Abstract
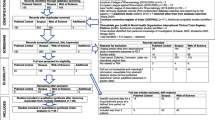
We evaluated clinical response, normalization of inflammatory markers, angiographic stabilization (primary outcomes), relapses and adverse events (secondary outcomes) in Takayasu arteritis (TAK) patients following corticosteroid monotherapy. MEDLINE, EMBASE, Web of Science, Scopus, Pubmed Central, Cochrane library, clinical trial databases and major international Rheumatology conferences were searched for studies reporting outcomes in TAK following corticosteroid monotherapy (without language/date restrictions). Risk ratios were calculated for controlled studies. Proportions were pooled for uncontrolled studies. Heterogeneity was assessed using I2 statistic. Quality assessment of individual studies utilized the Newcastle–Ottawa scale. GRADE methodology ascertained certainty of individual outcomes across studies. Twenty-eight observational studies (1098 TAK) were identified. Twenty-three uncontrolled studies (580 TAK) were synthesized in meta-analysis. Clinical response was observed in 60% (95% CI 45–74%, 19 studies), normalization of inflammatory markers in 84% (95% CI 54–100%, 4 studies) and angiographic stabilization in 28% (95% CI 6–57%, 4 studies). Relapses occurred in 66% (95% CI 18–99%, 4 studies). Adverse events were reported in 51% (95% CI 2–99%, 4 studies). All pooled estimates had considerable heterogeneity, unexplained by subgroup analyses (time period, geographic location or number of patients). Two studies reported lesser restenosis following vascular surgery and fewer relapses when corticosteroids were combined with immunosuppressants compared with corticosteroid monotherapy. All outcomes had very low certainty. While corticosteroid monotherapy induces clinical response in most TAK patients, angiographic stabilization is observed in fewer than one-third. Most patients relapse following corticosteroid withdrawal. Preliminary evidence supports up-front addition of immunosuppressants to retard angiographic progression and reduce relapses (PROSPERO identifier CRD42021242910).



Similar content being viewed by others
Data availability
All the analyses performed for this systematic review have been reported in the main text or in the supplementary files. Data pertaining to the systematic review shall be shared on reasonable request to the corresponding author (Durga Prasanna Misra, durgapmisra@gmail.com).
Abbreviations
- 95% CI:
-
95% Confidence intervals
- ACR:
-
American College of Rheumatology
- APLAR:
-
Asia–Pacific League of Associations for Rheumatology
- CENTRAL:
-
Cochrane Central Register of Clinical Trials
- CRP:
-
C-reactive protein
- DMARD:
-
Disease-modifying anti-rheumatic drug
- ESR:
-
Erythrocyte sedimentation rate
- EULAR:
-
European Alliance of Associations for Rheumatology
- GRADE:
-
Grading of recommendations, assessment, development and evaluation
- ICTRP:
-
International Clinical Trials Registry Platform
- ITAS2010:
-
Indian Takayasu Clinical Activity Score
- MOOSE:
-
Meta-analysis of observational studies in epidemiology
- NIH:
-
National Institutes of Health
- PET-CT:
-
Positron emission tomography computerized tomography
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PRISMA-S:
-
PRISMA statement modified to include systematic searches across databases
- PROSPERO:
-
International prospective register of systematic reviews
- TAK:
-
Takayasu arteritis
- Th1:
-
T helper 1
- Th17:
-
T helper 17
- Th17.1:
-
T helper 17.1
References
Jennette JC, Falk RJ, Bacon PA et al (2013) 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65:1–11. https://doi.org/10.1002/art.37715
Keser G, Direskeneli H, Aksu K (2014) Management of Takayasu arteritis: a systematic review. Rheumatology (Oxford) 53:793–801. https://doi.org/10.1093/rheumatology/ket320
Misra DP, Wakhlu A, Agarwal V, Danda D (2019) Recent advances in the management of Takayasu arteritis. Int J Rheum Dis 22(Suppl 1):60–68. https://doi.org/10.1111/1756-185x.13285
Arnaud L, Haroche J, Mathian A, Gorochov G, Amoura Z (2011) Pathogenesis of Takayasu’s arteritis: a 2011 update. Autoimmun Rev 11:61–67. https://doi.org/10.1016/j.autrev.2011.08.001
Misra DP, Chaurasia S, Misra R (2016) Increased circulating Th17 cells, serum IL-17A, and IL-23 in Takayasu arteritis. Autoimmun Dis. https://doi.org/10.1155/2016/7841718
