Abstract
Objectives
To evaluate the clinical course of disappearing colorectal liver metastases (DLM) or residual tiny (≤5 mm) colorectal liver metastases (RTCLM) on gadoxetic acid-enhanced magnetic resonance imaging (MRI) and diffusion-weighted imaging (DWI) in patients who had colorectal liver metastases (CLM) and received chemotherapy.
Methods
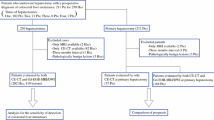
Among 137 patients who received chemotherapy for CLM and underwent gadoxetic acid-enhanced MRI and DWI between 2010 and 2012, 43 patients with 168 DLMs and 48 RTCLMs were included. The cumulative in situ recurrence rate of DLM and progression rate of RTCLM and their predictive factors were evaluated.
Results
A total of 150 DLMs and 26 RTCLMs were followed up without additional treatment. At 1 and 2 years, respectively, the cumulative in situ recurrence rates for DLM were 10.9 % and 15.7 % and the cumulative progression rates for RTCLM were 27.2 % and 33.2 %. The in situ recurrence rate at 2 years was 4.9 % for the DLM group that did not show reticular hypointensity of liver parenchyma on hepatobiliary phase.
Conclusions
DLM on gadoxetic acid-enhanced liver MRI and DWI indicates a high possibility of clinical complete response, especially in patients without chemotherapy-induced sinusoidal obstruction syndrome. Thirty-three percent of RTCLMs showed progression at 2 years.
Key Points
• DLMs on gadoxetic acid-enhanced MRI and DWI showed low recurrence rates.
• If there is sinusoidal obstruction syndrome, evaluation of DLM needs special care.
• The progression rate for residual tiny CLMs was 33.2 % at 2 years.





Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- CLM:
-
Colorectal liver metastases
- CR:
-
Complete response
- CT:
-
Computed tomography
- DLM:
-
Disappearing liver metastases
- DWI:
-
Diffusion-weighted imaging
- MRI:
-
Magnetic resonance imaging
- RTCLM:
-
Residual tiny colorectal liver metastases
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, Bouvier AM (2006) Epidemiology and management of liver metastases from colorectal cancer. Ann Surg 244:254–259
Scheele J, Stang R, Altendorf-Hofmann A, Paul M (1995) Resection of colorectal liver metastases. World J Surg 19:59–71
Zavadsky KE, Lee YT (1994) Liver metastases from colorectal carcinoma: incidence, resectability, and survival results. Am Surg 60:929–933
Chua TC, Saxena A, Liauw W, Kokandi A, Morris DL (2010) Systematic review of randomized and nonrandomized trials of the clinical response and outcomes of neoadjuvant systemic chemotherapy for resectable colorectal liver metastases. Ann Surg Oncol 17:492–501
Benoist S, Brouquet A, Penna C et al (2006) Complete response of colorectal liver metastases after chemotherapy: does it mean cure? J Clin Oncol 24:3939–3945
Kim HJ, Lee SS, Byun JH et al (2015) Incremental value of liver MR imaging in patients with potentially curable colorectal hepatic metastasis detected at CT: a prospective comparison of diffusion-weighted imaging, gadoxetic acid-enhanced MR imaging, and a combination of both MR techniques. Radiology 274:712–722
Scharitzer M, Ba-Ssalamah A, Ringl H et al (2013) Preoperative evaluation of colorectal liver metastases: comparison between gadoxetic acid-enhanced 3.0-T MRI and contrast-enhanced MDCT with histopathological correlation. Eur Radiol 23:2187–2196
Muhi A, Ichikawa T, Motosugi U et al (2011) Diagnosis of colorectal hepatic metastases: comparison of contrast-enhanced CT, contrast-enhanced US, superparamagnetic iron oxide-enhanced MRI, and gadoxetic acid-enhanced MRI. J Magn Reson Imaging 34:326–335
Owen JW, Fowler KJ, Doyle MB, Saad NE, Linehan DC, Chapman WC (2016) Colorectal liver metastases: disappearing lesions in the era of Eovist hepatobiliary magnetic resonance imaging. HPB (Oxford) 18:296–303
Kim A, Lee CH, Kim BH et al (2012) Gadoxetic acid-enhanced 3.0T MRI for the evaluation of hepatic metastasis from colorectal cancer: metastasis is not always seen as a "defect" on the hepatobiliary phase. Eur J Radiol 81:3998–4004
