Abstract
Objectives
Our aim was to evaluate the contribution of pseudo-continuous arterial spin labelling (pCASL) in the detection of a postoperative residual lesion in adult brain tumours.
Methods
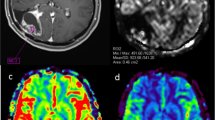
Seventy-five patients were prospectively included. Following the results of preoperative DSC-PWI assessment, intra-axial lesions, including high-grade gliomas (n = 43) and certain metastases (n = 14), were classified as hyper-vascular (HV+ group, n = 57); other lesions, including low-grade gliomas and certain metastases, were classified as non-hyper-vascular (HV− group, n = 18). To confirm the absence/presence of a residual lesion or disease progression, postoperative MRI including pCASL sequence and follow-up-MRI were performed within 72 h and 1–6 months after the resection, respectively. Two raters evaluated the images. Mean and maximal ASL cerebral blood flow (CBF) values were measured in the perioperative region and normalised to the contralateral tissue. The pCASL-CBF maps and post-contrast T1WI were visually assessed for residual lesion. Quantitative data were analysed with unpaired Student t and Mann-Whitney U tests and the visual diagnostic performance with the McNemar test.
Results
In the HV+ group, the mean normalised CBF was 1.97 ± 0.59 and 0.97 ± 0.29 (p < 0.0001, AUC = 0.964, cut-off = 1.27) for patients with or without residual tumours, respectively. The mean normalised CBF was not discriminative for assessing residual tumours in the HV− group (p = 0.454). Visual CBF evaluation allowed 92.98% patients belonging to the HV+ group to be correctly classified (sensitivity 93.02%, specificity 92.86%, p < 0.001). Visual evaluation was correlated with contrast enhancement evaluation and with the mean normalised CBF values (r = 0.505, p < 0.0001 and 0.838, p < 0.0001, respectively).
Conclusion
Qualitative and quantitative ASL evaluation shows high diagnostic performance in postoperative assessment of hyper-perfused tumours. In this case, postoperative pCASL may be useful, especially if contrast injection cannot be performed or when contrast enhancement is doubtful.
Key Points
• Evaluation of postoperative residual lesion in the case of brain tumours is an imaging challenge.
• This prospective monocentric study showed that increased normalised cerebral blood flow assessed by pseudo-continuous arterial spin labelling (pCASL) correlates well with the presence of a residual tumour in the case of hyper-vascular tumour diagnosed on preoperative MRI.
• Qualitative and quantitative pCASL is an informative sequence for hyper-vascular residual tumour, especially if acquired more than 48 h after brain tumour surgery, when contrast enhancement can give ambiguous results due to blood-brain barrier disruption.






Similar content being viewed by others
Abbreviations
- CBF:
-
Cerebral blood flow
- CE-T1WI:
-
Contrast-enhanced T1-weighted imaging
- CInd:
-
Confidence index
- maxrCBF:
-
Normalised ratio for the maximal CBF values
- meanrCBF:
-
Normalised ratio for the mean CBF values
- PRL:
-
Postoperative residual lesion
- visualCBF:
-
Visually assessed CBF
References
Ricard D, Idbaih A, Ducray F, Lahutte M, Hoang-Xuan K, Delattre JY (2012) Primary brain tumours in adults. Lancet 379:1984–1996. https://doi.org/10.1016/S0140-6736(11)61346-9
Cagney DN, Martin AM, Catalano PJ et al (2017) Incidence and prognosis of patients with brain metastases at diagnosis of systemic malignancy: a population-based study. Neuro Oncol 19:1511–1521. https://doi.org/10.1093/neuonc/nox077
Villanueva-Meyer JE, Mabray MC, Cha S (2017) Current clinical brain tumor imaging. Neurosurgery 81:397–415. https://doi.org/10.1093/neuros/nyx103
Weber MA, Zoubaa S, Schlieter M et al (2006) Diagnostic performance of spectroscopic and perfusion MRI for distinction of brain tumors. Cancer Imaging 6:S32–S41. https://doi.org/10.1102/1470-7330.2006.9096
