Data System (LIRADS). Available via https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/LI-RADS. Accessed August 2 2019
Kim B, Lee SS, Sung YS et al (2017) Intravoxel incoherent motion diffusion-weighted imaging of the pancreas: characterization of benign and malignant pancreatic pathologies. J Magn Reson Imaging 45:260–269
Hecht EM, Liu MZ, Prince MR et al (2017) Can diffusion-weighted imaging serve as a biomarker of fibrosis in pancreatic adenocarcinoma? J Magn Reson Imaging 46:393–402
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
El Fattach H, Guerrache Y, Eveno C et al (2015) Primary neuroendocrine tumors of the gallbladder: ultrasonographic and MDCT features with pathologic correlation. Diagn Interv Imaging 96:499–502
Ohtani T, Shirai Y, Tsukada K, Muto T, Hatakeyama K (1996) Spread of gallbladder carcinoma: CT evaluation with pathologic correlation. Abdom Imaging 21:195–201
Pettersson H, Ackerman N, Kaude J et al (1987) Gadolinium-DTPA enhancement of experimental soft tissue carcinoma and hemorrhage in magnetic resonance imaging. Acta Radiol 28:75–78
Deehan DJ, Heys SD, Kernohan N, Eremin O (1993) Carcinoid tumour of the gall bladder: two case reports and a review of published works. Gut 34:1274–1276
Kim SH, Kim SH, Kim MA, Shin CI, Han JK, Choi BI (2015) CT differentiation of poorly-differentiated gastric neuroendocrine tumours from well-differentiated neuroendocrine tumours and gastric adenocarcinomas. Eur Radiol 25:1946–1957
Dromain C, de Baere T, Baudin E et al (2003) MR imaging of hepatic metastases caused by neuroendocrine tumors: comparing four techniques. AJR Am J Roentgenol 180:121–128
Guo C, Chen X, Wang Z et al (2017) Differentiation of pancreatic neuroendocrine carcinoma from pancreatic ductal adenocarcinoma using magnetic resonance imaging: the value of contrast-enhanced and diffusion weighted imaging. Oncotarget 8:42962–42973
Chen C, Wang L, Liu X, Zhang G, Zhao Y, Geng Z (2015) Gallbladder neuroendocrine carcinoma: report of 10 cases and comparison of clinicopathologic features with gallbladder adenocarcinoma. Int J Clin Exp Pathol 8:8218–8226
Yun SP, Shin N, Seo HI (2015) Clinical outcomes of small cell neuroendocrine carcinoma and adenocarcinoma of the gallbladder. World J Gastroenterol 21:269–275
Feinstein AR, Cicchetti DV (1990) High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol 43:543–549
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea [NRF] funded by the Ministry of Science, ICT& Future Planning (NRF-2019R1F1A1060131) and by Seoul National University Hospital Research Fund No. 03-2019-0070.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Joon Koo Han.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Among the 63 patients comprising our study population, 10 patients had been reported in Outcome and CT differentiation of gallbladder neuroendocrine tumours from adenocarcinomas (PMID 27225621).
Methodology
• retrospective
• case-control study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 104 kb)
Rights and permissions
About this article
Cite this article
Bae, J.S., Kim, S.H., Yoo, J. et al. Differential and prognostic MRI features of gallbladder neuroendocrine tumors and adenocarcinomas. Eur Radiol 30, 2890–2901 (2020). https://doi.org/10.1007/s00330-019-06588-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06588-9