Lee EW, Wei LJ, Amato DA (1992) Cox-type regression analysis for large number of small groups of correlated failure time observations. In: Klein JP, Goel PK (eds) Survival analysis, state of the art. Kluwer Academic Publishers, Dordrecht, pp 237–247
Auer RC, White RR, Kemeny NE et al (2010) Predictors of a true complete response among disappearing liver metastases from colorectal cancer after chemotherapy. Cancer 116:1502–1509
Elias D, Goere D, Boige V et al (2007) Outcome of posthepatectomy-missing colorectal liver metastases after complete response to chemotherapy: impact of adjuvant intra-arterial hepatic oxaliplatin. Ann Surg Oncol 14:3188–3194
Elias D, Youssef O, Sideris L et al (2004) Evolution of missing colorectal liver metastases following inductive chemotherapy and hepatectomy. J Surg Oncol 86:4–9
Tanaka K, Takakura H, Takeda K, Matsuo K, Nagano Y, Endo I (2009) Importance of complete pathologic response to prehepatectomy chemotherapy in treating colorectal cancer metastases. Ann Surg 250:935–942
van Vledder MG, de Jong MC, Pawlik TM, Schulick RD, Diaz LA, Choti MA (2010) Disappearing colorectal liver metastases after chemotherapy: should we be concerned? J Gastrointest Surg 14:1691–1700
Gaujoux S, Goere D, Dumont F et al (2011) Complete radiological response of colorectal liver metastases after chemotherapy: what can we expect? Dig Surg 28:114–120
Yu MH, Lee JM, Hur BY et al (2015) Gadoxetic acid-enhanced MRI and diffusion-weighted imaging for the detection of colorectal liver metastases after neoadjuvant chemotherapy. Eur Radiol 25:2428–2436
Kim YK, Lee MW, Lee WJ et al (2012) Diagnostic accuracy and sensitivity of diffusion-weighted and of gadoxetic acid-enhanced 3-T MR imaging alone or in combination in the detection of small liver metastasis (</= 1.5 cm in diameter). Investig Radiol 47:159–166
Koh DM, Collins DJ, Wallace T, Chau I, Riddell AM (2012) Combining diffusion-weighted MRI with Gd-EOB-DTPA-enhanced MRI improves the detection of colorectal liver metastases. Br J Radiol 85:980–989
Macera A, Lario C, Petracchini M et al (2013) Staging of colorectal liver metastases after preoperative chemotherapy. Diffusion-weighted imaging in combination with Gd-EOB-DTPA MRI sequences increases sensitivity and diagnostic accuracy. Eur Radiol 23:739–747
Shin NY, Kim MJ, Lim JS et al (2012) Accuracy of gadoxetic acid-enhanced magnetic resonance imaging for the diagnosis of sinusoidal obstruction syndrome in patients with chemotherapy-treated colorectal liver metastases. Eur Radiol 22:864–871
Tamandl D, Klinger M, Eipeldauer S et al (2011) Sinusoidal obstruction syndrome impairs long-term outcome of colorectal liver metastases treated with resection after neoadjuvant chemotherapy. Ann Surg Oncol 18:421–430
Angliviel B, Benoist S, Penna C et al (2009) Impact of chemotherapy on the accuracy of computed tomography scan for the evaluation of colorectal liver metastases. Ann Surg Oncol 16:1247–1253
Aloysius MM, Zaitoun AM, Beckingham IJ et al (2007) The pathological response to neoadjuvant chemotherapy with FOLFOX-4 for colorectal liver metastases: a comparative study. Virchows Arch 451:943–948
Acknowledgements
The scientific guarantor of this publication is Won Jae Lee, the head of radiology department. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. Kyung A. Kim from the Center for Biostatistics and Clinical Epidemiology (Samsung Medical Center) kindly provided statistical advice for this manuscript. This study was performed on human subjects. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. No study subjects or cohorts have been previously reported. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S.S., Song, K.D., Kim, Y.K. et al. Disappearing or residual tiny (≤5 mm) colorectal liver metastases after chemotherapy on gadoxetic acid-enhanced liver MRI and diffusion-weighted imaging: Is local treatment required?. Eur Radiol 27, 3088–3096 (2017). https://doi.org/10.1007/s00330-016-4644-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4644-4