Abstract
Objectives
Quantitative evaluation of hemodynamic characteristics of arteriovenous and venous malformations using time-resolved magnetic resonance angiography (MRA) at 3.0 Tesla.
Methods
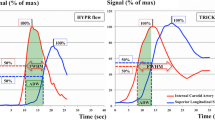
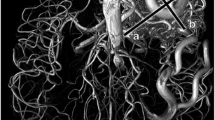
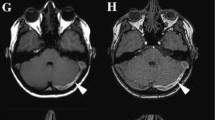
Time-resolved MRA with interleaved stochastic trajectories (TWIST) at 3.0 Tesla was studied in 83 consecutive patients with venous malformations (VM) and arteriovenous malformations (AVM). Enhancement characteristics were calculated as percentage increase of signal intensity above baseline over time. Maximum percentage signal intensity increase (signalmax), time intervals between onset of arterial enhancement and lesion enhancement (tonset), and time intervals between beginning of lesion enhancement and maximum percentage of lesion enhancement (tmax) were analyzed.
Results
All AVMs showed a high-flow hemodynamic pattern. Two significantly different (p < 0.001) types of venous malformations emerged: VMs with arteriovenous fistulas (AVF) (median signalmax 737 %, IQR [interquartile range] = 511 – 1182 %; median tonset 5 s, IQR = 5 – 10 s; median tmax 35 s, IQR = 26 – 40 s) and without AVFs (median signalmax 284 %, IQR = 177–432 %; median tonset 23 s, IQR = 15 – 30 s; median tmax 60 s, IQR = 55 – 75 s).
Conclusions
Quantitative evaluation of time-resolved MRA at 3.0 Tesla provides hemodynamic characterization of vascular malformations. VMs can be subclassified into two hemodynamic subgroups due to presence or absence of AVFs.
Key points
• Time-resolved MRA at 3.0 Tesla provides quantitative hemodynamic characterization of vascular malformations.
• Malformations significantly differ in time courses of enhancement and signal intensity increase.
• AVMs show a distinctive high-flow hemodynamic pattern.
• Two significantly different types of VMs emerged: VMs with and without AVFs.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- AVF:
-
Arteriovenous fistula
- AVM:
-
Arteriovenous malformation
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- MRA:
-
Magnetic resonance angiography
- ROC:
-
Receiver operating curve
- ROI:
-
Region of interest
- signal% :
-
Percentage increase of signal intensity above baseline
- signalmax :
-
Maximum percentage signal intensity increase
- tmax :
-
Time interval between beginning of enhancement and maximum percentage of enhancement
- tonset :
-
Time interval between onset of enhancement in an adjacent artery and within the lesion
- TWIST:
-
Time-resolved MRA with interleaved stochastic trajectories
- VIBE:
-
Volumetric interpolated breath-hold examination
- VM:
-
Venous malformation
References
Mulliken JB, Glowacki J (1982) Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 69(3):412–422
Behr GG, Johnson C (2013) Vascular anomalies: hemangiomas and beyond-part 1, fast-flow lesions. Am J Roentgenol 200(2):414–422
Donnelly LF, Adams DM, Bisset GS (2000) Vascular malformations and hemangiomas: a practical approach in a multidisciplinary clinic. AJR Am J Roentgenol 174(3):597–608
Lee BB, Kim DI, Huh S, Kim HH, Choo IW, Byun HS et al (2001) New experiences with absolute ethanol sclerotherapy in the management of a complex form of congenital venous malformation. J Vasc Surg 33(4):764–772
Park HS, Do YS, Park KB, Kim K, Woo SY, Jung S et al (2015) Clinical outcome and predictors of treatment response in foam sodium tetradecyl sulfate sclerotherapy of venous malformations. Eur Radiol. doi:10.1007/s00330-015-3931-9
Flors L, Leiva-Salinas C, Maged IM, Norton PT, Matsumoto AH, Angle JF et al (2011) MR imaging of soft-tissue vascular malformations: diagnosis, classification, and therapy follow-up. Radiographics 31(5):1321–1340
