Abstract
Objectives
To provide an indication-based and scanner-specific radiation dose and risk guide for paediatric patients undergoing dental and maxillofacial cone beam computed tomography (CBCT) examinations.
Methods
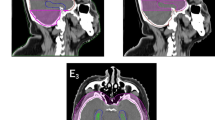
Five commercially available scanners were simulated in EGSnrc Monte Carlo (MC) code. Dedicated, in-house built, head and neck voxel models, each consisting of 22 segmented organs, were used in the study. Organ doses and life attributable risk (LAR) for cancer incidence were assessed for males and females, aged 5 to 14 years old, for every clinically available protocol: central upper and lower incisors, upper and lower premolars, upper and lower jaws, cleft palate, temporal bone, sinus, dentomaxillofacial complex, and face and skull imaging. Dose results were normalised to the x-ray tube load (mAs) and logarithmic curves were fit to organ dose and risk versus age data.
Results
Females demonstrated higher LAR values in all cases. A well-established dose decreasing pattern with increasing age-at-exposure was observed. Central upper incisor protocols were those with the lowest risk, contrary to skull protocols which provided the highest LAR values. Salivary glands and oral mucosa were the highest irradiated organs in all cases, followed by extrathoracic tissue (ET) in protocols where the entire nasal cavity was inside the primary field. The dose to thyroid was considerably high for younger patients.
Conclusions
This work provides an extensive dose assessment guide for 5 dental CBCTs, enabling detailed dose assessment for every paediatric patient.
Key Points
• Radiation dose concerns due to the growing use of paediatric dental and maxillofacial CBCT underline the need for justification that should in part be based on radiation exposure in radiology.
• Patient-specific dose calculations based on Monte Carlo simulations and head-neck paediatric voxel models overcome the limitations of conventional thermoluminescent dosimeter (TLD) dosimetry and provide proper guidance for justification of CBCT exposures.
• Monte Carlo simulations with head-neck models reveal an organ dose and radiation risk decreasing pattern with increasing age at exposure, and with decreasing size of the scanning volume of interest (field of view).

Similar content being viewed by others
Abbreviations
- μGy:
-
Microgray
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional
- CBCT:
-
Cone beam computed tomography
- CLI:
-
Central lower incisors
- CUI:
-
Central upper incisors
- CV:
-
Coefficient of variance
- ED:
-
Effective dose
- ET:
-
Extrathoracic tissue
- FOV:
-
Field of view
- LAR:
-
Life attributable risk
- LJ:
-
Lower jaw
- mAs:
-
Milli ampere second product
- MC:
-
Monte Carlo
- MDCT:
-
Multi-detector computed tomography
- PL:
-
Lower premolar
- PU:
-
Upper premolar
- RBM:
-
Red bone marrow
- SAD:
-
Source to axis of rotation distance
- SDD:
-
Source to detector distance
- Sv:
-
Sievert
- TCM:
-
Tube current modulation
- TLD:
-
Thermoluminescent dosimeter
- ULJ:
-
Upper and lower jaw
References
Miracle AC, Mukherji SK (2009) Cone beam CT of the head and neck, part 2: clinical applications. AJNR Am J Neuroradiol 30:1285–1292
Scarfe WC, Farman AG, Sukovic P (2006) Clinical applications of cone beam computed tomography in dental practice. J Can Dent Assoc 72:75–80
Carter JB, Stone JD, Clark RS, Mercer JE (2016) Applications of cone-beam computed tomography in oral and maxillofacial surgery: an overview of published indications and clinical usage in United States academic centers and oral and maxillofacial surgery practices. J Oral Maxillofac Surg 74(4):668–679
Pauwels R (2015) Cone beam CT for dental and maxillofacial imaging: dose matters. Radiat Prot Dosimetry 165(1–4):156–161
American Dental Association Council on Scientific Affairs (2012) The use of cone-beam tomography in dentistry. An advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 143:899–902
European Commission (2011) Cone beam CT for dental and maxillofacial radiology: evidence based guidelines. Radiation protection publication 172. Available via http://www.sedentexct.eu/files/radiation_protection_172.pdf Last accessed 21 April 2019
Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E (2009) Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 38:187–195
Health Protection Agency (2010) Guidance on the safe use of dental cone beam CT (computed tomography) equipment HPA-CRCE-010. Chilton, Health Protection Agency
Jacobs R (2011) Dental cone beam CT and its justified use in oral health care. JBR-BTR 94(5):254–265
SEDENTEXCT Project (2011) Chapter 4, Justification and referral criteria. Surgical applications. Implant dentistry. In: Radiation protection: cone beam CT for dental and maxillofacial radiology. Evidence based guidelines 2011 (v2.0 Final)
Loubele M, Jacobs R, Maes F et al (2005) Radiation dose vs image quality for low-dose CT protocols of the head for maxillofacial surgery and oral implant planning. Radiat Prot Dosimetry 117(1–3):211–216
Stratis A, Zhang G, Lopez-Rendon X et al (2017) Two examples of indication specific radiation dose calculations in dental CBCT and multidetector CBCT scanners. Phys Med 41:71–77
Ludlow JB, Timothy R, Walker C et al (2015) Effective dose of dental CBCT – a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol 44:20140197
Pauwels R, Binsberger J, Collaert B et al (2012) Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 81:267–271
