Abstract
Objectives
The present study aimed to compare the diagnostic performance of a machine learning (ML)–based FFRCT algorithm, quantified subtended myocardial volume, and high-risk plaque features for predicting if a coronary stenosis is hemodynamically significant, with reference to FFRICA.
Methods
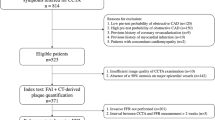
Patients who underwent both CCTA and FFRICA measurement within 2 weeks were retrospectively included. ML-based FFRCT, volume of subtended myocardium (Vsub), percentage of subtended myocardium volume versus total myocardium volume (Vratio), high-risk plaque features, minimal lumen diameter (MLD), and minimal lumen area (MLA) along with other parameters were recorded. Lesions with FFRICA ≤ 0.8 were considered to be functionally significant.
Results
One hundred eighty patients with 208 lesions were included. The lesion length (LL), diameter stenosis, area stenosis, plaque burden, Vsub, Vratio, Vratio/MLD, Vratio/MLA, and LL/MLD4 were all significantly longer or larger in the group of FFRICA ≤ 0.8 while smaller minimal lumen area, MLD, and FFRCT value were noted. The AUC of FFRCT + Vratio/MLD was significantly better than that of FFRCT alone (0.935 versus 0.873, p < 0.001). High-risk plaque features failed to show difference between functionally significant and insignificant groups. Vratio/MLD-complemented ML-based FFRCT for “gray zone” lesions with FFRCT value ranged from 0.7 to 0.8 and the combined use of these two parameters yielded the best diagnostic performance (86.5%, 180/208).
Conclusions
ML-based FFRCT simulation and Vratio/MLD both provide incremental value over CCTA-derived diameter stenosis and high-risk plaque features for predicting hemodynamically significant lesions. Vratio/MLD is more accurate than ML-based FFRCT for lesions with simulated FFRCT value from 0.7 to 0.8.
Key Points
• Machine learning–based FFR CT and subtended myocardium volume both performed well for predicting hemodynamically significant coronary stenosis.
• Subtended myocardium volume was more accurate than machine learning–based FFR CT for “gray zone” lesions with simulated FFR value from 0.7 to 0.8.
• CT-derived high-risk plaque features failed to correctly identify hemodynamically significant stenosis.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- CCTA:
-
Coronary computed tomography angiography
- CFD:
-
Computational fluid dynamics
- DJS:
-
Duke Jeopardy Score
- FFR:
-
Fractional flow reserve
- ICA:
-
Invasive coronary angiography
- LL:
-
Lesion length
- ML:
-
Machine learning
- MLA:
-
Minimal lumen area
- MLD:
-
Minimal lumen diameter
- ROC:
-
Receiver operating characteristic
References
Miller JM, Rochitte CE, Dewey M et al (2008) Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 359(22):2324–2336
Westwood ME, Raatz HD, Misso K et al (2013) Systematic review of the accuracy of dual-source cardiac CT for detection of arterial stenosis in difficult to image patient groups. Radiology 267(2):387–395
Yang L, Zhou T, Zhang R et al (2014) Meta-analysis: diagnostic accuracy of coronary CT angiography with prospective ECG gating based on step-and-shoot, flash and volume modes for detection of coronary artery disease. Eur Radiol 24(10):2345–2352
Toth G, Hamilos M, Pyxaras S et al (2014) Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J 35(40):2831–2838
Tonino PA, Fearon WF, De Bruyne B et al (2010) Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol 55(25):2816–2821
Taylor CA, Fonte TA, Min JK (2013) Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J Am Coll Cardiol 61(22):2233–2241
Nørgaard BL, Leipsic J, Gaur S et al (2014) Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol 63(12):1145–1155
Min JK, Leipsic J, Pencina MJ et al (2012) Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 308:1237–1245
Itu L, Rapaka S, Passerini T et al (2016) A machine-learning approach for computation of fractional flow reserve from coronary computed tomography. J Appl Physiol (1985) 121(1):42–52
Park HB, Heo R, ó Hartaigh B et al (2015) Atherosclerotic plaque characteristics by CT angiography identify coronary lesions that cause ischemia: a direct comparison to fractional flow reserve. JACC Cardiovasc Imaging 8(1):1–10
Driessen RS, Stuijfzand WJ, Raijmakers PG et al (2018) Effect of plaque burden and morphology on myocardial blood flow and fractional flow reserve. J Am Coll Cardiol 71(5):499–509
Califf RM, Phillips HR 3rd, Hindman MC et al (1985) Prognostic value of a coronary artery jeopardy score. J Am Coll Cardiol 5(5):1055–1063
Yu M, Zhao Y, Li W et al (2018) Relationship of the Duke jeopardy score combined with minimal lumen diameter as assessed by computed tomography angiography to the hemodynamic relevance of coronary artery stenosis. J Cardiovasc Comput Tomogr 12(3):247–254
Ide S, Sumitsuji S, Yamaguchi O, Sakata Y (2017) Cardiac computed tomography-derived myocardial mass at risk using the Voronoi-based segmentation algorithm: a histological validation study. J Cardiovasc Comput Tomogr 11(3):179–182
Min JK, Shaw LJ, Devereux RB et al (2007) Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 50:1161–1170
