Abstract
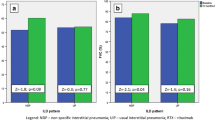
Progressive connective tissue disease (CTD)-related lung disease is a challenging condition that requires lung transplantation in some patients. Treatment with rituximab may improve lung function. To evaluate the effect of rituximab in patients with progressive CTD-related lung disease who met criteria for inclusion in waiting list for a lung transplant. Retrospective study of patients with progressive CTD-related lung disease with criteria for lung transplant (FVC < 60% and/or DLCO < 40%) that started treatment with rituximab because of disease progression. Clinical variables, pulmonary function tests and chest computed tomography were used to monitor the effect of rituximab. The cohort included 18 patients; systemic sclerosis (7), rheumatoid arthritis (5), systemic lupus erythematosus (4), Sjögren syndrome (1) and antisynthetase syndrome (1). The radiologic patterns observed were: usual interstitial pneumonia (1), non-specific interstitial pneumonia (9), lymphoid interstitial pneumonia (1), emphysema-usual interstitial pneumonia (1), shrinking lung syndrome (3) and undetermined pattern (3). Over the previous year to rituximab initiation a decline in FVC (− 3.8%, p = 0.095) and DLCO (− 8.4%, p = 0.004) was observed. After 2 years of treatment, DLCO significantly improved (+ 12.4%, p < 0.001 at 1 year and + 15.3%, p = 0.001 at 2 years). Six patients (33.3%) presented adverse events related to rituximab. No patient required lung transplant or died during the study period. Rituximab is an effective treatment for patients with severe and progressive CTD-related lung disease, which allows to delay lung transplantation in some cases.



Similar content being viewed by others
References
Marie I, Josse S, Hatron PY et al (2013) Interstitial lung disease in anti-Jo-1 patients with antisynthetase síndrome. Arthritis Care Res 65:800–808. https://doi.org/10.1002/acr.21895
Elhai M, Meune C, Avouac J, Kahan A, Allanore Y (2012) Trends in mortality in patients with systemic sclerosis over 40 years: a systematic review and metaanalysis of cohort studies. Rheumatology (Oxford) 51:1017–1026. https://doi.org/10.1093/rheumatology/ker269
Bongartz T, Nannini C, Medina-Velasquez YF et al (2010) Incidence and mortality of interstitial lung disease in rheumatoid arthritis: a population-based study. Arthritis Rheum 62:1583–1591. https://doi.org/10.1002/art.27405
Kim E, Collard H, King TE Jr (2009) Rheumatoid arthritis-associated interstitial lung disease, the relevance of histopathologic and radiographic pattern. Chest 136:1397–1405. https://doi.org/10.1378/chest.09-0444
Tashkin DP, Elashoff R, Clements PJ, Roth MD, Furst DE, Silver RM et al (2006) Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med 354:2655–2666. https://doi.org/10.1517/13543784.16.3.393
Tashkin DP, Roth MD, Clements PJ et al (2016) Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease (SLS II): a randomized controlled, double-blind, parallel group trial. Lancet Respir Med 4:708–719. https://doi.org/10.1016/S2213-2600(16)30152-7
Iqbal K, Kelly C (2015) Treatment of rheumatoid arthritis-associated interstitial lung disease: a perspective review. Ther Adv Musculoskel Dis 7:247–267. https://doi.org/10.1177/1759720X15612250
Francois A, Chatelus E, Wachsmann D et al (2013) B lymphocites and B-cell activating factor promote collagen and profibrotic markers expression by dermal fibroblasts in systemic sclerosis. Arthritis Res Ther 15:R168. https://doi.org/10.1186/ar4352
Atkins S, Turesson C, Myers J et al (2006) Morphologic and quantitative assessment of CD20+ B cell infiltrates in rheumatoid arthritis-associated nonspecific interstitial pneumonia and usual interstitial pneumonia. Arthritis Rheum 54:635–641. https://doi.org/10.1002/art.21758
