Abstract
Objectives
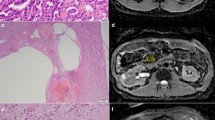
To determine the performance of chemical shift signal intensity index (CS-SII) values for distinguishing minimal-fat renal angiomyolipoma (mfAML) from renal cell carcinoma (RCC) and to assess RCC subtype characterisation.
Methods
We identified eligible studies on CS magnetic resonance imaging (CS-MRI) of focal renal lesions via PubMed, Embase, and the Cochrane Library. CS-SII values were extracted by lesion type and evaluated using linear mixed model-based meta-regression. RCC subtypes were analysed. Two-sided p value <0.05 indicated statistical significance. Methodological quality was assessed using the Quality Assessment of Diagnostic Accuracy Studies 2 tool.
Results
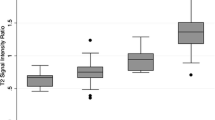
Eleven articles involving 850 patients were included. Minimal-fat AML had significantly higher CS-SII value than RCC (p < 0.05); there were no significant differences between mfAML and clear cell RCC (cc-RCC) (p = 0.112). Clear cell RCC had a significantly higher CS-SII value than papillary RCC (p-RCC) (p < 0.001) and chromophobe RCC (ch-RCC) (p = 0.045). The methodological quality was relatively high, and Begg’s test data points indicated no obvious publication bias.
Conclusions
The CS-SII value for differentiating mfAML from cc-RCC remains unproven, but is a promising method for differentiating cc-RCC from p-RCC and ch-RCC.
Key Points
• RCC CS-SII values are significantly lower than those of mfAML overall.
• CS-SII values cannot aid differentiation between mfAML and cc-RCC.
• CS-SII values might help characterise RCC subtypes.




Similar content being viewed by others
References
Bissler JJ, Kingswood JC (2004) Renal angiomyolipomata. Kidney Int 66:924–934
Bosniak MA, Megibow AJ, Hulnick DH et al (1988) CT diagnosis of renal angiomyolipoma: the importance of detecting small amounts of fat. AJR Am J Roentgenol 151:497–501
Catalano OA, Samir AE, Sahani DV et al (2008) Pixel distribution analysis: can it be used to distinguish clear cell carcinomas from angiomyolipomas with minimal fat? Radiology 247:738–746
Israel GM, Hindman N, Hecht E et al (2005) The use of opposed-phase chemical shift MRI in the diagnosis of renal angiomyolipomas. AJR Am J Roentgenol 184:1868–1872
Jinzaki M, Tanimoto A, Narimatsu Y et al (1997) Angiomyolipoma: imaging findings in lesions with minimal fat. Radiology 205:497–502
Thoenes W, Störkel S, Rumpelt HJ et al (1986) Histopathology and classification of renal cell tumors (adenomas, oncocytomas and carcinomas). The basic cytological and histopathological elements and their use for diagnostics. Pathol Res Pract 181:125–143
O’Toole KM, Brown M, Hoffmann P et al (1993) Pathology of benign and malignant kidney tumors. Urol Clin North Am 20:193–205
Hajdu SI, Savino A, Hajdu EO et al (1971) Cytologic diagnosis of renal cell carcinoma with the aid of fat stain. Acta Cytol 15:31–33
Krishnan B, Truong LD (2002) Renal epithelial neoplasms: the diagnostic implications of electron microscopic study in 55 cases. Hum Pathol 33:68–79
Hood MN, Ho VB, Smirniotopoulos JG et al (1999) Chemical shift: the artifact and clinical tool revisited. Radiographics 19:357–371
Namimoto T, Yamashita Y, Mitsuzaki K et al (2001) Adrenal masses: quantification of fat content with double-echo chemical shift in-phase and opposed-phase FLASH MR images for differentiation of adrenal adenomas. Radiology 218:642–646
Haider MA, Ghai S, Jhaveri K et al (2004) Chemical shift MR imaging of hyperattenuating (10 HU) adrenal asses: does it still have a role? Radiology 231:711–716
Hosokawa Y, Kinouchi T, Sawai Y et al (2002) Renal angiomyolipoma with minimal fat. Int J Clin Oncol 7:120–123
Delfaut EM, Beltran J, Johnson G et al (1999) Fat suppression in MR imaging: techniques and pitfalls. Radiographics 19:373–382
