Abstract
Objectives
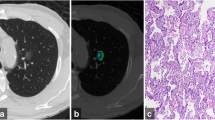
This study aimed to investigate the diagnostic advantage of nodule mass in differentiating invasive pulmonary adenocarcinomas (IPAs) among pure ground-glass nodules (pGGNs) over other volumetric measurements. Another aim of this study was to analyse the correlation between volumetric measurements on computed tomography (CT) scans and the pathological invasive component size.
Methods
This Institutional Review Board-approved retrospective study included 117 patients (men:women = 53:64; mean age, 57.3 years) with 117 pGGNs. Semi-automatic segmentation was performed for all nodules, and volumetric measurements, such as nodule volume, attenuation, mass, two-dimensional (2D) average diameter and three-dimensional (3D) longest diameter, were obtained. Receiver operating characteristic (ROC) curve analyses were performed to evaluate the diagnostic performances of the volumetric parameters in discriminating IPAs. Spearman correlation coefficients were calculated between the volumetric measurements and the invasive component size.
Results
Area under the ROC curve for mass was 0.792 (95% CI, 0.691-0.872) in non-enhanced CT and 0.730 (95% CI, 0.607-0.832) in contrast-enhanced CT. Nodule mass was not superior to 2D average diameter for the differentiation of IPAs in both non-enhanced (0.792 vs 0.780; p = 0.501) CT and contrast-enhanced CT scans (0.730 vs 0.700; p = 0.319). The correlation between the volumetric measurements (mass, 3D longest diameter and 2D average diameter) and the invasive component size was moderate (Spearman’s rho, 0.401-0.422) in non-enhanced CT and weak (Spearman’s rho, 0.276-0.310) in contrast-enhanced CT.
Conclusions
Nodule mass measurement had no strength over other volumetric parameters for the prediction of pathological invasiveness in the diagnosis of pGGNs.
Key Points
• Mass is not superior to other volumetric measurements for the diagnosis of pure ground-glass nodules.
• Mass and two-dimensional average diameter exhibited comparable performance for the discrimination of invasive adenocarcinomas among pure ground-glass nodules.
• The diagnostic performance of volumetric measurements was lower on contrast-enhanced CT scans.
• The correlation between the volumetric measurements and the invasive component size was moderate on non-enhanced CT scans and weak on contrast-enhanced CT scans.


Similar content being viewed by others
Abbreviations
- IPA:
-
Invasive pulmonary adenocarcinoma
- pGGN:
-
Pure ground-glass nodule
- PSN:
-
Part-solid nodule
- SSN:
-
Subsolid nodule
References
Travis WD, Asamura H, Bankier AA et al (2016) The IASLC Lung Cancer Staging Project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol 11:1204–1223
Lee KH, Goo JM, Park SJ et al (2014) Correlation between the size of the solid component on thin-section CT and the invasive component on pathology in small lung adenocarcinomas manifesting as ground-glass nodules. J Thorac Oncol 9:74–82
Ko JP, Suh J, Ibidapo O et al (2016) Lung adenocarcinoma: correlation of quantitative CT findings with pathologic findings. Radiology 280:931–939
Yanagawa M, Johkoh T, Noguchi M et al (2017) Radiological prediction of tumor invasiveness of lung adenocarcinoma on thin-section CT. Medicine (Baltimore) 96:e6331
Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH (2013) Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology 268:265–273
Moon Y, Sung SW, Lee KY, Sim SB, Park JK (2016) Pure ground-glass opacity on chest computed tomography: predictive factors for invasive adenocarcinoma. J Thorac Dis 8:1561–1570
Lim HJ, Ahn S, Lee KS et al (2013) Persistent pure ground-glass opacity lung nodules ≥10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 144:1291–1299
Heidinger BH, Anderson KR, Nemec U et al (2017) Lung adenocarcinoma manifesting as pure ground-glass nodules: correlating CT size, volume, density, and roundness with histopathologic invasion and size. J Thorac Oncol 12:1288–1298
Ding H, Shi J, Zhou X et al (2017) Value of CT characteristics in predicting invasiveness of adenocarcinoma presented as pulmonary ground-glass nodules. Thorac Cardiovasc Surg 65:136–141
Hwang IP, Park CM, Park SJ et al (2015) Persistent pure ground-glass nodules larger than 5 mm: differentiation of invasive pulmonary adenocarcinomas from preinvasive lesions or minimally invasive adenocarcinomas using texture analysis. Invest Radiol 50:798–804
Li Q, Fan L, Cao ET, Li QC, Gu YF, Liu SY (2017) Quantitative CT analysis of pulmonary pure ground-glass nodule predicts histological invasiveness. Eur J Radiol 89:67–71
de Hoop B, Gietema H, van de Vorst S, Murphy K, van Klaveren RJ, Prokop M (2010) Pulmonary ground-glass nodules: increase in mass as an early indicator of growth. Radiology 255:199–206