Behr GG, Johnson CM (2013) Vascular anomalies: hemangiomas and beyond - part 2, slow-flow lesions. Am J Roentgenol 200(2):423–436
Ohgiya Y, Hashimoto T, Gokan T, Watanabe S, Kuroda M, Hirose M et al (2005) Dynamic MRI for distinguishing high-flow from low-flow peripheral vascular malformations. AJR Am J Roentgenol 185(5):1131–1137
Herborn CU, Goyen M, Lauenstein TC, Debatin JF, Ruehm SG, Kröger K (2003) Comprehensive time-resolved MRI of peripheral vascular malformations. AJR Am J Roentgenol 181(3):729–735
Lim R, Shapiro M, Wang E, Law M, Babb J, Rueff L et al (2008) 3D time-resolved MR angiography (MRA) of the carotid arteries with time-resolved imaging with stochastic trajectories: comparison with 3D contrast-enhanced bolus-chase MRA and 3D time-of-flight MRA. Am J Neuroradiol 29(10):1847–1854
Rak KM, Yakes WF, Ray RL, Dreisbach JN, Parker SH, Luethke JM et al (1992) MR imaging of symptomatic peripheral vascular malformations. AJR Am J Roentgenol 159(1):107–112
Meyer JS, Hoffer FA, Barnes PD, Mulliken JB (1991) Biological classification of soft-tissue vascular anomalies: MR correlation. AJR Am J Roentgenol 157(3):559–564
van Rijswijk CSP, van der Linden E, van der Woude H, van Baalen JM, Bloem JL (2002) Value of dynamic contrast-enhanced MR imaging in diagnosing and classifying peripheral vascular malformations. AJR Am J Roentgenol 178(5):1181–1187
Kim JS, Chandler A, Borzykowski R, Thornhill B, Taragin BH (2012) Maximizing time-resolved MRA for differentiation of hemangiomas, vascular malformations and vascularized tumors. Pediatr Radiol 42(7):775–784
Kramer U, Ernemann U, Fenchel M, Seeger A, Laub G, Claussen CD et al (2011) Pretreatment evaluation of peripheral vascular malformations using low-dose contrast-enhanced time-resolved 3D MR angiography: initial results in 22 patients. AJR Am J Roentgenol 196(3):702–711
Anzidei M, Cavallo Marincola B, Napoli A, Saba L, Zaccagna F, Lucatelli P et al (2011) Low-dose contrast-enhanced time-resolved MR angiography at 3T: diagnostic accuracy for treatment planning and follow-up of vascular malformations. Clin Radiol 66(12):1181–1192
Mostardi PM, Young PM, McKusick MA, Riederer SJ (2012) High temporal and spatial resolution imaging of peripheral vascular malformations. J Magn Reson Imaging 36(4):933–942
Burrows PE, Paltiel HJ (2013) Radiological Imaging of Vascular Malformations. In: Mulliken JB, Burrows PE, Fishman SJ (eds) Mulliken & Young’s vascular anomalies: Hemangiomas and malformations, 2nd edn. Oxford University Press, Oxford, p 410
Dasgupta R, Fishman SJ (2014) ISSVA classification. Semin Pediatr Surg 23(4):158–161
Varnagy D, Labropoulos N (2006) The issue of spontaneous arteriovenous fistulae after superficial thrombophlebitis, endovenous ablations, and deep vein thrombosis: an unusual but predictable finding. Perspect Vasc Surg Endovasc Ther 18(3):247–250
Garzon MC, Huang JT, Enjolras O, Frieden IJ (2007) Vascular malformations: Part I. J Am Acad Dermatol 56(3):353–370, quiz 371–4
Acknowledgments
The scientific guarantor of this publication is Prof. Walter A. Wohlgemuth. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. Mr. Florian Zeman kindly provided statistical advice for this manuscript. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board.
Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hammer, S., Uller, W., Manger, F. et al. Time-resolved magnetic resonance angiography (MRA) at 3.0 Tesla for evaluation of hemodynamic characteristics of vascular malformations: description of distinct subgroups. Eur Radiol 27, 296–305 (2017). https://doi.org/10.1007/s00330-016-4270-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4270-1