Ludlow JB, Ivanovic M (2008) Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:106–114
Rottke D, Patzelt S, Poxleitner P, Schulze D (2013) Effective dose span of ten different cone beam CT devices. Dentomaxillofac Radiol 42:20120417
Pauwels R, Theodorakou C, Walker A et al (2012) Dose distribution for dental cone beam CT and its implication for defining a dose index. Dentomaxillofac Radiol 41:583–593
Theodorakou C, Walker A, Horner K et al (2012) Estimation of paediatric organ and effective doses from dental cone beam ct using anthropomorphic phantoms. Br J Radiol 85:153–160
Al Najjar A, Colosi D, Dauer LT et al (2013) Comparison of adult and child equivalent doses from 2 dental cone-beam computed tomography units. Am J Orthod Dentofacial Orthop 143:784–792
Pauwels R, Cockmartin L, Ivanauskaité D et al (2014) Estimating cancer risk from dental cone-beam CT exposure based on skin dosimetry. Phys Med Biol 59:3877–3891
(2007) The 2007 recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP 37(2–4)1–332
Brenner DJ (2008) Effective dose: a flawed concept that could and should be replaced. Br J Radiol 81(967):521–523
Martin CJ (2007) Effective dose: how should it be applied to medical exposures? Br J Radiol 80:639–647
Kawrakow I, Mainegra - Hing E, Rogers DW, Tessier F, Walters BRB (2009) The EGSnrc code system: Monte Carlo simulation of electron and photon transport NRCC report PIRS-701, NRC Canada. Available via https://nrc.canada.ca/en/researchdevelopment/productsservices/software-applications/egsnrc-software-tool-modelradiation-transport Last accessed 21 April 2019
Stratis A, Zhang G, Lopez-Rendon X, Jacobs R, Bogaerts R, Bosmans H (2016) Customization of a Monte Carlo dosimetry tool for dental cone beam CT systems. Radiat Prot Dosimetry 169(1–4):378–385
Zhang G, Pauwels R, Marshall N et al (2011) Development and validation of a hybrid simulation technique for cone beam CT: application to an oral imaging system. Phys Med Biol 56:5823–5843
Zhang G, Marshall N, Bogaerts R, Jacobs R, Bosmans H (2013) Monte Carlo modeling for dose assessment in cone beam CT for oral and maxillofacial applications. Med Phys 40:072103
Turner AC, Zhang D, Kim HJ et al (2009) A method to generate equivalent energy spectra and filtration models based on measurement for multidetector CT Monte Carlo simulations. Med Phys 36:2154–2164
Sempau J, Sanchez-Reyes A, Salvat F, Oulad ben Tahar B, Jiang SB, Fernandez-Varea JM (2001) Monte Carlo simulation of electron beams from an accelerator head using PENELOPE. Phys Med Biol 46:1163–1186
Walters BRB, Kawrakow I, Rogers DWO (2012) History by history statistical estimators in the beam code system. Med Phys 29:2745–2752
Stratis A, Touyz N, Zhang G et al (2017) Development of a paediatric head voxel model database for dosimetric applications. Br J Radiol 90(1078):20170051
Lee C, Lee C, Shah AP, Bolch WE (2006) An assessment of bone marrow and bone endosteum dosimetry methods for photon sources. Phys Med Biol 51:5391–5407
Tapiovaara M, Siiskonen T (2008) PCXMC a Monte Carlo program for calculating patient doses in medical x-ray examinations (2nd edition) STUK-A231, Edita Prima Oy, Helsinki, Finland
(2002) Basic anatomical and physiological data for use in radiological protection reference values. A report of age- and gender-related differences in the anatomical and physiological characteristics of reference individuals. ICRP Publication 89. Ann ICRP 32(3–4)5–265
Menzel HG, Clement C, DeLuca P (2009) ICRP Publication 110. Realistic reference phantoms: an ICRP/ICRU joint effort. A report of adult reference computational phantoms. Ann ICRP 39(2):1–164
Stratis A, Zhang G, Jacobs R, Bogaerts R, Bosmans H (2016) Rotating and translating anthropomorphic head voxel models to establish an horizontal Frankfort plane for dental CBCT Monte Carlo simulations: a dose comparison study. Phys Med Biol 61(24):N681–N696
National Research Council (2006) Health risks from exposure to low levels of ionizing radiation - BEIR VII. The National Academies Press, Washington, DC
Acknowledgements
This work was supported by the European 415 Atomic Energy Community’s Seventh Framework Programme FP7/ 416 2007–2011 under grant agreement No. 604984 (OPERRA: Open 417 Project for the European Radiation Research Area) and by the research fund of KU Leuven (OT/13/109).
Funding
This work was supported by the European 415 Atomic Energy Community’s Seventh Framework Programme FP7/ 416 2007–2011 under grant agreement No. 604984 (OPERRA: Open 417 Project for the European Radiation Research Area) and by the research fund of KU Leuven (OT/13/109).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor is Prof. Dr. Ir. Hilde Bosmans (hilde.bosmans@uzleuven.be).
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study; this study was based on blind CT image datasets, not on patients themselves.
Ethical approval
YES: Commissie Medische Ethiek van de Universitaire Ziekenhuizen KU Leuven, B322201525196.
Methodology
• Retrospective
• Experimental
• Multicentre study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 2547 kb)
Rights and permissions
About this article
Cite this article
Stratis, A., Zhang, G., Jacobs, R. et al. The growing concern of radiation dose in paediatric dental and maxillofacial CBCT: an easy guide for daily practice. Eur Radiol 29, 7009–7018 (2019). https://doi.org/10.1007/s00330-019-06287-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06287-5