Abstract
Objectives
To evaluate the longitudinal risk to patients with cirrhosis of hypervascular hepatocellular carcinoma (HCC) developing from hypovascular hepatic nodules that show positive uptake of gadoxetic acid (hyperintensity) on hepatocyte phase images.
Methods
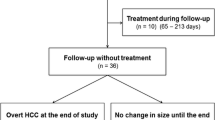
In 69 patients, we evaluated findings from serial follow-up examinations of 633 hepatic nodules that appeared hypovascular and hyperintense on initial gadoxetic acid-enhanced magnetic resonance imaging (EOB-MRI) until the nodules demonstrated hypervascularity and were diagnosed as hypervascular HCC. Cox analyses were performed to identify risk factors for the development of hypervascular HCCs from the nodules.
Results
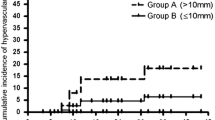
The median follow-up was 663 days (range, 110 to 1215 days). Hypervascular HCCs developed in six of the 633 nodules (0.9 %) in five of the 69 patients. The only independent risk factor, the nodule’s initial maximum diameter of 10 mm or larger, demonstrated a hazard ratio of 1.25. The one-year risk of hypervascular HCC developing from a nodule was 0.44 %. The risk was significantly higher for nodules of larger diameter (1.31 %) than those smaller than 10 mm (0.10 %, p < 0.01).
Conclusions
Hypervascular HCC rarely develops from hypovascular, hyperintense hepatic nodules. We observed low risk even for nodules of 10 mm and larger diameter at initial examination.
Key Points
• Hypervascularization was rare on follow-up examination of hypovascular, hyperintense nodules
• The risk of hypervascularization in a nodule increased with large size
• Hypovascular, hyperintense nodules require neither treatment nor more intense follow-up



Similar content being viewed by others
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- AFP:
-
Alpha-fetoprotein
- CE-CT:
-
Contrast-enhanced computed tomography
- CT:
-
Computed tomography
- CTAP:
-
Computed tomography during arterial portography
- CTHA:
-
Computed tomography during hepatic arteriography
- DN:
-
Dysplastic nodule
- HCC:
-
Hepatocellular carcinoma
- HP:
-
Hepatocyte phase
- MRI:
-
Magnetic resonance imaging
- OATP:
-
Organic anion transporter
- PIVKA-II:
-
Protein induced by vitamin K absence or antagonist II
- T1WI:
-
T1-weighted imaging
- T2WI:
-
T2-weighted imaging
References
International Consensus Group for Hepatocellular Neoplasia (2009) Pathologic diagnosis of early hepatocellular carcinoma: a report of the International Consensus Group for Hepatocellular Neoplasia. Hepatology 49:658–664
Takayama T, Makuuchi M, Hirohashi S et al (1990) Malignant transformation of adenomatous hyperplasia to hepatocellular carcinoma. Lancet 336:1150–1153
Kitao A, Zen Y, Matsui O, Gabata T, Nakanuma Y (2009) Hepatocarcinogenesis: multistep changes of drainage vessels at CT during arterial portography and hepatic arteriography--radiologic-pathologic correlation. Radiology 252:605–614
Huppertz A, Haraida S, Kraus A et al (2005) Enhancement of focal liver lesions at gadoxetic acid-enhanced MR imaging: correlation with histopathologic findings and spiral CT--initial observations. Radiology 234:468–478
Motosugi U, Ichikawa T, Sou H et al (2010) Distinguishing hypervascular pseudolesions of the liver from hypervascular hepatocellular carcinomas with gadoxetic acid-enhanced MR imaging. Radiology 256:151–158
Jung G, Breuer J, Poll LW et al (2006) Imaging characteristics of hepatocellular carcinoma using the hepatobiliary contrast agent Gd-EOB-DTPA. Acta Radiol 47:15–23
Neri E, Bali MA, Ba-Ssalamah A et al (2016) ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur Radiol 26:921–931
Ahn SS, Kim MJ, Lim JS, Hong HS, Chung YE, Choi JY (2010) Added value of gadoxetic acid-enhanced hepatobiliary phase MR imaging in the diagnosis of hepatocellular carcinoma. Radiology 255:459–466
