Abstract
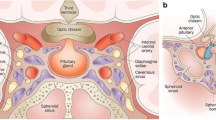
The sellar and parasellar region is an anatomically complex area that represents a crucial crossroad of important adjacent structures, e.g. orbits, cavernous sinus and its content, polygon of Willis, hypothalamus through the pituitary stalk and dural reflections forming the diaphragm sellae and the walls of the cavernous sinuses. Although the cavernous sinus represents the most relevant parasellar structure, from the practical and clinical point of view all the structures that surround the sella turcica can be included in the parasellar region. CT and, mainly, MRI are the imaging modalities to study and characterise the normal anatomy and the majority of processes in this region. We present a practical short review of the most relevant CT and MRI characteristics, such as location, nature of contrast enhancement and presence of cystic components, together with clinical findings, which permit differentiation of the most frequent and less common lesions found in the parasellar region.
Learning objectives:
-
A short review of the anatomy and clinical symptoms related to the parasellar region.
-
Radiological characterisation, mainly by MRI, of the many lesions that alter the structure and function of sellar and parasellar anatomy.
-
Description of the MRI features that permit differentiation among less common lesions









Similar content being viewed by others
References
Elster AD (1993) Modern imaging of the pituitary. Radiology 187:1–14
Gallioud P, Ruiz D, Muster M, et al (2000) Angiographic anatomy of laterocavernous sinus. Am J Neuroradiol 21:1923–1929
Keane JR (1996) Cavernous sinus syndrome. Analysis of 151 cases. Arch Neurol 53:967–971
Hudson J, Rufenacht DA, Ehman RL, Wiebers DO (1991) Intracranial aneurysms and vascular malformations: comparison of time-of-flight and phase-contrast MR angiography. Radiology 181:721–730
Niieo M, Shimozuru T, Nakamura K, et al (2000) Long-term follow-up study of patients with cavernous sinus aneurysm treated by proximal occlusion. Neurol Med Chir (Tokyo) 40:88–96
Hahn CD, Nicolle DA, Lownie SP, Drake CG (2000) Giant cavernous carotid aneurysms: clinical presentation in fifty-seven cases. J Neuroophthalmol 20:253–258
Debrun GM, Vinuela F, Fox AJ, et al (1988) Indications for treatment and classification of 132 carotid–cavernous fistulas. Neurosurgery 22:285–289
Ozwa T, Minakawa T, Saito A, et al (2001) MRA demonstration of ‘periarteritis’ in Tolosa–Hunt syndrome. Acta Neurochir 143:309–312
Cakirer S (2003) MRI findings in the patients with the presumptive clinical diagnosis of Tolosa–Hunt syndrome. Eur Radiol 13(1):17–28
Cottier J, Destrieux C, Brunereau J, et al (2000) Cavernous sinus invasion by pituitary adenoma: MR imaging. Radiology 215:463–469
Oot RF, Melville GE, New PFJ, et al (1988) The role of MR and CT in evaluating clival chordomas and chondrosarcomas. Am J Nueroradiol 9:715–723
Hayward R (1999) The present and future management of childhood craniopharyngiomas. Childs Nerv Syst 15:764–769
Sartorettt-Schefer S, et al (1997) MR differentiation of adamantinomatous and squamous-papillary craniopharyngiomas. Am J Neuroradiol 18:77–78
Boyko OB, Curnes JT, Oakes WJ, Burger PC (1991) Hamartomas of the tuber cinereum: CT, MR and pathological findings. Am J Neuroradiol 12:309–314
Iglesias A, Arias M, Brasa J, Paramo C, et al (2000) MR imaging findings in granular cell tumor of the neurohypophysis: a difficult preoperative diagnosis. Eur Radiol 10:1871–1873
Mamata H, Matsumae M, Yanagimachi N, Matsuyama S, et al (1998) Parasellar dermoid tumor with intra-tumoral hemorrhage. Eur Radiol 8:1594–1597
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruscalleda, J. Parasellar lesions. Eur Radiol 15, 549–559 (2005). https://doi.org/10.1007/s00330-004-2628-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2628-2