Cohen JG, Goo JM, Yoo RE et al (2016) Software performance in segmenting ground-glass and solid components of subsolid nodules in pulmonary adenocarcinomas. Eur Radiol 26:4465–4474
Cohen JG, Goo JM, Yoo RE et al (2016) The effect of late-phase contrast enhancement on semi-automatic software measurements of CT attenuation and volume of part-solid nodules in lung adenocarcinomas. Eur J Radiol 85:1174–1180
Cohen JG, Kim H, Park SB et al (2017) Comparison of the effects of model-based iterative reconstruction and filtered back projection algorithms on software measurements in pulmonary subsolid nodules. Eur Radiol 27:3266–3274
Kim H, Park CM, Hwang EJ, Ahn SY, Goo JM (2017) Pulmonary subsolid nodules: value of semi-automatic measurement in diagnostic accuracy, diagnostic reproducibility and nodule classification agreement. Eur Radiol. https://doi.org/10.1007/s00330-017-5171-7
Yoo RE, Goo JM, Hwang EJ et al (2017) Retrospective assessment of interobserver agreement and accuracy in classifications and measurements in subsolid nodules with solid components less than 8mm: which window setting is better? Eur Radiol 27:1369–1376
de Hoop B, Gietema H, van Ginneken B, Zanen P, Groenewegen G, Prokop M (2009) A comparison of six software packages for evaluation of solid lung nodules using semi-automated volumetry: what is the minimum increase in size to detect growth in repeated CT examinations. Eur Radiol 19:800–808
Travis WD, Brambilla E, Noguchi M et al (2011) International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6:244–285
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Karlik SJ (2003) Exploring and summarizing radiologic data. AJR Am J Roentgenol 180:47–54
Das M, Ley-Zaporozhan J, Gietema HA et al (2007) Accuracy of automated volumetry of pulmonary nodules across different multislice CT scanners. Eur Radiol 17:1979–1984
Das M, Muhlenbruch G, Katoh M et al (2007) Automated volumetry of solid pulmonary nodules in a phantom: accuracy across different CT scanner technologies. Invest Radiol 42:297–302
Doo KW, Kang EY, Yong HS, Woo OH, Lee KY, Oh YW (2014) Accuracy of lung nodule volumetry in low-dose CT with iterative reconstruction: an anthropomorphic thoracic phantom study. Br J Radiol 87:20130644
Gietema HA, Wang Y, Xu D et al (2006) Pulmonary nodules detected at lung cancer screening: interobserver variability of semiautomated volume measurements. Radiology 241:251–257
Goodman LR, Gulsun M, Washington L, Nagy PG, Piacsek KL (2006) Inherent variability of CT lung nodule measurements in vivo using semiautomated volumetric measurements. AJR Am J Roentgenol 186:989–994
Revel MP, Lefort C, Bissery A et al (2004) Pulmonary nodules: preliminary experience with three-dimensional evaluation. Radiology 231:459–466
Kim H, Park CM, Woo S et al (2013) Pure and part-solid pulmonary ground-glass nodules: measurement variability of volume and mass in nodules with a solid portion less than or equal to 5 mm. Radiology 269:585–593
Scholten ET, de Hoop B, Jacobs C et al (2013) Semi-automatic quantification of subsolid pulmonary nodules: comparison with manual measurements. PLoS One 8:e80249
Scholten ET, de Jong PA, Jacobs C et al (2015) Interscan variation of semi-automated volumetry of subsolid pulmonary nodules. Eur Radiol 25:1040–1047
Bankier AA, MacMahon H, Goo JM, Rubin GD, Schaefer-Prokop CM, Naidich DP (2017) Recommendations for measuring pulmonary nodules at CT: a statement from the Fleischner Society. Radiology 285:584–600
MacMahon H, Naidich DP, Goo JM et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner society 2017. Radiology 284:228–243
Bae KT (2010) Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology 256:32–61
McDonald JH (2014) Handbook of biological statistics, 3rd edn. Sparky House Publishing, Baltimore
Garzelli L, Goo JM, Ahn SY et al (2018) Improving the prediction of lung adenocarcinoma invasive component on CT: value of a vessel removal algorithm during software segmentation of subsolid nodules. Eur J Radiol 100:58–65
Funding
This study has received funding by a grant from the National R&D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (1520230).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jin Mo Goo.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in journal articles (Eur Radiol 2016, 26:4465-4474; Eur J Radiol 2016, 85:1174-1180; Eur Radiol 2017, 27:3266-3274; Eur Radiol 2017, doi:10.1007/s00330-017-5171-7; Eur Radiol 2017, 27:1369-1376).
Methodology
-
retrospective
-
diagnostic or prognostic study
-
performed at one institution
Electronic supplementary material
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Kim, H., Goo, J.M. & Park, C.M. Evaluation of T categories for pure ground-glass nodules with semi-automatic volumetry: is mass a better predictor of invasive part size than other volumetric parameters?. Eur Radiol 28, 4288–4295 (2018). https://doi.org/10.1007/s00330-018-5440-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5440-0