Yu M, Lu Z, Li W, Wei M, Yan J, Zhang J (2018) CT morphological index provides incremental value to machine learning based CT-FFR for predicting hemodynamically significant coronary stenosis. Int J Cardiol 265:256–261
Pijls NH, De Bruyne B, Peels K et al (1996) Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 334(26):1703–1708
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44(3):837–845
Cook CM, Petraco R, Shun-Shin MJ et al (2017) Diagnostic accuracy of computed tomography-derived fractional flow reserve: a systematic review. JAMA Cardiol 2(7):803–810
Tonino PA, De Bruyne B, Pijls NH et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360(3):213–224
De Bruyne B, Pijls NH, Kalesan B et al (2012) Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367(11):991–1001
De Bruyne B, Fearon WF, Pijls NH et al (2014) Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 371(13):1208–1217
Leone AM, De Caterina AR, Basile E et al (2013) Influence of the amount of myocardium subtended by a stenosis on fractional flow reserve. Circ Cardiovasc Interv 6(1):29–36
Ahmadi A, Stone GW, Leipsic J et al (2016) Association of coronary stenosis and plaque morphology with fractional flow reserve and outcomes. JAMA Cardiol 1(3):350–357
Gaur S, Øvrehus KA, Dey D et al (2016) Coronary plaque quantification and fractional flow reserve by coronary computed tomography angiography identify ischaemia-causing lesions. Eur Heart J 13:1220–1227
Waksman R, Legutko J, Singh J et al (2013) FIRST: Fractional Flow Reserve and Intravascular Ultrasound Relationship Study. J Am Coll Cardiol 61:917–923
Brugaletta S, Garcia-Garcia HM, Shen ZJ et al (2012) Morphology of coronary artery lesions assessed by virtual histology intravascular ultrasound tissue characterization and fractional flow reserve. Int J Cardiovasc Imaging 28:221–228
Yu M, Lu Z, Li W et al (2018) Coronary plaque characteristics on baseline CT predict the need for late revascularization in symptomatic patients after percutaneous intervention. Eur Radiol 28(8):3441–3453
Yu M, Li W, Lu Z et al (2018) Quantitative baseline CT plaque characterization of unrevascularized non-culprit intermediate coronary stenosis predicts lesion volume progression and long-term prognosis: a serial CT follow-up study. Int J Cardiol 264:181–186
Ferencik M, Mayrhofer T, Bittner DO et al (2018) Use of high-risk coronary atherosclerotic plaque detection for risk stratification of patients with stable chest pain: a secondary analysis of the PROMISE randomized clinical trial. JAMA Cardiol 3(2):144–152
Guibas L, Stolfi J (1985) Primitives for the manipulation of general subdivisions and the computations of Voronoi diagrams. ACM Trans Graph 4:74–123
Tesche C, De Cecco CN, Baumann S et al (2018) Coronary CT angiography-derived fractional flow reserve: machine learning algorithm versus computational fluid dynamics modeling. Radiology 288(1):64–72
Coenen A, Kim YH, Kruk M et al (2018) Diagnostic accuracy of a machine-learning approach to coronary computed tomographic angiography-based fractional flow reserve: result from the MACHINE consortium. Circ Cardiovasc Imaging 11(6):e007217
Dey D, Gaur S, Ovrehus KA et al (2018) Integrated prediction of lesion-specific ischaemia from quantitative coronary CT angiography using machine learning: a multicentre study. Eur Radiol 28(6):2655–2664
von Knebel Doeberitz PL, De Cecco CN, Schoepf UJ et al (2018) Coronary CT angiography-derived plaque quantification with artificial intelligence CT fractional flow reserve for the identification of lesion-specific ischemia. Eur Radiol. https://doi.org/10.1007/s00330-018-5834-z
Siogkas PK, Anagnostopoulos CD, Liga R et al (2018) Noninvasive CT-based hemodynamic assessment of coronary lesions derived from fast computational analysis: a comparison against fractional flow reserve. Eur Radiol. https://doi.org/10.1007/s00330-018-5781-8
van Hamersvelt RW, Zreik M, Voskuil M, Viergever MA, Išgum I, Leiner T (2018) Deep learning analysis of left ventricular myocardium in CT angiographic intermediate-degree coronary stenosis improves the diagnostic accuracy for identification of functionally significant stenosis. Eur Radiol. https://doi.org/10.1007/s00330-018-5822-3
Funding
This study has received funding from the National Natural Science Foundation of China (Grant No.: 81671678), Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant Support (Grant No.: 20161428), Shanghai Key Discipline of Medical Imaging (No.: 2017ZZ02005), and The National Key Research and Development Program of China (Grant Nos.: 2016YFC1300400 and 2016YFC1300402).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Jiayin Zhang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by hospital IRB.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• comparative study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Yu, M., Lu, Z., Shen, C. et al. The best predictor of ischemic coronary stenosis: subtended myocardial volume, machine learning–based FFRCT, or high-risk plaque features?. Eur Radiol 29, 3647–3657 (2019). https://doi.org/10.1007/s00330-019-06139-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06139-2