Abstract
Objectives
The aim of this study was to investigate B-mode and elastographical ultrasound criteria capable of differentiating between benign and malignant parotid tumours and to define characteristic elastographical patterns for pleomorphic adenomas and Warthin’s tumours.
Methods
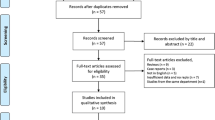
Fifty-seven patients with parotid gland tumours were examined using a combination of B-mode and elastographic ultrasounds. The data acquired were analysed retrospectively by two experienced ultrasound operators to identify specific sonographical features of benign and malignant lesions. Additionally, elastographical patterns were defined and analysed for their specificity.
Results
A blurred margin proved to be the only significant criterion in B-mode ultrasound capable of differentiating between malignant and benign tumours. The garland sign was defined as an elastographical pattern found significantly more frequently in malignant tumours, improving sonographical prediction of the benign or malignant nature of a parotid lesion. A logistic regression model was developed that achieved a correct prediction in 87.7% of cases. A “dense core” sign was also specifically defined for pleomorphic adenomas and a “half-half” sign for Warthin’s tumours.
Conclusions
Elastography is an innovative and powerful diagnostic tool that can improve the sonographical examination of parotid gland tumours by revealing easily recognised and characteristic patterns of tissue distribution.
Key Points
• Elastography can help differentiate benign from malignant parotid tumours during parotid ultrasound.
• The elastographical “garland sign” is more frequent in malignant than benign parotid tumours.
• Pleomorphic adenomas show an elastographical “dense core sign”.
• Warthin’s tumours show an elastographical “half-half sign”.
• Parotid cysts show an elastographical “bull’s-eye sign”.







Similar content being viewed by others
References
Stennert E, Wittekindt C, Klussmann JP, Guntinas-Lichius O (2004) New aspects in parotid gland surgery. Otolaryngol Pol 58:109–114
Klintworth N, Zenk J, Koch M, Iro H (2010) Postoperative complications after extracapsular dissection of benign parotid lesions with particular reference to facial nerve function. Laryngoscope 120:484–490. doi:10.1002/lary.20801
Rehberg E, Schroeder HG, Kleinsasser O (1998) Surgery in benign parotid tumors: individually adapted or standardized radical interventions? Laryngorhinootologie 77:283–288. doi:10.1055/s-2007-996975
Zbaren P, Guelat D, Loosli H, Stauffer E (2008) Parotid tumors: fine-needle aspiration and/or frozen section. Otolaryngol Head Neck Surg 139:811–815. doi:10.1016/j.otohns.2008.09.013
Howlett DC, Mercer J, Williams MD (2008) Same day diagnosis of neck lumps using ultrasound-guided fine-needle core biopsy. Br J Oral Maxillofac Surg 46:64–65
Hausegger KW, Krasa H, Pelzmann W, Grasser RK, Frisch C, Simon H (1993) Sonography of the salivary glands. Ultraschall Med 14:68–74
Yasumoto M, Yoshimura R, Sunaba K, Shibuya H (2001) Sonographic appearances of malignant lymphoma of the salivary glands. J Clin Ultrasound 29:491–498
Zhang L, Zhang ZY (2010) Evaluation of the ultrasonographic features of salivary gland tumours. Chin J Dent Res 13:133–137
Burke CJ, Thomas RH, Howlett D (2010) Imaging the major salivary glands. Br J Oral Maxillofac Surg 49:261–269
Thoeny HC (2007) Imaging of salivary gland tumours. Cancer Imaging 7:52–62
Wojcinski S, Farrokh A, Weber S et al (2010) Multicenter study of ultrasound real-time tissue elastography in 779 cases for the assessment of breast lesions: improved diagnostic performance by combining the BI-RADS(R)-US classification system with sonoelastography. Ultraschall Med 31:484–491
Yonetsu K, Ohki M, Kumazawa S, Eida S, Sumi M, Nakamura T (2004) Parotid tumors: differentiation of benign and malignant tumors with quantitative sonographic analyses. Ultrasound Med Biol 30:567–574
Scheipers U, Siebers S, Gottwald F et al (2005) Sonohistology for the computerized differentiation of parotid gland tumors. Ultrasound Med Biol 31:1287–1296
Yabuuchi H, Matsuo Y, Kamitani T et al (2008) Parotid gland tumors: can addition of diffusion-weighted MR imaging to dynamic contrast-enhanced MR imaging improve diagnostic accuracy in characterization? Radiology 249:909–916
Habermann CR, Arndt C, Graessner J et al (2009) Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible? AJNR Am J Neuroradiol 30:591–596
Christe A, Waldherr C, Hallett R, Zbaeren P, Thoeny H (2011) MR imaging of parotid tumors: typical lesion characteristics in MR imaging improve discrimination between benign and malignant disease. AJNR Am J Neuroradiol 32:1202–1207