Motosugi U, Ichikawa T, Araki T (2013) Rules, roles, and room for discussion in gadoxetic acid-enhanced magnetic resonance liver imaging: current knowledge and future challenges. Magn Reson Med Sci 12:161–175
Inoue T, Kudo M, Komuta M et al (2012) Assessment of Gd-EOB-DTPA-enhanced MRI for HCC and dysplastic nodules and comparison of detection sensitivity versus MDCT. J Gastroenterol 47:1036–1047
Ichikawa T, Saito K, Yoshioka N et al (2010) Detection and characterization of focal liver lesions: a Japanese phase III, multicenter comparison between gadoxetic acid disodium-enhanced magnetic resonance imaging and contrast-enhanced computed tomography predominantly in patients with hepatocellular carcinoma and chronic liver disease. Investig Radiol 45:133–141
Golfieri R, Grazioli L, Orlando E et al (2012) Which is the best MRI marker of malignancy for atypical cirrhotic nodules: hypointensity in hepatobiliary phase alone or combined with other features? Classification after Gd-EOB-DTPA administration. J Magn Reson Imaging 36:648–657
Sano K, Ichikawa T, Motosugi U et al (2011) Imaging study of early hepatocellular carcinoma: usefulness of gadoxetic acid-enhanced MR imaging. Radiology 261:834–844
Motosugi U, Ichikawa T, Sano K et al (2011) Outcome of hypovascular hepatic nodules revealing no gadoxetic acid uptake in patients with chronic liver disease. J Magn Reson Imaging 34:88–94
Kumada T, Toyoda H, Tada T et al (2011) Evolution of hypointense hepatocellular nodules observed only in the hepatobiliary phase of gadoxetate disodium-enhanced MRI. AJR Am J Roentgenol 197:58–63
Hyodo T, Murakami T, Imai Y et al (2013) Hypovascular nodules in patients with chronic liver disease: risk factors for development of hypervascular hepatocellular carcinoma. Radiology 266:480–490
Kim YK, Lee WJ, Park MJ, Kim SH, Rhim H, Choi D (2012) Hypovascular hypointense nodules on hepatobiliary phase gadoxetic acid-enhanced MR images in patients with cirrhosis: potential of DW imaging in predicting progression to hypervascular HCC. Radiology 265:104–114
Kim YS, Song JS, Lee HK, Han YM (2015) Hypovascular hypointense nodules on hepatobiliary phase without T2 hyperintensity on gadoxetic acid-enhanced MR images in patients with chronic liver disease: long-term outcomes and risk factors for hypervascular transformation. Eur Radiol. doi:10.1007/s00330-015-4146-9
Higaki A, Ito K, Tamada T et al (2014) Prognosis of small hepatocellular nodules detected only at the hepatobiliary phase of Gd-EOB-DTPA-enhanced MR imaging as hypointensity in cirrhosis or chronic hepatitis. Eur Radiol 24:2476–2481
Chen N, Motosugi U, Sano K et al (2013) Early hepatocellular carcinomas showing isointensity or hyperintensity in gadoxetic acid-enhanced, hepatocyte-phase magnetic resonance images. J Comput Assist Tomogr 37:466–469
Kanata N, Yoshikawa T, Ohno Y et al (2013) HCC-to-liver contrast on arterial-dominant phase images of EOB-enhanced MRI: comparison with dynamic CT. Magn Reson Imaging 31:17–22
Kudo M, Matsui O, Izumi N, Iijima H, Kadoya M, Imai Y (2014) Surveillance and diagnostic algorithm for hepatocellular carcinoma proposed by the Liver Cancer Study Group of Japan: 2014 update. Oncology 87:7–21
Imai Y, Murakami T, Hori M et al (2008) Hypervascular hepatocellular carcinoma: combined dynamic MDCT and SPIO-enhanced MRI versus combined CTHA and CTAP. Hepatol Res 38:147–158
Bruix J, Sherman M, American Association for the Study of Liver Diseases (2011) Management of hepatocellular carcinoma: an update. Hepatology 53:1020–1022