Castillo-Martínez D, Amezcua-Castillo LM, Granados J, Pineda C, Amezcua-Guerra LM (2020) Is Takayasu arteritis the result of a Mycobacterium tuberculosis infection? The use of TNF inhibitors may be the proof-of-concept to demonstrate that this association is epiphenomenal. Clin Rheumatol 39:2003–2009. https://doi.org/10.1007/s10067-020-05045-z
Misra DP, Misra R (2015) Assessment of disease activity in Takayasu’s arteritis. Indian J Rheumatol 10:S43–S47. https://doi.org/10.1016/j.injr.2015.08.006
Misra DP, Sharma A, Kadhiravan T, Negi VS (2017) A scoping review of the use of non-biologic disease modifying anti-rheumatic drugs in the management of large vessel vasculitis. Autoimmun Rev 16:179–191. https://doi.org/10.1016/j.autrev.2016.12.009
Misra DP, Agarwal V (2020) The perennial search for alternatives to corticosteroids in rheumatology: is there light at the end of the tunnel? Clin Rheumatol 39:2845–2848. https://doi.org/10.1007/s10067-020-05357-0
Dua A, Das P, Ravindran V (2019) Glucocorticoids: a review of its adverse effects including bone loss. Indian J Rheumatol 14:90–98. https://doi.org/10.4103/0973-3698.272158
Misra DP, Rathore U, Patro P, Agarwal V, Sharma A (2021) Disease-modifying anti-rheumatic drugs for the management of Takayasu arteritis—a systematic review and meta-analysis. Clin Rheumatol. https://doi.org/10.1007/s10067-021-05743-2
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) (2019) Cochrane handbook for systematic reviews of interventions, 2nd edn. John Wiley & Sons, Chichester
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:1000097–1000097. https://doi.org/10.1371/journal.pmed.1000097
Rethlefsen ML, Kirtley S, Waffenschmidt S et al (2021) PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev 10:39. https://doi.org/10.1186/s13643-020-01542-z
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD (2011) Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 31:1409–1417. https://doi.org/10.1007/s00296-011-1999-3
Arend WP, Michel BA, Bloch DA et al (1990) The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 33:1129–1134. https://doi.org/10.1002/art.1780330811
Ishikawa K (1988) Diagnostic approach and proposed criteria for the clinical diagnosis of Takayasu’s arteriopathy. J Am Coll Cardiol 12:964–972. https://doi.org/10.1016/0735-1097(88)90462-7
Sharma BK, Jain S, Suri S, Numano F (1996) Diagnostic criteria for Takayasu arteritis. Int J Cardiol 54(Suppl):S141-147
Ozen S, Pistorio A, Iusan SM et al (2010) EULAR/PRINTO/PRES criteria for Henoch-Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: final classification criteria. Ann Rheum Dis 69:798–806. https://doi.org/10.1136/ard.2009.116657
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Newcastle-Ottawa scale. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed on 16 Apr 2021
Li L, Liu C, Cheng L, Yan S, Chen H, Li Y (2021) Assessment of diagnostic utility, clinical phenotypic associations, and prognostic significance of anti-NXP2 autoantibody in patients with idiopathic inflammatory myopathies: a systematic review and meta-analysis. Clin Rheumatol 40:819–832. https://doi.org/10.1007/s10067-020-05291-1
Lin L, Chu H (2018) Quantifying publication bias in meta-analysis. Biometrics 74:785–794. https://doi.org/10.1111/biom.12817
Misra DP, Agarwal V (2018) Systematic reviews: challenges for their justification, related comprehensive searches, and implications. J Korean Med Sci 33:9. https://doi.org/10.3346/jkms.2018.33.e92
Online calculator for pooling variances. https://home.ubalt.edu/ntsbarsh/business-stat/otherapplets/Pooled.htm. Accessed 20 Apr 2021
Practical meta-analysis effect size calculator. Available at https://campbellcollaboration.org/escalc/html/EffectSizeCalculator-SMD1.php. Accessed 23 Jul 2021
Nyaga VN, Arbyn M, Aerts M (2014) Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72:39. https://doi.org/10.1186/2049-3258-72-39
Brunner J, Feldman BM, Tyrrell PN et al (2010) Takayasu arteritis in children and adolescents. Rheumatology (Oxford) 49:1806–1814. https://doi.org/10.1093/rheumatology/keq167
Misra DP, Aggarwal A, Lawrence A, Agarwal V, Misra R (2015) Pediatric-onset Takayasu’s arteritis: clinical features and short-term outcome. Rheumatol Int 35:1701–1706. https://doi.org/10.1007/s00296-015-3272-7
GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2020 (developed by Evidence Prime, Inc.). Available from gradepro.org.
