Abstract
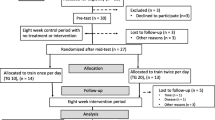
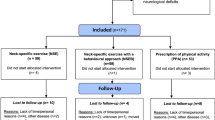
To investigate the effect of a structured exercise training program on pain, functional status, physical function and quality of life (QoL) in string and woodwind players with nonspecific cervical pain. This study had a prospective cohort design and conducted on 40 musicians (26 male, 14 female) aged between 18 and 65 years with persistent nonspecific neck pain in the previous 3 months. Forty musicians were assigned to either violin (n = 20, median age; 26.5 year, height; 1.67 m, body mass; 65 kg, BMI; 23.04 kg/m2) or ney group (n = 20, median age; 27.5 year, height; 1.81 m, body mass; 75 kg, BMI; 23.35 kg/m2) and followed the same structured exercise program (3 days/per week for 8 weeks). The primary outcome was neck pain intensity and assessed on a visual analog scale (VAS). Secondary outcomes; cervical range of motion (ROM) was measured using a goniometer, the jaw-to-sternum and jaw-to-wall distances were used for the assessment of cervical mobility, neck, shoulder and back muscles strength were assessed with a hand-held dynamometer, the Northwick Park Neck Pain and Short Form 36 (SF-36) questionnaires were also used. Normality of data distribution was checked using the Kolmogorov–Smirnov test. For evaluating the training effectiveness on outcome measures, Mann–Whitney U and Wilcoxon test were used compare pre-test and post-test values with/within groups, respectively. The primary outcome (pain intensity) was lowered %33 in both groups. However, the mean change was found similar (median mean changes; −2 for both groups) (p > 0.05). The secondary outcomes; cervical mobility, cervical flexion ROM, disability and muscle strength of the left middle trapezius, left hand grip, anterior and middle parts of the right deltoid, and cervical flexors also significantly improved in both groups (p < 0.05). Only the mean changes of right serratus anterior, middle trapezius and cervical flexor muscles were higher in violin group than ney group (p < 0.05). There was no significant difference in the cervical extension, right rotation, left rotation, right lateral flexion and left lateral flexion after the treatment in both groups (p > 0.05). There was no significant difference between the groups after the exercise program in terms of pain, mobility, range of motion and SF-36 subdomains (p > 0.05). Specific exercise program had similar positive effects on pain, cervical mobility, cervical fexion ROM and disability in string and woodwind players. Although several muscles showed similar improvements in strength, some muscle groups recovered differently. Physical needs specific to the instrument and performance should be taken into account when prescribing exercises to musicians having the same problem, but playing different instruments.


Similar content being viewed by others
References
Rotter G, Noeres K, Fernholz I, Willich SN, Schmidt A, Berghöfer A (2020) Musculoskeletal disorders and complaints in professional musicians: a systematic review of prevalence, risk factors, and clinical treatment effects. Int Arch Occup Environ Health 93:149–187. https://doi.org/10.1007/s00420-019-01467-8
Overton M, Du Plessis H, Sole G (2018) Electromyography of neck and shoulder muscles in instrumental musicians with musculoskeletal pain compared to asymptomatic controls: a systematic review and meta-analysis. Musculoskelet Sci 36:32–42. https://doi.org/10.1016/j.msksp.2018.04.001
Rensing N, Schemmann H, Zalpour C (2018) Musculoskeletal demands in violin and viola playing a literature review. Med Probl Perform Art 33:265–274. https://doi.org/10.21091/mppa.2018.4040
Steinmetz A, Seidel W, Muche B (2010) Impairment of postural stabilization systems in musicians with playing-related musculoskeletal disorders. J Manip Physiol Ther 33:603–611. https://doi.org/10.1016/j.jmpt.2010.08.006
Kok LM, Huisstede BM, Voorn VM, Schoones JW, Nelissen RG (2016) The occurrence of musculoskeletal complaints among professional musicians: a systematic review. Int Arch Occup Environ Health 89:373–396. https://doi.org/10.1007/s00420-015-1090-6
Ramella M, Fronte F, Converti R (2014) Postural disorders in conservatory students: the Diesis project. Med Probl Perform Art 29:19–22. https://doi.org/10.21091/mppa.2014.1005
Kaufman-Cohen Y, Ratzon N (2011) Correlation between risk factors and musculoskeletal disorders among classical musicians. Occup Med 61:90–95. https://doi.org/10.1093/occmed/kqq196
