Abstract
Renal disease in primary Sjogren’s Syndrome(pSS) occurs as tubulointerstitial nephritis(TIN) or glomerulonephritis(GN). Data from India on pSS are sparse and even less on nephritis.
We studied the prevalence and impact of renal disease on patient outcomes. We reviewed 179 (F:M 12.7:1, age 41.7 ± 12.9 years) patients of pSS from records at a single centre from 2000 to 2020. Data on nephritis, clinical and laboratory variables were collected from baseline visit. Outcomes studied were chronic kidney disease(CKD) and death. We identified predictors of nephritis and rising creatinine on follow-up.
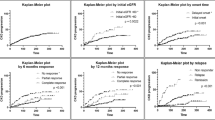
Fifty-four (30.17%) patients had nephritis. Their mean age was 40.19 ± 13.28 years with 157.3 person-years follow-up. Vasculitis (OR 2.33, 1.02–5.3), fatigue (OR 3.29, 1.63–6.65), ANA positivity (OR 7.79, 1–60.62), anti-Ro52 (OR 2.74, 1.18–6.39), anti-La (OR 2.13, 1.1–4.14), both Ro and La (OR 2.4, 1.23–4.69) and lymphopenia (OR 2.27, 1.16–4.41) predicted nephritis on univariate analysis. On multivariate analysis, only fatigue (OR 2.83, 1.22–6.57) and an interaction between polyarthritis and vasculitis (OR 9.17, 1.15–72.96) was associated with nephritis. Creatinine at one (1.6 ± 1.17 mg/dL vs. 0.8 ± 0.2 mg/dL) and 2 years (1.62 ± 1.19 mg/dL vs. 0.8 ± 0.2 mg/dL) follow-up was higher in the nephritis group. Baseline haematuria, leukocyturia, 24 h urinary protein and thrombocytopenia were independent predictors of rising creatinine. Six patients died and 10 developed CKD. Event-free (death or CKD) survival was 89.1% at 5 years. Patients with nephritis had worse event-free survival.
Our cohort had a younger age of onset of Sjogren’s syndrome and a higher prevalence of nephritis than previously reported. Fatigue, polyarthritis and vasculitis at baseline predicted the development of nephritis. Nephritis was associated with a higher probability of death or CKD.

Similar content being viewed by others
Data availability
Anonymised data and the R scripts will be available on request by email to the corresponding author.
References
Ramos-Casals M, Brito-Zerón P, Solans R, Camps M-T, Casanovas A, Sopeña B et al (2014) Systemic involvement in primary Sjogren’s syndrome evaluated by the EULAR-SS disease activity index: analysis of 921 Spanish patients (GEAS-SS registry). Rheumatol Oxf Engl 53(2):321–331
Sandhya P, Jeyaseelan L, Scofield RH, Danda D (2009) Clinical characteristics and outcome of primary Sjogren’s syndrome: a large asian indian cohort. Open Rheumatol J 9:36–45
Jain A, Srinivas BH, Emmanuel D, Jain VK, Parameshwaran S, Negi VS (2018) Renal involvement in primary Sjogren’s syndrome: a prospective cohort study. Rheumatol Int 38(12):2251–2262
Skopouli FN, Dafni U, Ioannidis JP, Moutsopoulos HM (2000) Clinical evolution, and morbidity and mortality of primary Sjögren’s syndrome. Semin Arthritis Rheum 29(5):296–304
Goules AV, Tatouli IP, Moutsopoulos HM, Tzioufas AG (2013) Clinically significant renal involvement in primary Sjögren’s syndrome: clinical presentation and outcome: clinical presentation and outcome of significant renal involvement in SS. Arthritis Rheum 65(11):2945–2953
Nocturne G, Mariette X (2013) Advances in understanding the pathogenesis of primary Sjögren’s syndrome. Nat Rev Rheumatol 9:544–556
Jasiek M, Karras A, Le Guern V, Krastinova E, Mesbah R, Faguer S et al (2017) A multicentre study of 95 biopsy-proven cases of renal disease in primary Sjögren’s syndrome. Rheumatology (Oxford) 56(3):362–370
Kim YK, Song HC, Kim WY, Yoon HE, Choi YJ, Ki CS et al (2008) Acquired Gitelman syndrome in a patient with primary Sjögren syndrome. Am J Kidney Dis 52(6):1163–1167
François H, Mariette X (2016) Renal involvement in primary Sjögren syndrome. Nat Rev Nephrol 12(2):82–93
Goules AV, Geetha D, Arend LJ, Baer AN (2019) Renal involvement in primary Sjögren’s syndrome: natural history and treatment outcome. Clin Exp Rheumatol 118(3):123–132
Yang HX, Wang J, Wen YB, Fei YY, Jiang MD, Zhou MY et al (2018) Renal involvement in primary Sjögren’s syndrome: a retrospective study of 103 biopsy-proven cases from a single center in China. Int J Rheum Dis 21(1):223–229
