Abstract
Objectives
To assess dose area products (DAP) and effective doses (ED) of voiding cystourethrography (VCUG) in children using optimized protocols on a modern flat detector unit.
Methods
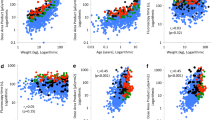
DAP and ED were evaluated in 651 VCUG (316 girls, median age: 2.25 years) between 2009 and 2012. DAP was analyzed in relation to patient characteristics (gender, age, presence of pathological findings) and experience of performing physician using analysis of variance. ED values were estimated using adapted conversion factors from the literature. Diagnostic image quality was validated by two experienced physicians using a 3-point scale.
Results
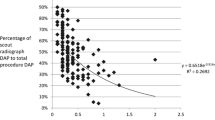
Median DAP/ED was 0.5 cGycm2/4.56 μSv (boys: 0.6 cGycm2/6.16 μSv; girls: 0.4 cGycm2/3.54 μSv). In 300 studies without pathologic findings DAP was 0.35 cGycm2, whereas 351 studies with pathologic findings had a median DAP of 0.7 cGycm2. No significant relationship between DAP and experience of radiologist was observed. Image validation resulted in an overall good to excellent rating.
Conclusions
DAP and ED can be markedly reduced in paediatric VCUG performed with optimized protocols on modern equipment without a noticeable decrease in diagnostic image quality.
Key points
• Voiding cystourethrography is a comprehensive examination in diagnosing vesicoureteral reflux (VUR).
• Radiation reduction is achieved in VCUG through modern equipment and optimized protocols.
• Low-dose VCUG is possible without noticeable decrease in diagnostic image quality.


Similar content being viewed by others
Abbreviations
- VCUG:
-
Voiding cystourethrography
- VUR:
-
Vesicoureteral reflux
- VUS:
-
Voiding urosonography
- RNC:
-
Radionuclide cystography
- MR-VCUG:
-
Magnetic resonance voiding cystourethrography
- DAP:
-
Dose area product
- ED:
-
Effective dose
- IRB:
-
Institutional review board
- FD:
-
Flat panel detector
- RIS:
-
Radiology information system
- PACS:
-
Picture Archiving and Communication System
References
Ammenti A, Cataldi L, Chimenz R et al (2012) Febrile urinary tract infections in young children: recommendations for the diagnosis, treatment and follow‐up. Acta Paediatr 101:451–457
Ward VL, Strauss KJ, Barnewolt CE et al (2008) Pediatric radiation exposure and effective dose reduction during voiding cystourethrography1. Radiology 249:1002–1009
Ward VL, Barnewolt CE, Strauss KJ et al (2006) Radiation exposure reduction during voiding cystourethrography in a pediatric porcine model of vesicoureteral reflux. Radiol Radiol Soc N Am 238:96–106
Hernanz-Schulman C, Coley - American College of Radiology. ACR–SPR Practice Guideline for the Performance of Voiding Cystourethrography in Children Res. 33 – 2009. American College of Radiology Web site2009 [February 3, 2015]; Available from: http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/Voiding_Cystourethrography.pdf
Roberts KB, Revised AAP (2012) Guideline on UTI in febrile infants and young children. Am Fam Physician 86:940–946
Riccabona M, Avni FE, Blickman JG et al (2008) Imaging recommendations in paediatric uroradiology: minutes of the ESPR workgroup session on urinary tract infection, fetal hydronephrosis, urinary tract ultrasonography and voiding cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol 38:138–145
Schultz F, Geleijns J, Holscher H, Weststrate J, Zonderland H, Zoetelief J (1999) Radiation burden to paediatric patients due to micturating cystourethrography examinations in a Dutch children’s hospital. Br J Radiol 72:763–772
Stueve D (2006) Management of pediatric radiation dose using Philips fluoroscopy systems DoseWise: perfect image, perfect sense. Pediatr Radiol 36:216–220