Abrigo JM, Fountain DM, Provenzale JM et al (2018) Magnetic resonance perfusion for differentiating low-grade from high-grade gliomas at first presentation. Cochrane Database Syst Rev 1:CD011551. https://doi.org/10.1002/14651858.CD011551.pub2
Heo YJ, Kim HS, Park JE, Choi CG, Kim SJ (2015) Uninterpretable dynamic susceptibility contrast-enhanced perfusion MR images in patients with post-treatment glioblastomas: Cross-Validation of Alternative Imaging Options. PLoS One 10. https://doi.org/10.1371/journal.pone.0136380
Detre JA, Alsop DC (1999) Perfusion magnetic resonance imaging with continuous arterial spin labeling: methods and clinical applications in the central nervous system. Eur J Radiol 30:115–124
Järnum H, Steffensen EG, Knutsson L et al (2010) Perfusion MRI of brain tumours: a comparative study of pseudo-continuous arterial spin labelling and dynamic susceptibility contrast imaging. Neuroradiology 52:307–317. https://doi.org/10.1007/s00234-009-0616-6
White CM, Pope WB, Zaw T et al (2014) Regional and voxel-wise comparisons of blood flow measurements between dynamic susceptibility contrast magnetic resonance imaging (DSC-MRI) and arterial spin labeling (ASL) in brain tumors. J Neuroimaging 24:23–30. https://doi.org/10.1111/j.1552-6569.2012.00703.x
van Westen D, Petersen ET, Wirestam R et al (2011) Correlation between arterial blood volume obtained by arterial spin labelling and cerebral blood volume in intracranial tumours. MAGMA 24:211–223. https://doi.org/10.1007/s10334-011-0255-x
Noguchi T, Nishihara M, Egashira Y et al (2015) Arterial spin-labeling MR imaging of cerebral hemorrhages. Neuroradiology 57:1135–1144. https://doi.org/10.1007/s00234-015-1574-9
Brown TJ, Brennan MC, Li M et al (2016) Association of the extent of resection with survival in glioblastoma: a systematic review and meta-analysis. JAMA Oncol 2:1460–1469. https://doi.org/10.1001/jamaoncol.2016.1373
Awad A-W, Karsy M, Sanai N et al (2017) Impact of removed tumor volume and location on patient outcome in glioblastoma. J Neurooncol 135:161–171. https://doi.org/10.1007/s11060-017-2562-1
Lee C-H, Kim DG, Kim JW et al (2013) The role of surgical resection in the management of brain metastasis: a 17-year longitudinal study. Acta Neurochir (Wien) 155:389–397. https://doi.org/10.1007/s00701-013-1619-y
Thust SC, Heiland S, Falini A et al (2018) Glioma imaging in Europe: a survey of 220 centres and recommendations for best clinical practice. Eur Radiol. https://doi.org/10.1007/s00330-018-5314-5
Viken HH, Iversen IA, Jakola A, Sagberg LM, Solheim O (2018) When are complications after brain tumor surgery detected? World Neurosurg 112:e702–e710. https://doi.org/10.1016/j.wneu.2018.01.137
Kamp MA, Rapp M, Bühner J et al (2015) Early postoperative magnet resonance tomography after resection of cerebral metastases. Acta Neurochir (Wien) 157:1573–1580. https://doi.org/10.1007/s00701-015-2479-4
Grade M, Hernandez Tamames JA, Pizzini FB, Achten E, Golay X, Smits M (2015) A neuroradiologist’s guide to arterial spin labeling MRI in clinical practice. Neuroradiology 57:1181–1202. https://doi.org/10.1007/s00234-015-1571-z
Sunwoo L, Yun TJ, You S-H et al (2016) Differentiation of glioblastoma from brain metastasis: qualitative and quantitative analysis using arterial spin labeling MR imaging. PLoS One 11:e0166662. https://doi.org/10.1371/journal.pone.0166662
Chawla S, Wang S, Wolf RL et al (2007) Arterial spin-labeling and MR spectroscopy in the differentiation of gliomas. AJNR Am J Neuroradiol 28:1683–1689. https://doi.org/10.3174/ajnr.A0673
Choi YJ, Kim HS, Jahng GH, Kim SJ, Suh DC (2013) Pseudoprogression in patients with glioblastoma: added value of arterial spin labeling to dynamic susceptibility contrast perfusion MR imaging. Acta Radiol 54:448–454. https://doi.org/10.1177/0284185112474916