Nakao K, Ikeda M, Kimata S, Niitani H, Niyahara M (1967) Takayasu’s arteritis. Clinical report of eighty-four cases and immunological studies of seven cases. Circulation 35:1141–1155. https://doi.org/10.1161/01.cir.35.6.1141
Fraga A, Mintz G, Valle L, Flores-Izquierdo G (1972) Takayasu’s arteritis: frequency of systemic manifestations (study of 22 patients) and favorable response to maintenance steroid therapy with adrenocorticosteroids (12 patients). Arthritis Rheum 15:617–624. https://doi.org/10.1002/art.1780150608
Morooka S, Ito I, Yamaguchi H, Takeda T, Saito Y (1972) Follow-up observation of aortitis syndrome. Jpn Heart J 13:201–213. https://doi.org/10.1536/ihj.13.201
Lupi-Herrera E, Sánchez-Torres G, Marcushamer J, Mispireta J, Horwitz S, Vela JE (1977) Takayasu’s arteritis. Clinical study of 107 cases. Am Heart J 93:94–103. https://doi.org/10.1016/s0002-8703(77)80178-6
Hall S, Barr W, Lie JT, Stanson AW, Kazmier FJ, Hunder GG (1985) Takayasu arteritis: a study of 32 north American patients. Medicine (Baltimore) 64:89–99. https://doi.org/10.1097/00005792-198503000-00002
Shelhamer JH, Volkman DJ, Parrillo JE, Lawley TJ, Johnston MR, Fauci AS (1985) Takayasu’s arteritis and its therapy. Ann Intern Med 103:121–126. https://doi.org/10.7326/0003-4819-103-1-121
Weaver FA, Yellin AE, Campen DH et al (1990) Surgical procedures in the management of Takayasu’s arteritis. J Vasc Surg 12:429–439. https://doi.org/10.1016/0741-5214(90)90045-C
Ishikawa K (1991) Effects of prednisolone therapy on arterial angiographic features in Takayasu’s disease. Am J Cardiol 68:410–413. https://doi.org/10.1016/0002-9149(91)90845-C
Zheng D, Fan D, Liu L (1992) Takayasu arteritis in China: a report of 530 cases. Heart Vessels Suppl 7:32–36
Kerr GS, Hallahan CW, Giordano J et al (1994) Takayasu arteritis. Ann Intern Med 120:919–929. https://doi.org/10.7326/0003-4819-120-11-199406010-00004
Jain S, Kumari S, Ganguly NK, Sharma BK (1996) Current status of Takayasu arteritis in India. Int J Cardiol 54:S111–S116. https://doi.org/10.1016/S0167-5273(96)88780-8
Lambert M, Hachulla E, Hatron PY et al (1998) Takayasu’s arteritis: vascular investigations and therapeutic management. Experience with 16 patients. Rev Med Interne 19:878–884
Sato EI, Lima DN, Santo BE, Hata F (2000) Takayasu arteritis. Treatment and prognosis in a university center in Brazil. Int J Cardiol 75(Suppl 1):163–166
Paul JF, Fiessinger JN, Sapoval M et al (2001) Follow-up electron beam CT for the management of early phase Takayasu arteritis. J Comput Assist Tomogr 25:924–931. https://doi.org/10.1097/00004728-200111000-00015
El Asri A, Tazi-Mezalek Z, Aouni M et al (2002) Takayasu’s arteritis in Morroco. A study of 47 cases. Rev Med Interne 23:9–20. https://doi.org/10.1016/s0248-8663(01)00510-0
Park MC, Lee SW, Park YB, Lee SK, Choi D, Shim WH (2006) Post-interventional immunosuppressive treatment and vascular restenosis in Takayasu’s arteritis. Rheumatology (Oxford) 45:600–605. https://doi.org/10.1093/rheumatology/kei245
Maksimowicz-McKinnon K, Clark TM, Hoffman GS (2007) Limitations of therapy and a guarded prognosis in an American cohort of Takayasu arteritis patients. Arthritis Rheum 56:1000–1009. https://doi.org/10.1002/art.22404
Petrovic-Rackov L, Pejnovic N, Jevtic M, Damjanov N (2009) Longitudinal study of 16 patients with Takayasu’s arteritis: clinical features and therapeutic management. Clin Rheumatol 28:179–185. https://doi.org/10.1007/s10067-008-1009-7