Sousa CM, Machado JP, Greten HJ, Coimbra D (2017) Playing-related musculoskeletal disorders of professional orchestra musicians from the North of Portugal: comparing string and wind musicians. Acta Med Port 30:302–306. https://doi.org/10.20344/amp.7568
Nyman T, Wiktorin C, Mulder M, Johansson YL (2007) Work postures and neck–shoulder pain among orchestra musicians. Am J Ind Med 50:370–376. https://doi.org/10.1002/ajim.20454
Kuo YL, Lee TH, Tsai YJ (2020) Evaluation of a cervical stabilization exercise program for pain, disability, and physical impairments in university violinists with nonspecific neck pain. Int J Environ Res 17:5430. https://doi.org/10.3390/ijerph17155430
Nezhad AB (2014) Iranian classical ney: pedagogy and performance. Malays J Music 3:48–66
Amanak K (2020) The effect of the sound of the ney (reed flute) on women in labour in Bursa, Turkey. J Pak Med Assoc 70:1934–1937. https://doi.org/10.47391/JPMA
Dawson WJ (2002) Upper-extremity problems caused by playing specific instruments. Med Probl Perform Art 17:135–140. https://doi.org/10.21091/mppa.2002.3022
Frank A, Mühlen CA (2007) Playing-related musculoskeletal complaints among musicians: prevalence and risk factors. Rev Bras Reumatol 47:188–196. https://doi.org/10.21091/mppa.2002.3022
Lederman RJ (2003) Neuromuscular and musculoskeletal problems in instrumental musicians. Muscle Nerve 27:549–561. https://doi.org/10.1002/mus.10380
Clemente MP, Mendes J, Vardasca R, Moreira A, Branco CA, Ferreira AP, Amarante JM (2020) Infrared thermography of the crânio-cervico-mandibular complex in wind and string instrumentalists. Int Arch Occup Environ Health 93:645–658. https://doi.org/10.1007/s00420-020-01517-6
Chan C, Driscoll T, Ackermann B (2013) Development of a specific exercise programme for professional orchestral musicians. Inj Prev 19:257–263. https://doi.org/10.1136/injuryprev-2012-040608
Ajidahun AT, Myezwa H, Mudzi W, Wood WA (2019) A scoping review of exercise intervention for playing-related musculoskeletal disorders (PRMDS) among musicians. Muziki 16:7–30. https://doi.org/10.1080/18125980.2019.1606675
Roos M, Roy JS (2018) Effect of a rehabilitation program on performance-related musculoskeletal disorders in student and professional orchestral musicians: a randomized controlled trial. Clin Rehabil 32:1656–1665. https://doi.org/10.1177/0269215518785000
Shafer-Crane GA (2006) Repetitive stress and strain injuries: preventive exercises for the musician. Phys Med Rehabil Clin 17(4):827–842. https://doi.org/10.1016/j.pmr.2006.07.005
Stanhope J, Pisaniello D, Weinstein P (2020) The effect of strategies to prevent and manage musicians’ musculoskeletal symptoms: a systematic review. Arch Environ Occup Health. https://doi.org/10.1080/19338244.2020.1860879
Alinia N, Norasteh AA, Majlan AS, Zarei H (2019) The Effect of Selected Exercise Program on Musculoskeletal Pain of Neck and Shoulder in Violinist. J Clin Physiother Res 4:20–25. https://doi.org/10.22037/jcpr.v4i1.24187
Tsai Y, Lee T, Kuo Y (2018) Effects of cervical stabilization/strengthening exercises in violinists with chronic nonspecific neck pain. Ann Phys Rehabil Med 61:e148. https://doi.org/10.1016/j.rehab.2018.05.331
Rotter G, Fernholz I, Binting S, Keller T, Roll S, Kass B, Reinhold T, Willich SN, Schmidt A, Brinkhaus B (2020) The effect of osteopathic medicine on pain in musicians with nonspecific chronic neck pain: a randomized controlled trial. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X20979853
Misailidou V, Malliou P, Beneka A, Karagiannidis A, Godolias G (2010) Assessment of patients with neck pain: a review of definitions, selection criteria, and measurement tools. J Chiropr Med 9:49–59. https://doi.org/10.1016/j.jcm.2010.03.002
Aslan Telci E, Karaduman A (2012) Effects of three different conservative treatments on pain, disability, quality of life, and mood in patients with cervical spondylosis. Rheumatol Int 32:1033–1040. https://doi.org/10.1007/s00296-010-1751-4
Akaltun MS, Kocyigit BF (2021) Assessment of the responsiveness of four scales in geriatric patients with chronic neck pain. Rheumatol Int 41:1825–1831. https://doi.org/10.1007/s00296-021-04957-6
Leak A, Cooper J, Dyer S, Williams K, Turner-Stokes L, Frank A (1994) The Northwick Park Neck Pain Questionnaire, devised to measure neck pain and disability. Rheumatology 33:469–474. https://doi.org/10.1093/rheumatology/33.5.469
Cools AM, De Wilde L, Van Tongel A, Ceyssens C, Ryckewaert R, Cambier DC (2014) Measuring shoulder external and internal rotation strength and range of motion: comprehensive intra-rater and inter-rater reliability study of several testing protocols. J Shoulder Elb Surg 23:1454–1461. https://doi.org/10.1016/j.jse.2014.01.006