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 392(10159):1789–1858
Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM et al (2017) 2016 American college of rheumatology/european league against rheumatism classification criteria for primary Sjögren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol 69(1):35–45
Goules A, Masouridi S, Tzioufas AG, Ioannidis JP, Skopouli FN, Moutsopoulos HM (2000) Clinically significant and biopsy-documented renal involvement in primary Sjögren syndrome. Medicine 79(4):241–249
Bates D, Mächler M, Bolker B, Walker S (2015) Fitting linear mixed-effects models using lme4. J Stat Softw 67(1):1–48
Kuznetsova A, Brockhoff PB, Christensen RHB (2017) lmer test package: tests in linear mixed effects models. J Stat Softw 82(13):1–26
Ren H, Wang W-M, Chen X-N, Zhang W, Pan X-X, Wang X-L et al (2008) Renal involvement and followup of 130 patients with primary Sjögren’s syndrome. J Rheumatol 35(2):278–284
Luo J, Huo Y-W, Wang J-W, Guo H (2019) High-risk indicators of renal involvement in primary Sjogren’s syndrome: a clinical study of 1002 cases. J Immunol Res 2019:e3952392
Goules AV, Argyropoulou OD, Pezoulas VC, Chatzis L, Critselis E, Gandolfo S et al (2020) Primary Sjögren’s syndrome of early and late onset: distinct clinical phenotypes and lymphoma development. Front Immunol 11:594096
Ramos-Casals M, Cervera R, Font J, García-Carrasco M, Espinosa G, Reino S et al (1998) Young onset of primary Sjögren’s syndrome: clinical and immunological characteristics. Lupus 7(3):202–206
Anquetil C, Hachulla E, Machuron F, Mariette X, Le Guern V, Vittecoq O et al (2019) Is early-onset primary Sjögren’s syndrome a worse prognosis form of the disease? Rheumatology (Oxford) 58(7):1163–1167
Maripuri S, Grande JP, Osborn TG, Fervenza FC, Matteson EL, Donadio JV et al (2009) Renal involvement in primary Sjögren’s syndrome: a clinicopathologic study. Clin J Am Soc Nephrol CJASN 4(9):1423–1431
Gottenberg J-E, Seror R, Miceli-Richard C, Benessiano J, Devauchelle-Pensec V, Dieude P et al (2013) Serum levels of beta2-microglobulin and free light chains of immunoglobulins are associated with systemic disease activity in primary Sjögren’s syndrome data at enrollment in the prospective ASSESS cohort. PLoS ONE 8(5):e59868
Baldini C, Pepe P, Quartuccio L, Priori R, Bartoloni E, Alunno A et al (2014) Primary Sjogren’s syndrome as a multi-organ disease: impact of the serological profile on the clinical presentation of the disease in a large cohort of Italian patients. Rheumatol Oxf Engl 53(5):839–844
Ramos-Casals M, Solans R, Rosas J, Camps MT, Gil A, Del Pino-Montes J et al (2008) Primary Sjögren syndrome in Spain: clinical and immunologic expression in 1010 patients. Medicine (Baltimore) 87(4):210–219
Lin D-F, Yan S-M, Zhao Y, Zhang W, Li M-T, Zeng X-F et al (2010) Clinical and prognostic characteristics of 573 cases of primary Sjögren’s syndrome. Chin Med J (Engl) 123(22):3252–3257
Bodewes I, van der Spek PJ, Leon LG, Wijkhuijs A, van Helden-Meeuwsen CG, Tas L et al (2019) Fatigue in Sjögren’s syndrome: a search for biomarkers and treatment targets. Front Immunol 10:312
Majumder S, Singh P, Chatterjee R, Pattnaik SS, Aggarwal A (2021) Elevated urinary IL-36γ in patients with active lupus nephritis and response to treatment. Lupus 30(6):921–925
Norheim KB, Imgenberg-Kreuz J, Alexsson A, Johnsen SJA, Bårdsen K, Brun JG et al (2021) Genetic variants at the RTP4/MASP1 locus are associated with fatigue in scandinavian patients with primary Sjögren’s syndrome. RMD Open 7(3):e001832
Boys IN, Xu E, Mar KB, De La Cruz-Rivera PC, Eitson JL, Moon B, Schoggins JW (2020) RTP4 is a potent IFN-inducible anti-flavivirus effector engaged in a host-virus arms race in bats and other mammals. Cell Host Microbe 28(5):712-723.e9
Tarn JR, Howard-Tripp N, Lendrem DW, Mariette X, Saraux A, Devauchelle-Pensec V et al (2019) Symptom-based stratification of patients with primary Sjögren’s syndrome: multi-dimensional characterisation of international observational cohorts and reanalyses of randomised clinical trials. Lancet Rheumatol 1(2):e85-94