Arnaud L, Haroche J, Limal N et al (2010) Takayasu arteritis in France: a single-center retrospective study of 82 cases comparing white, North African, and black patients. Medicine 89:1–17. https://doi.org/10.1097/MD.0b013e3181cba0a3
Cong X-L, Dai S-M, Feng X et al (2010) Takayasu’s arteritis: clinical features and outcomes of 125 patients in China. Clin Rheumatol 29:973–981. https://doi.org/10.1007/s10067-010-1496-1
Jaafoura NG, Khalifa M, Rezgui A et al (2010) Takayasu’s disease in central Tunisia: 27 cases. J Mal Vasc 35:4–11. https://doi.org/10.1016/j.jmv.2009.09.002
Nunes G, Neves FS, Melo FM, de Castro GRW, Zimmermann AF, Pereira IA (2010) Takayasu arteritis: anti-TNF therapy in a Brazilian setting. Rev Bras Reumatol 50:295–298. https://doi.org/10.1590/s0482-50042010000300009
Ohigashi H, Haraguchi G, Konishi M et al (2012) Improved prognosis of Takayasu arteritis over the past decade—comprehensive analysis of 106 patients. Circ J 76:1004–1011. https://doi.org/10.1253/circj.CJ-11-1108
Yang L, Zhang H, Jiang X et al (2015) Clinical features and outcomes of Takayasu arteritis with neurological symptoms in China: a retrospective study. J Rheumatol 42:1846–1852. https://doi.org/10.3899/jrheum.150097
Gudbrandsson B, Molberg PO (2017) TNF inhibitors appear to inhibit disease progression and improve outcome in Takayasu arteritis; an observational, population-based time trend study. Arthritis Res Ther 19:99. https://doi.org/10.1186/s13075-017-1316-y
Ohigashi H, Tamura N, Ebana Y et al (2017) Effects of immunosuppressive and biological agents on refractory Takayasu arteritis patients unresponsive to glucocorticoid treatment. J Cardiol 69:774–778. https://doi.org/10.1016/j.jjcc.2016.07.009
Peng Y-F, Guo J, Deng Y-B (2017) The role of mean platelet volume in patients with Takayasu arteritis. Ann Clin Biochem 54:273–278. https://doi.org/10.1177/0004563216658312
Mutoh T, Shirai T, Fujii H, Ishii T, Harigae H (2020) Insufficient use of corticosteroids without immunosuppressants results in higher relapse rates in Takayasu arteritis. J Rheumatol 47:255–263. https://doi.org/10.3899/jrheum.181219
Hoffman GS (1996) Takayasu arteritis: lessons from the American National Institutes of Health Experience. Int J Cardiol 54:S99–S102. https://doi.org/10.1016/s0167-5273(96)88778-x
Maz M, Chung SA, Abril A et al (2021) 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of giant cell arteritis and Takayasu arteritis. Arthritis Rheumatol. https://doi.org/10.1002/art.41774
IntHout J, Ioannidis JPA, Borm GF, Goeman JJ (2015) Small studies are more heterogeneous than large ones: a meta-meta-analysis. J Clin Epidemiol 68:860–869. https://doi.org/10.1016/j.jclinepi.2015.03.017
Misra DP, Naidu G, Agarwal V, Sharma A (2019) Vasculitis research: current trends and future perspectives. Int J Rheum Dis 22(Suppl 1):10–20. https://doi.org/10.1111/1756-185x.13370
Barra L, Kanji T, Malette J, Pagnoux C (2018) Imaging modalities for the diagnosis and disease activity assessment of Takayasu’s arteritis: a systematic review and meta-analysis. Autoimmun Rev 17:175–187. https://doi.org/10.1016/j.autrev.2017.11.021