Higgins SC, Adams J, Hughes R (2018) Measuring hand grip strength in rheumatoid arthritis. Rheumatol Int 38:707–714. https://doi.org/10.1007/s00296-018-4024-2
Ulutatar F, Unal-Ulutatar C, Duruoz MT (2019) Cervical proprioceptive impairment in patients with rheumatoid arthritis. Rheumatol Int 39:2043–2051. https://doi.org/10.1007/s00296-019-04419-0
Arranz L, Canela MA, Rafecas M (2012) Relationship between body mass index, fat mass and lean mass with SF-36 quality of life scores in a group of fibromyalgia patients. Rheumatol Int 32:3605–3611. https://doi.org/10.1007/s00296-011-2250-y
Falla D, Bilenkij G, Jull G (2004) Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine 29:1436–1440. https://doi.org/10.1097/01.brs.0000128759.02487.bf
Berque P, Gray H (2002) The influence of neck–shoulder pain on trapezius muscle activity among professional violin and viola players: an electromyographic study. Med Probl Perform Art 17(2):68–75. https://doi.org/10.21091/mppa.2002.2011
Lee H, Nicholson LL, Adams RD (2004) Cervical range of motion associations with subclinical neck pain. Spine 29:33–40. https://doi.org/10.1097/01.BRS.0000103944.10408.BA
Stenneberg MS, Rood M, de Bie R, Schmitt MA, Cattrysse E, Scholten-Peeters GG (2017) To what degree does active cervical range of motion differ between patients with neck pain, patients with whiplash, and those without neck pain? A systematic review and meta-analysis. Arch Phys Med Rehabil 98:1407–1434. https://doi.org/10.1016/j.apmr.2016.10.003
Holtermann A, Mork P, Andersen L, Olsen HB, Søgaard K (2010) The use of EMG biofeedback for learning of selective activation of intra-muscular parts within the serratus anterior muscle: a novel approach for rehabilitation of scapular muscle imbalance. J Electromyogr Kinesiol 20:359–365. https://doi.org/10.1016/j.jelekin.2009.02.009
Fayez ES (2014) The correlation between neck pain and hand grip strength of dentists. Occup Med Health Aff 2:5. https://doi.org/10.4172/2329-6879.1000185
Seo NJ, Sindhu BS, Shechtman O (2011) Influence of pain associated with musculoskeletal disorders on grip force timing. J Hand Ther 24:335–344. https://doi.org/10.1016/j.jht.2011.06.004
Van Wilgen C, Akkerman L, Wieringa J, Dijkstra P (2003) Muscle strength in patients with chronic pain. Clin Rehabil 17:885–889. https://doi.org/10.1191/0269215503cr693oa
Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ (2003) Impact of neck and arm pain on overall health status. Spine 28:2030–2035. https://doi.org/10.1097/01.BRS.0000083325.27357.39
Telci EA, Karaduman A (2012) Effects of three different conservative treatments on pain, disability, quality of life, and mood in patients with cervical spondylosis. Rheumatol Int 32:1033–1040. https://doi.org/10.1007/s00296-010-1751-4
Rezai M, Côté P, Cassidy JD, Carroll L (2009) The association between prevalent neck pain and health-related quality of life: a cross-sectional analysis. Eur Spine J 18:371–381. https://doi.org/10.1007/s00586-008-0823-6
Piątkowska K, Wnuk B, Blicharska I, Rychlik M, Durmała J (2016) Cervical pain in young professional musicians-quality of life. Ortop Traumatol Rehabil 18:21–29. https://doi.org/10.5604/15093492.1198832
Gross AR, Paquin JP, Dupont G, Blanchette S, Lalonde P, Cristie T, Graham N, Kay TM, Burnie SJ, Gelley G, Goldsmith CH, Forget M, Santaguida PL, Yee AJ, Radisic GG, Hoving JL, Bronfort G, Cervical Overview Group (2016) Exercises for mechanical neck disorders: a cochrane review update. Man Ther 24:25–45. https://doi.org/10.1016/j.math.2016.04.005
Funding
Not funded.
Author information
Authors and Affiliations
Contributions
SU and HA designed the study; SU, HA and AA provided the data; BFK and YY made the statistical analyses; SU and AA contributed the analysis tools; SU, HA, BFK, AA and YY authored and reviewed drafts of the paper; SU and HA prepared the tables and figures; SU, HA, BFK, AA and YY reviewed and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical statement
This study was approved by the Ethics Committee for Non-Invasive Research Trials of Hasan Kalyoncu University Faculty of Health Sciences (approval number 2017/14).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Usgu, S., Akbey, H., Kocyigit, B.F. et al. Comparison of the effectiveness of a structured exercise program on nonspecific neck pain in string and woodwind players. Rheumatol Int 42, 725–736 (2022). https://doi.org/10.1007/s00296-021-05085-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-05085-x