Karlo CA, Donati OF, Burger IA et al (2013) MR imaging of renal cortical tumours: qualitative and quantitative chemical shift imaging parameters. Eur Radiol 23:1738–1744
Outwater EK, Bhatia M, Siegelman ES et al (1997) Lipid in renal clear cell carcinoma: detection on opposed-phase gradient-echo MR images. Radiology 205:103–107
Peng XG, Ju S, Qin Y et al (2011) Quantification of liver fat in mice: comparing dual-echo Dixon imaging, chemical shift imaging, and 1H-MR spectroscopy. J Lipid Res 52:1847–1855
Kim JK, Kim SH, Jang YJ et al (2006) Renal angiomyolipoma with minimal fat: differentiation from other neoplasms at double-echo chemical shift FLASH MR imaging. Radiology 239:174–180
Sasiwimonphan K, Takahashi N, Leibovich BC et al (2012) Small (<4 cm) renal mass: differentiation of angiomyolipoma without visible fat from renal cell carcinoma utilizing MR imaging. Radiology 263:160–168
Hindman N, Ngo L, Genega EM et al (2012) Angiomyolipoma with minimal fat: can it be differentiated from clear cell renal cell carcinoma by using standard MR techniques? Radiology 265:468–477
Ferré R, Cornelis F, Verkarre V et al (2015) Double-echo gradient chemical shift MR imaging fails to differentiate minimal fat renal angiomyolipomas from other homogeneous solid renal tumors. Eur J Radiol 84:360–365
Schieda N, Dilauro M, Moosavi B et al (2016) MRI evaluation of small (<4 cm) solid renal masses: multivariate modeling improves diagnostic accuracy for angiomyolipoma without visible fat compared to univariate analysis. Eur Radiol 26:2242–2251
Park JJ, Kim CK (2017) Small (<4 cm) renal tumors with predominantly low signal intensity on T2-weighted images: differentiation of minimal-fat angiomyolipoma from renal cell carcinoma. AJR Am J Roentgenol 208:124–130
Jhaveri KS, Elmi A, Hosseini-Nik H et al (2015) Predictive value of chemical-shift MRI in distinguishing clear cell renal cell carcinoma from non–clear cell renal cell carcinoma and minimal-fat angiomyolipoma. AJR Am J Roentgenol 205:W79–W86
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Hafron J, Fogarty JD, Hoenig DM et al (2005) Imaging characteristics of minimal fat renal angiomyolipoma with histologic correlations. Urology 66:1155–1159
Milner J, McNeil B, Alioto J et al (2006) Fat poor renal angiomyolipoma: patient, computerized tomography and histological findings. J Urol 176:905–909
Simpfendorfer C, Herts BR, Motta-Ramirez GA et al (2009) Angiomyolipoma with minimal fat on MDCT: can counts of negative-attenuation pixels aid diagnosis? AJR Am J Roentgenol 192:438–443
Roy C, Sauer B, Lindner V et al (2007) MR Imaging of papillary renal neoplasms: potential application for characterization of small renal masses. Eur Radiol 17:193–200
Pedrosa I, Sun MR, Spencer M et al (2008) MR imaging of renal masses: correlation with findings at surgery and pathologic analysis. Radiographics 28:985–1003
Kohl CA, Chivers FS, Lorans R et al (2014) Accuracy of chemical shift MR imaging in diagnosing indeterminate bone marrow lesions in the pelvis: review of a single institution's experience. Skelet Radiol 43:1079–1084
Wang X, Hernando D, Reeder SB et al (2016) Sensitivity of chemical shift-encoded fat quantification to calibration of fat MR spectrum. Magn Reson Med 75:845–851
Priola AM, Priola SM, Ciccone G et al (2015) Differentiation of rebound and lymphoid thymic hyperplasia from anterior mediastinal tumors with dual echo chemical-shift MR imaging in adulthood: reliability of the chemical shift ratio and signal intensity index. Radiology 274:238–249
Tsushima Y, Ishizaka H, Matsumoto M et al (2015) Adrenal masses: differentiation with chemical shift, fast low-angle shot MR imaging. Radiology 186:705–709