Lindner T, Ahmeti H, Juhasz J et al (2018) A comparison of arterial spin labeling and dynamic susceptibility perfusion imaging for resection control in glioblastoma surgery. Oncotarget 9:18570–18577. https://doi.org/10.18632/oncotarget.24970
Lindner T, Ahmeti H, Lübbing I et al (2017) Intraoperative resection control using arterial spin labeling - proof of concept, reproducibility of data and initial results. Neuroimage Clin 15:136–142. https://doi.org/10.1016/j.nicl.2017.04.021
Neska-Matuszewska M, Bladowska J, Sąsiadek M, Zimny A (2018) Differentiation of glioblastoma multiforme, metastases and primary central nervous system lymphomas using multiparametric perfusion and diffusion MR imaging of a tumor core and a peritumoral zone—Searching for a practical approach. PLoS One 13. https://doi.org/10.1371/journal.pone.0191341
Sugahara T, Korogi Y, Kochi M et al (1998) Correlation of MR imaging-determined cerebral blood volume maps with histologic and angiographic determination of vascularity of gliomas. AJR Am J Roentgenol 171:1479–1486. https://doi.org/10.2214/ajr.171.6.9843274
Welker K, Boxerman J, Kalnin A et al (2015) ASFNR recommendations for clinical performance of mr dynamic susceptibility contrast perfusion imaging of the brain. AJNR Am J Neuroradiol 36:E41–E51. https://doi.org/10.3174/ajnr.A4341
Rollin N, Guyotat J, Streichenberger N, Honnorat J, Tran Minh VA, Cotton F (2006) Clinical relevance of diffusion and perfusion magnetic resonance imaging in assessing intra-axial brain tumors. Neuroradiology 48:150–159. https://doi.org/10.1007/s00234-005-0030-7
Boxerman JL, Shiroishi MS, Ellingson BM, Pope WB (2016) Dynamic susceptibility contrast mr imaging in glioma: review of current clinical practice. Magn Reson Imaging Clin N Am 24:649–670. https://doi.org/10.1016/j.mric.2016.06.005
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World health organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
You S-H, Yun TJ, Choi HJ et al (2018) Differentiation between primary CNS lymphoma and glioblastoma: qualitative and quantitative analysis using arterial spin labeling MR imaging. Eur Radiol. https://doi.org/10.1007/s00330-018-5359-5
Zeng Q, Jiang B, Shi F, Ling C, Dong F, Zhang J (2017) 3D Pseudocontinuous arterial spin-labeling MR imaging in the preoperative evaluation of gliomas. AJNR Am J Neuroradiol 38:1876–1883. https://doi.org/10.3174/ajnr.A5299
Liu Z-C, Yan L-F, Hu Y-C et al (2017) Combination of IVIM-DWI and 3D-ASL for differentiating true progression from pseudoprogression of glioblastoma multiforme after concurrent chemoradiotherapy: study protocol of a prospective diagnostic trial. BMC Med Imaging 17:10. https://doi.org/10.1186/s12880-017-0183-y
Ye J, Bhagat SK, Li H et al (2016) Differentiation between recurrent gliomas and radiation necrosis using arterial spin labeling perfusion imaging. Exp Ther Med 11:2432–2436. https://doi.org/10.3892/etm.2016.3225
Ata ES, Turgut M, Eraslan C, Dayanır YÖ (2016) Comparison between dynamic susceptibility contrast magnetic resonance imaging and arterial spin labeling techniques in distinguishing malignant from benign brain tumors. Eur J Radiol 85:1545–1553. https://doi.org/10.1016/j.ejrad.2016.05.015
Qiao XJ, Kim HG, Wang DJJ et al (2017) Application of arterial spin labeling perfusion MRI to differentiate benign from malignant intracranial meningiomas. Eur J Radiol 97:31–36. https://doi.org/10.1016/j.ejrad.2017.10.005
Kikuchi K, Hiwatashi A, Togao O et al (2018) Arterial spin-labeling is useful for the diagnosis of residual or recurrent meningiomas. Eur Radiol. https://doi.org/10.1007/s00330-018-5404-4
Grabowski MM, Recinos PF, Nowacki AS et al (2014) Residual tumor volume versus extent of resection: predictors of survival after surgery for glioblastoma. J Neurosurg 121:1115–1123. https://doi.org/10.3171/2014.7.JNS132449