European Association for the Study of the Liver, European Organisation for Research and Treatment of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Murakami T, Oi H, Hori M et al (1997) Helical CT during arterial portography and hepatic arteriography for detecting hypervascular hepatocellular carcinoma. AJR Am J Roentgenol 169:131–135
Matsui O, Takashima T, Kadoya M et al (1985) Dynamic computed tomography during arterial portography: the most sensitive examination for small hepatocellular carcinomas. J Comput Assist Tomogr 9:19–24
Miyayama S, Matsui O, Yamashiro M et al (2009) Detection of hepatocellular carcinoma by CT during arterial portography using a cone-beam CT technology: comparison with conventional CTAP. Abdom Imaging 34:502–506
Merine D, Takayasu K, Wakao F (1990) Detection of hepatocellular carcinoma: comparison of CT during arterial portography with CT after intraarterial injection of iodized oil. Radiology 175:707–710
Van Beers BE, Pastor CM, Hussain HK (2012) Primovist, Eovist: what to expect? J Hepatol 57:421–429
Bartolozzi C, Battaglia V, Bargellini I et al (2013) Contrast-enhanced magnetic resonance imaging of 102 nodules in cirrhosis: correlation with histological findings on explanted livers. Abdom Imaging 38:290–296
Yoshida H, Shiratori Y, Moriyama M et al (1999) Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med 131:174–181
Tsukuma H, Hiyama T, Tanaka S et al (1993) Risk factors for hepatocellular carcinoma among patients with chronic liver disease. N Engl J Med 328:1797–1801
Motosugi U, Bannas P, Sano K, Reeder SB (2015) Hepatobiliary MR contrast agents in hypovascular hepatocellular carcinoma. J Magn Reson Imaging 41:251–265
Tsuboyama T, Onishi H, Kim T et al (2010) Hepatocellular carcinoma: hepatocyte-selective enhancement at gadoxetic acid-enhanced MR imaging--correlation with expression of sinusoidal and canalicular transporters and bile accumulation. Radiology 255:824–833
Kitao A, Zen Y, Matsui O et al (2010) Hepatocellular carcinoma: signal intensity at gadoxetic acid-enhanced MR imaging--correlation with molecular transporters and histopathologic features. Radiology 256:817–826
Kitao A, Matsui O, Yoneda N et al (2012) Hypervascular hepatocellular carcinoma: correlation between biologic features and signal intensity on gadoxetic acid-enhanced MR images. Radiology 265:780–789
Choi JW, Lee JM, Kim SJ et al (2013) Hepatocellular carcinoma: imaging patterns on gadoxetic acid-enhanced MR images and their value as an imaging biomarker. Radiology 267:776–786
Beasley RP, Hwang LY, Lin CC, Chien CS (1981) Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet 2:1129–1133
Liang TJ, Jeffers LJ, Reddy KR et al (1993) Viral pathogenesis of hepatocellular carcinoma in the United States. Hepatology 18:1326–1333
Tateishi R, Yoshida H, Matsuyama Y, Mine N, Kondo Y, Omata M (2008) Diagnostic accuracy of tumor markers for hepatocellular carcinoma: a systematic review. Hepatol Int 2:17–30
Chang KC, Lu SN, Chen PF et al (2011) Incidence and associated risk factors of hepatocellular carcinoma in a dural hepatitis B and C virus endemic area: a surveillance study. Kaohsiung J Med Sci 27:85–90
Lok AS, Seeff LB, Morgan TR et al (2009) Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advanced liver disease. Gastroenterology 136:138–148
Acknowledgments
The scientific guarantor of this publication is Tomoaki Ichikawa. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding.
No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board.
Methodology: retrospective, diagnostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sano, K., Ichikawa, T., Motosugi, U. et al. Outcome of hypovascular hepatic nodules with positive uptake of gadoxetic acid in patients with cirrhosis. Eur Radiol 27, 518–525 (2017). https://doi.org/10.1007/s00330-016-4423-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4423-2