Incerti E, Tombetti E, Fallanca F et al (2017) (18)F-FDG PET reveals unique features of large vessel inflammation in patients with Takayasu’s arteritis. Eur J Nucl Med Mol Imaging 44:1109–1118. https://doi.org/10.1007/s00259-017-3639-y
Wen X, Hou R, Xu K et al (2021) Pentraxin 3 is more accurate than C-reactive protein for Takayasu arteritis activity assessment: a systematic review and meta-analysis. PLoS ONE 16:e0245612. https://doi.org/10.1371/journal.pone.0245612
Goel R, Nair A, Kabeerdoss J et al (2018) Study of serial serum myeloid-related protein 8/14 as a sensitive biomarker in Takayasu arteritis: a single centre study. Rheumatol Int 38:623–630. https://doi.org/10.1007/s00296-017-3881-4
Saadoun D, Garrido M, Comarmond C et al (2015) Th1 and Th17 cytokines drive inflammation in takayasu arteritis. Arthritis Rheumatol 67:1353–1360. https://doi.org/10.1002/art.39037
Deng J, Younge BR, Olshen RA, Goronzy JJ, Weyand CM (2010) Th17 and Th1 T-cell responses in giant cell arteritis. Circulation 121:906–915. https://doi.org/10.1161/circulationaha.109.872903
Ramesh R, Kozhaya L, McKevitt K et al (2014) Pro-inflammatory human Th17 cells selectively express P-glycoprotein and are refractory to glucocorticoids. J Exp Med 211:89–104. https://doi.org/10.1084/jem.20130301
Kansal A, Tripathi D, Rai MK, Agarwal V (2016) Persistent expression and function of P-glycoprotein on peripheral blood lymphocytes identifies corticosteroid resistance in patients with systemic lupus erythematosus. Clin Rheumatol 35:341–349. https://doi.org/10.1007/s10067-015-3079-7
Prasad S, Tripathi D, Rai MK, Aggarwal S, Mittal B, Agarwal V (2014) Multidrug resistance protein-1 expression, function and polymorphisms in patients with rheumatoid arthritis not responding to methotrexate. Int J Rheum Dis 17:878–886. https://doi.org/10.1111/1756-185x.12362
Osborne SF, Jordan K (2004) Spontaneous regression of optic disc neovascularization in Takayasu arteritis. Eye 18:86–88. https://doi.org/10.1038/sj.eye.6700508
Palmowski A, Buttgereit F (2020) Reducing the toxicity of long-term glucocorticoid treatment in large vessel vasculitis. Curr Rheumatol Rep 22:85. https://doi.org/10.1007/s11926-020-00961-0
Funding
Durga Prasanna Misra acknowledges support from Indian Council of Medical Research (Grant No 5/4/1-2/2019-NCD-II) for his research on Takayasu arteritis. The funding agency had no role in the actual conduct or reporting of this systematic review.
Author information
Authors and Affiliations
Contributions
The conception and design of the study: DPM, VA, AS; acquisition of data, analysis and interpretation of data: DPM, UR, PP; drafting the article: DPM, UR, PP; revising it critically for important intellectual content: VA, AS; final approval of the version to be submitted: DPM, UR, PP, VA, AS; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: DPM, UR, PP, VA, AS.
Corresponding author
Ethics declarations
Conflict of interest
Durga Prasanna Misra, Upendra Rathore, Pallavi Patro, Vikas Agarwal and Aman Sharma declares that they have no conflicts of interest, including no relationship with pharmaceutical companies.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Misra, D.P., Rathore, U., Patro, P. et al. Corticosteroid monotherapy for the management of Takayasu arteritis—a systematic review and meta-analysis. Rheumatol Int 41, 1729–1742 (2021). https://doi.org/10.1007/s00296-021-04958-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-04958-5