Andersson H, Sem M, Lund MB et al (2015) Long-term experience with rituximab in anti-synthetase syndrome-related interstitial lung disease. Rheumatology 54:1420–1428. https://doi.org/10.1093/rheumatology/kev004
Daoussis D, Melissaropoulos K, Sakellaropoulos G et al (2016) A multicenter, open-label, comparative study of B-cell depletion therapy with Rituximab for systemic sclerosis-associated interstitial lung disease. Semin Arthritis Rheum. https://doi.org/10.1016/j.semarthrit.2016.10.003(Epub ahead of print)
Lepri G, Avouac J, Airò P et al (2016) Effects of rituximab in connective tissue disorders related interstitial lung disease. Clin Exp Rheumatol 34(Suppl 100):181–185
Peñacoba P, Corica ME, Mayos M et al (2014) Rituximab in the treatment of shrinking lung syndrome in systemic lupus erythematosus. Reumatol Clin 10:325–327. https://doi.org/10.1016/j.reuma.2013.09.003
Lacerda RI, Scheinberg MA, Formiga MY et al (2014) Use of rituximab as a treatment for systemic lupus erythematosus: retrospective review. Einstein 12:36–41. https://doi.org/10.1590/s1679-45082014ao2706
Sharp C, McCabe M, Dodds N et al (2016) Rituximab in autoimmune connective tissue disease-associated interstitial lung disease. Rheumatology 55:1318–1324. https://doi.org/10.1093/rheumatology/kew195
Giuggioli D, Lumetti F, Colaci M et al (2015) Rituximab in the treatment of patients with systemic sclerosis. Our experience and review of the literature. Autoimmun Rev 14:1072–1078. https://doi.org/10.1016/j.autrev.2015.07.008
Duron L, Cohen-Aubart F, Diot E et al (2016) Shrinking lung syndrome associated with systemic lupus erythematosus: a multicenter collaborative study of 15 new cases and a review of the 155 cases in the literature focusing on treatment response and long-term outcomes. Autoimmun Rev 15:994–1000. https://doi.org/10.1016/j.autrev.2016.07.021
Keir GJ, Maher TM, Ming D et al (2014) Rituximab in severe, tratment-refractory interstitial lung disease. Respirology 19:353–359. https://doi.org/10.1111/resp.12214
Fitzgerald DB, Moloney F, Twomey M et al (2015) Efficacy and safety of rituximab in connective tissue disease related interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis 32(3):215–221
Chen MH, Chen CK, Chou HP et al (2016) Rituximab therapy in primary Sjögren’s syndrome with interstitial lung disease: a retrospective cohort study. Clin Exp Rheumatol 34(6):1077–1084
Duarte AC, Cordeiro A, Fernandes BM et al (2019) Rituximab in connective tissue disease-associated interstitial lung disease. Clin Rheumatol 38(7):2001–2009. https://doi.org/10.1007/s10067-019-04557-7
Bennett D, Fossi A, Bargagli E et al (2015) Mortality on the waiting list for lung transplantation in patients with idiopathic pulmonary fibrosis: a single-centre experience. Lung 193:677–681. https://doi.org/10.1007/s00408-015-9767-x
He WX, Tang UL, Xia Y et al (2016) Outcomes of Chinese patients with end-stage pulmonary disease while awaiting lung transplantation: a single-center study. Chin Med J 129:3–7. https://doi.org/10.4103/0366-6999.172547
Paik HC, Haam SJ, Lee DY et al (2012) The fate of patients on the waiting list for lung transplantation in Korea. Transplant Proc 44:865–869. https://doi.org/10.1016/j.transproceed.2011.12.059
Higo H, Kurosaki T, Ichihara E et al (2017) Clinical charactersitics of Japanese candidates for lung transplant for interstitial lung disease and risk factors for early death while on the waiting list. Respir Investig 55:264–269. https://doi.org/10.1016/j.resinv.2017.03.002