Ogden CL, Kuczmarski RJ, Flegal KM et al (2002) Centers for Disease Control and Prevention 2000 growth charts for the United States: improvements to the 1977 National Center for Health Statistics version. Pediatrics 109:45–60
Gosch D, Gosch K, Kahn T (2007) Conversion coefficients for estimation of effective dose to patients from dose area product during fluoroscopy x-ray examinations. Röfo 179:1035–1042
Le Heron J (1992) Estimation of effective dose to the patient during medical x-ray examinations from measurements of the dose-area product. Phys Med Biol 37:2117
Fefferman NR, Sabach AS, Rivera R et al (2009) The efficacy of digital fluoroscopic image capture in the evaluation of vesicoureteral reflux in children. Pediatr Radiol 39:1179–1187
Fotakis M, Athanasopoulou EM, Psarrakos K, Economou I (2003) Radiation doses to paediatric patients up to 5 years of age undergoing micturating cystourethrography examinations and its dependence on patient age: a Monte Carlo study. Br J Radiol 76:812–817
Papadopoulou F, Efremidis SC, Oiconomou A et al (2002) Cyclic voiding cystourethrography: is vesicoureteral reflux missed with standard voiding cystourethrography? Eur Radiol 12:666–670
Paltiel HJ, Rupich RC, Kiruluta HG (1992) Enhanced detection of vesicoureteral reflux in infants and children with use of cyclic voiding cystourethrography. Radiology 184:753–755
Born M, Spiller L, Bachour H, Heydweiller A, Franke I (2013) Dose area product of pediatric VCUG with regard to the strongly lowered German diagnostic reference levels. Röfo 185:262–267
González L, Vañó E, Ruiz M (1995) Radiation doses to paediatric patients undergoing micturating cystourethrography examinations and potential reduction by radiation protection optimization. Br J Radiol 68:291–295
Merkle EM, Aschoff AJ, Vogel J, Merk J, Bachor R, Brambs HJ (1997) Radiation exposure in digital micturition cystourethrography in children. How much exposure by fluoroscopy? Der Urologe Ausg A 36:181–185
Perisinakis K, Raissaki M, Damilakis J, Stratakis J, Neratzoulakis J, Gourtsoyiannis N (2006) Fluoroscopy-controlled voiding cystourethrography in infants and children: are the radiation risks trivial? Eur Radiol 16:846–851
Pazik FD, Staton RJ, Williams JL, Arreola MM, Hintenlang DE, Bolch WE (2007) Organ and effective doses in newborns and infants undergoing voiding cystourethrograms (VCUG): a comparison of stylized and tomographic phantoms. Med Phys 34:294–306
Publication of updated diagnostic reference levels for diagnostic and interventional X-ray examinations. German Federal Office for Radiation Protection Web site2010 [February 3, 2015]; Available from: http://www.bfs.de/de/ion/medizin/diagnostik/drw_roentgen.pdf
Kliegman R (2011) Nelson textbook of pediatrics. Elsevier/Saunders
Lassmann M, Treves ST (2014) Paediatric radiopharmaceutical administration: harmonization of the 2007 EANM paediatric dosage card (version 1.5.2008) and the 2010 North American consensus guidelines. Eur J Nucl Med Mol Imaging 41:1036–1041
Kim SW, Im YJ, Hong CH, Han SW (2010) The clinical significance of intrarenal reflux in voiding cystourethrography (VCUG). Korean J Urol 51:60–63
Boubnova J, Sergent-Alaoui A, Deschenes G, Audry G (2011) Evolution and prognosis value of intrarenal reflux. J Pediatr Urol 7:638–643
Fukui S, Watanabe M, Yoshino K (2013) Intrarenal reflux in primary vesicoureteral reflux. Int J Urol Off J Jpn Urol Assoc 20:631–636
Acknowledgments
The scientific guarantor of this publication is Jürgen F Schäfer. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sara Y. S. Linke and Ilias Tsiflikas contributed equally to this work.
Rights and permissions
About this article
Cite this article
Linke, S.Y.S., Tsiflikas, I., Herz, K. et al. Ultra low-dose VCUG in children using a modern flat detectorunit. Eur Radiol 26, 1678–1685 (2016). https://doi.org/10.1007/s00330-015-3996-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3996-5