Fodor D, Pop S, Maniu A, Cosgaria M (2010) Gray scale and Doppler ultrasonography of the benign tumors of parotid gland (pleomorphic adenoma and Warthin’s tumor). Pictorial essay. Med Ultrason 12:238–244
Ajayi BA, Pugh ND, Carolan G, Woodcock JP (1992) Salivary gland tumours: is colour Doppler imaging of added value in their preoperative assessment? Eur J Surg Oncol 18:463–468
Chikui T, Tokumori K, Yoshiura K, Oobu K, Nakamura S, Nakamura K (2005) Sonographic texture characterization of salivary gland tumors by fractal analyses. Ultrasound Med Biol 31:1297–1304
Steinhart H, Zenk J, Sprang K, Bozzato A, Iro H (2003) Contrast-enhanced color Doppler sonography of parotid gland tumors. Eur Arch Otorhinolaryngol 260:344–348
Siebers S, Zenk J, Bozzato A, Klintworth N, Iro H, Ermert H (2010) Computer aided diagnosis of parotid gland lesions using ultrasonic multi-feature tissue characterization. Ultrasound Med Biol 36:1525–1534
Dumitriu D, Dudea SM, Botar-Jid C, Baciut G (2010) Ultrasonographic and sonoelastographic features of pleomorphic adenomas of the salivary glands. Med Ultrason 12:175–183
Hall TJ (2003) AAPM/RSNA physics tutorial for residents: topics in US: beyond the basics: elasticity imaging with US. Radiographics 23:1657–1671
Leong LC, Sim LS, Lee YS et al (2010) A prospective study to compare the diagnostic performance of breast elastography versus conventional breast ultrasound. Clin Radiol 65:887–894
Schaefer FK, Heer I, Schaefer PJ et al (2011) Breast ultrasound elastography—results of 193 breast lesions in a prospective study with histopathologic correlation. Eur J Radiol 77:450–456
Adamietz BR, Meier-Meitinger M, Fasching P et al (2011) New diagnostic criteria in real-time elastography for the assessment of breast lesions. Ultraschall Med 32:67–73
Bojunga J, Herrmann E, Meyer G, Weber S, Zeuzem S, Friedrich-Rust M (2010) Real-time elastography for the differentiation of benign and malignant thyroid nodules: a meta-analysis. Thyroid 20:1145–1150
Holtel MR (2010) Emerging technology in head and neck ultrasonography. Otolaryngol Clin North Am 43:1267–1274, vii
Luo S, Kim EH, Dighe M, Kim Y (2011) Thyroid nodule classification using ultrasound elastography via linear discriminant analysis. Ultrasonics 51:425–431
Oliver C, Vaillant-Lombard J, Albarel F et al (2011) What is the contribution of elastography to thyroid nodules evaluation? Ann Endocrinol (Paris) 72:120–124
Sporea I, Vlad M, Bota S et al (2011) Thyroid stiffness assessment by acoustic radiation force impulse elastography (ARFI). Ultraschall Med 32:281–285
Pinto F, Totaro A, Calarco A et al (2011) Imaging in prostate cancer diagnosis: present role and future perspectives. Urol Int 86:373–382
Seitz M, Strittmatter F, Roosen A, Tilki D, Gratzke C (2010) Current status of ultrasound imaging in prostate cancer. Panminerva Med 52:189–194
Mahdavi SS, Moradi M, Wen X, Morris WJ, Salcudean SE (2011) Evaluation of visualization of the prostate gland in vibro-elastography images. Med Image Anal 15:589–600
Andersen ES, Christensen PB, Weis N (2009) Transient elastography for liver fibrosis diagnosis. Eur J Intern Med 20:339–342
Goertz RS, Amann K, Heide R, Bernatik T, Neurath MF, Strobel D (2011) An abdominal and thyroid status with Acoustic Radiation Force Impulse Elastometry - a feasibility srudy: Acoustic Radiation Force Impulse Elastometry of human organs. Eur J Radiol 80(3):e226–e230. doi:10.1016/j.ejrad.2010.09.025
Heide R, Strobel D, Bernatik T, Goertz RS (2010) Characterization of focal liver lesions (FLL) with acoustic radiation force impulse (ARFI) elastometry. Ultraschall Med 31:405–409
Bhatia KS, Rasalkar DD, Lee YP et al (2010) Evaluation of real-time qualitative sonoelastography of focal lesions in the parotid and submandibular glands: applications and limitations. Eur Radiol 20:1958–1964
Lyshchik A, Higashi T, Asato R et al (2007) Cervical lymph node metastases: diagnosis at sonoelastography—initial experience. Radiology 243:258–267
Bozzato A, Zenk J, Greess H et al (2007) Potential of ultrasound diagnosis for parotid tumors: analysis of qualitative and quantitative parameters. Otolaryngol Head Neck Surg 137:642–646
Poorten VV, Hart A, Vauterin T et al (2009) Prognostic index for patients with parotid carcinoma: international external validation in a Belgian–German database. Cancer 115:540–550. doi:10.1002/cncr.24015
Acknowledgements
Nils Klintworth and Konstantinos Mantsopoulos contributed equally to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klintworth, N., Mantsopoulos, K., Zenk, J. et al. Sonoelastography of parotid gland tumours: initial experience and identification of characteristic patterns. Eur Radiol 22, 947–956 (2012). https://doi.org/10.1007/s00330-011-2344-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2344-7