American Thoracic Society, European Respiratory Society (2002) American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This Joint Statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS Board of Directors, June 2001 and by The ERS Executive Committee, June 2001. Am J Respir Crit Car Med 165:277–304. https://doi.org/10.1164/ajrccm.165.2.ats01
Roman A, Borro JM, Ussetti P et al (2011) Selección de pacientes candidatos a trasplante pulmonar. Arch Bronconeumol 47:303–309. https://doi.org/10.1016/j.arbres.2011.03.007
Saunders P, Tsipouri V, Keir GJ et al (2017) Rituximab versus cyclophosphamide for the treatment of connective tissue disease-associated interstitial lung disease (RECITAL): study protocol for a randomized controlled trial. Trials 18(1):275. https://doi.org/10.1186/s13063-017-2016-2
Ebata S, Yoshizaki A, Fukasawa T et al (2019) Rituximab therapy is more effective than cyclophosphamide therapy for Japanese patients with anti-topoisomerase I-positive systemic sclerosis-associated interstitial lung disease. J Dermatol 46(11):1006–1013. https://doi.org/10.1111/1346-8138.15079
Eberlein M (2013) Shrinking lung syndrome as a manifestation of pleuritis: are surface forces and surfactant the pathophysiological link ? J Rheumatol 40:1926. https://doi.org/10.3899/jrheum.130764
Pérez de Llano LA, Castro-Añon O, López MJ et al (2011) Shrinking lung syndrome caused by lupus myopathy. Q J Med 104:259–262. https://doi.org/10.1093/qjmed/hcq095
Jacobelli S, Moreno R, Massardo L et al (1985) Inspiratory muscle dysfunction and unexplained dyspnea in systemic lupus erythematosus. Arthritis Rheum 28:781–788. https://doi.org/10.1002/art.1780280709
Hawkins P, Davison AG, Dasgupta B et al (2001) Diaphragm strenght in acute systemic lupus erythematosus in a patient with paradoxical abdominal motion and reduced lung volumes. Thorax 56:329–330. https://doi.org/10.1136/thorax.56.4.329
Wilcox PG, Stein HB, Clarke SD et al (1988) Phrenic nerve function in patients with diaphragmatic weakness and systemic lupus erythematosus. Chest 93:352–358. https://doi.org/10.1378/chest.93.2.352
Henderson LA, Loring SH, Gill RR et al (2013) Shrinking lung syndrome as a manifestation of pleuritis: a new model based on pulmonary physiological studies. J Rheumatol 40:273–281. https://doi.org/10.3899/jrheum.121048
Borrell H, Narváez J, Alegre JJ et al (2016) Shrinking lung syndrome in systemic lupus erythematosus. Medicine 95:33(e4626). https://doi.org/10.1097/MD.0000000000004626
Acknowledgements
Authors would like to acknowledge the IDIBELL Department of Statistics for statistical support.
Author information
Authors and Affiliations
Contributions
RPA: acquisition, analysis and interpretation of data. Draft of the work. DJ: Revision of the manuscript. CI: acquisition and analysis of data. Revision of the manuscript. NJM: Revision of the manuscript. M-MM: conception and design of the work. Revision of the manuscript and final approval. NJ: conception and design of the work. Revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors state they have no conflict of interest and no relationship with pharmaceutical agencies promoting rituximab or other biologic treatment.
Ethical standards
The study was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference for Harmonization. The manuscript has been approved for its publication by the Clinical Research Ethics Committee of Bellvitge University Hospital (reference number PR406/17).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Robles-Perez, A., Dorca, J., Castellví, I. et al. Rituximab effect in severe progressive connective tissue disease-related lung disease: preliminary data. Rheumatol Int 40, 719–726 (2020). https://doi.org/10.1007/s00296-020-04545-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-020-04545-0