Villanueva-Meyer JE, Han SJ, Cha S, Butowski NA (2017) Early tumor growth between initial resection and radiotherapy of glioblastoma: incidence and impact on clinical outcomes. J Neurooncol 134:213–219. https://doi.org/10.1007/s11060-017-2511-z
Fox BD, Cheung VJ, Patel, Suki D, Rao G (2011) Epidemiology of metastatic brain tumors. Neurosurg Clin N Am 22:1–6, v. https://doi.org/10.1016/j.nec.2010.08.007
Chaichana KL, McGirt MJ, Laterra J, Olivi A, Quiñones-Hinojosa A (2010) Recurrence and malignant degeneration after resection of adult hemispheric low-grade gliomas. J Neurosurg 112:10–17. https://doi.org/10.3171/2008.10.JNS08608
Benveniste RJ, Ferraro N, Tsimpas A (2014) Yield and utility of routine postoperative imaging after resection of brain metastases. J Neurooncol 118:363–367. https://doi.org/10.1007/s11060-014-1440-3
Belhawi SMK, Hoefnagels FWA, Baaijen JC et al (2011) Early postoperative MRI overestimates residual tumour after resection of gliomas with no or minimal enhancement. Eur Radiol 21:1526–1534. https://doi.org/10.1007/s00330-011-2081-y
Smets T, Lawson TM, Grandin C, Jankovski A, Raftopoulos C (2013) Immediate post-operative MRI suggestive of the site and timing of glioblastoma recurrence after gross total resection: a retrospective longitudinal preliminary study. Eur Radiol 23:1467–1477. https://doi.org/10.1007/s00330-012-2762-1
Hirai T, Kitajima M, Nakamura H et al (2011) Quantitative blood flow measurements in gliomas using arterial spin-labeling at 3 T: intermodality agreement and inter- and intraobserver reproducibility study. Am J Neuroradiol 32:2073–2079. https://doi.org/10.3174/ajnr.A2725
Law-Ye B, Schertz M, Galanaud D, Dormont D, Pyatigorskaya N (2017) Arterial spin labeling to predict brain tumor grading: limits of cutoff cerebral blood flow values. Radiology 282:610–612. https://doi.org/10.1148/radiol.2017162312
Kong L, Chen H, Yang Y, Chen L (2017) A meta-analysis of arterial spin labelling perfusion values for the prediction of glioma grade. Clin Radiol 72:255–261. https://doi.org/10.1016/j.crad.2016.10.016
Warmuth C, Gunther M, Zimmer C (2003) Quantification of blood flow in brain tumors: comparison of arterial spin labeling and dynamic susceptibility-weighted contrast-enhanced MR imaging. Radiology 228:523–532. https://doi.org/10.1148/radiol.2282020409
Lescher S, Schniewindt S, Jurcoane, Senft C, Hattingen E (2014) Time window for postoperative reactive enhancement after resection of brain tumors: less than 72 hours. Neurosurg Focus 37:E3. https://doi.org/10.3171/2014.9.FOCUS14479
Gempt J, Förschler A, Buchmann N et al (2013) Postoperative ischemic changes following resection of newly diagnosed and recurrent gliomas and their clinical relevance. J Neurosurg 118:801–808. https://doi.org/10.3171/2012.12.JNS12125
Alsop DC, Detre JA, Golay X et al (2015) Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: a consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med 73:102–116. https://doi.org/10.1002/mrm.25197
Haller S, Zaharchuk G, Thomas DL, Lovblad KO, Barkhof F, Golay X (2016) Arterial spin labeling perfusion of the brain: emerging clinical applications. Radiology 281:337–356. https://doi.org/10.1148/radiol.2016150789
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Nadya Pyatigorskaya.
Conflict of Interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board. All the patients were informed that they could refuse to participate in the study
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 119 kb)
Rights and permissions
About this article
Cite this article
Cohen, C., Law-Ye, B., Dormont, D. et al. Pseudo-continuous arterial spin labelling shows high diagnostic performance in the detection of postoperative residual lesion in hyper-vascularised adult brain tumours. Eur Radiol 30, 2809–2820 (2020). https://doi.org/10.1007/s00330-019-06474-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06474-4