Fujiyoshi F, Nakajo M, Fukukura Y et al (2003) Characterization of adrenal tumors by chemical shift fast low-angle shot MR imaging: comparison of four methods of quantitative evaluation. AJR Am J Roentgenol 180:1649–1657
Reuter VE (2003) The pathology of renal epithelial neoplasms. Semin Oncol 33:534–543
Lim RS, Flood TA, McInnes MDF et al (2017) Renal angiomyolipoma without visible fat: Can we make the diagnosis using CT and MRI? Eur Radiol. https://doi.org/10.1007/s 00330-017-4988-4
Kang SK, Huang WC, Pandharipande PV et al (2014) Solid renal masses: what the numbers tell us. AJR Am J Roentgenol 202:1196–1206
Amin MB, Amin MB, Tamboli P et al (2002) Prognostic impact of histologic subtyping of adult renal epithelial neoplasms: an experience of 405 cases. Am J Surg Pathol 26:281–291
Cheville JC, Lohse CM, Zincke H et al (2002) Comparisons of outcome and prognostic features among histologic subtypes of renal cell carcinoma. Am J Surg Pathol 27:612–624
Delahunt B, Bethwaite PB, Nacey JN (2007) Outcome prediction for renal cell carcinoma: evaluation of prognostic factors for tumours divided according to histological subtype. Pathology 39:459–465
Escudier B, Eisen T, Stadler WM et al (2007) Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356:125–134
Motzer RJ, Hutson TE, Tomczak P et al (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356:115–124
Chowdhury S, Choueiri TK (2009) Recent advances in the systemic treatment of metastatic papillary renal cancer. Expert Rev Anticancer Ther 9:373–379
Sun MR, Ngo L, Genega EM et al (2009) Renal cell carcinoma: dynamic contrast -enhanced MR imaging for differentiation of tumor subtypes—correlation with pathologic findings. Radiology 250:793–802
Mytsyk Y, Dutka I, Borys Y et al (2016) Renal cell carcinoma: applicability of the apparent coefficient of the diffusion‑weighted estimated by MRI for improving their differential diagnosis, histologic subtyping, and differentiation grade. Int Urol Nephrol 49:215–224
Pedrosa I, Chou MT, Ngo L et al (2007) MR classification of renal masses with pathologic correlation. Eur Radiol 18:365–375
Childs DD, Clingan MJ, Zagoria RJ et al (2014) In-phase signal intensity loss in solid renal masses on dual-echo gradient-echo MRI: association with malignancy and pathologic classification. AJR Am J Roentgenol 203:W421–W428
Yoshimitsu K, Kakihara D, Irie H et al (2006) Papillary renal carcinoma: diagnostic approach by chemical shift gradient echo and echo-planar MR imaging. J Magn Reson Imaging 23:339–344
Funding
This study has received funding by the National Natural Science Foundation of China (81471705).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Zhong-Qiu Wang, MD, PhD, (Department of Radiology, Affiliated Hospital of Nanjing University of CM, Nanjing 210029, China).
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Pin Wang, PhD, (Department of Endocrinology, Sichuan Academy of Medical Science and Sichuan Provincial People’s Hospital, Chengdu, Sichuan, China) kindly provided statistical advice for this manuscript.
Ethical approval
Institutional Review Board approval was not required because we only performed data analysis based on the published studies.
Informed consent
Informed consent was not required because this is a meta-analysis of several published papers and therefore data of our cohorts have been published already in these papers.
Methodology
• Diagnostic or prognostic study
• Performed at one institution
Rights and permissions
About this article
Cite this article
Chen, LS., Zhu, ZQ., Wang, ZT. et al. Chemical shift magnetic resonance imaging for distinguishing minimal-fat renal angiomyolipoma from renal cell carcinoma: a meta-analysis. Eur Radiol 28, 1854–1861 (2018). https://doi.org/10.1007/s00330-017-5141-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5141-0