Argyropoulou OD, Pezoulas V, Chatzis L, Critselis E, Gandolfo S, Ferro F et al (2020) Cryoglobulinemic vasculitis in primary Sjögren’s syndrome: clinical presentation, association with lymphoma and comparison with hepatitis C-related disease. Semin Arthritis Rheum 50(5):846–853
Brito-Zerón P, Kostov B, Solans R, Fraile G, Suárez-Cuervo C, Casanovas A et al (2016) Systemic activity and mortality in primary Sjögren syndrome: predicting survival using the EULAR-SS disease activity index (ESSDAI) in 1045 patients. Ann Rheum Dis 75(2):348–355
Baimpa E, Dahabreh IJ, Voulgarelis M, Moutsopoulos HM (2009) Hematologic manifestations and predictors of lymphoma development in primary Sjögren syndrome: clinical and pathophysiologic aspects. Medicine (Baltimore) 88(5):284–293
Quartuccio L, Isola M, Baldini C, Priori R, Bartoloni Bocci E, Carubbi F et al (2014) Biomarkers of lymphoma in Sjögren’s syndrome and evaluation of the lymphoma risk in prelymphomatous conditions: results of a multicenter study. J Autoimmun 51:75–80
McEwan WA, Tam JCH, Watkinson RE, Bidgood SR, Mallery DL, James LC (2013) Intracellular antibody-bound pathogens stimulate immune signaling via the Fc receptor TRIM21. Nat Immunol 14(4):327–336
Higgs R, Gabhann JN, Larbi NB, Breen EP, Fitzgerald KA, Jefferies CA (2008) The E3 ubiquitin ligase Ro52 negatively regulates IFN-β production post-pathogen recognition by polyubiquitin-mediated degradation of IRF3. J Immunol Baltim Md 1950 181(3):1780–1786
Lazzari E, Korczeniewska J, Ní Gabhann J, Smith S, Barnes BJ, Jefferies CA (2014) TRIpartite motif 21 (TRIM21) differentially regulates the stability of interferon regulatory factor 5 (IRF5) isoforms. PLoS ONE 9(8):e103609
Higgs R, Lazzari E, Wynne C, Ní Gabhann J, Espinosa A, Wahren-Herlenius M et al (2010) Self protection from anti-viral responses–Ro52 promotes degradation of the transcription factor IRF7 downstream of the viral Toll-Like receptors. PLoS ONE 5(7):e11776
Evans R, Zdebik A, Ciurtin C, Walsh SB (2015) Renal involvement in primary Sjögren’s syndrome. Rheumatology 54(9):1541–1548
Pertovaara M, Korpela M, Pasternack A (2001) Factors predictive of renal involvement in patients with primary Sjögren’s syndrome. Clin Nephrol 56(1):10–18
Luo J, Xu S, Lv Y, Huang X, Zhang H, Zhu X et al (2019) Clinical features and potential relevant factors of renal involvement in primary Sjögren’s syndrome. Int J Rheum Dis 22(2):182–190
Gottenberg J-E, Cinquetti G, Larroche C, Combe B, Hachulla E, Meyer O et al (2013) Efficacy of rituximab in systemic manifestations of primary Sjogren’s syndrome: results in 78 patients of the autoimmune and rituximab registry. Ann Rheum Dis 72(6):1026–1031
Shen Y, Xie J, Lin L, Li X, Shen P, Pan X, Ren H, Chen N (2017) Combination cyclophosphamide/glucocorticoids provide better tolerability and outcomes versus glucocorticoids alone in patients with Sjogren’s associated chronic interstitial nephritis. Am J Nephrol 46(6):473–480
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Author information
Authors and Affiliations
Contributions
RC and AL were involved in conception and design of the study, acquisition and analysis of the data, drafting the manuscript and revising it critically for intellectual content. RK, UR, AB, LG, DPM, VA and AA were involved in acquisition and analysis of the data, revising and improving the manuscript with intellectual content.
Corresponding author
Ethics declarations
Conflicts of interest
Rudrarpan Chatterjee, Anu Balakrishnan, Rajat Kharbanda, Upendra Rathore, Latika Gupta, Durga P Misra, Vikas Agarwal, Amita Aggarwal and Able Lawrence declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chatterjee, R., Balakrishnan, A., Kharbanda, R. et al. Renal involvement in Sjőgren’s syndrome: predictors and impact on patient outcomes. Rheumatol Int 43, 1297–1306 (2023). https://doi.org/10.1007/s00296-022-05242-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05242-w