Abstract
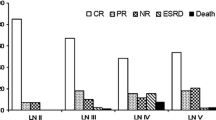
The objectives of the study were to investigate the pathological features and renal prognosis of severe lupus patients with rapidly progressive glomerulonephritis. One hundred and one cases of biopsy-proven severe LN with rapidly progressive glomerulonephritis (RPGN) were analyzed in this retrospective study. Another 200 severe LN patients without RPGN were randomly enrolled as a control group. Their clinicopathological data and long-term outcome were compared. There were 76 females and 25 males with an average age of 31.9 ± 14.2 years followed for a median period of 4 years. Compared with controls, patients with RPGN had shorter LN duration (p = 0.008), higher level of creatinine (p < 0.001), severe anemia (p = 0.037), heavier hematuria (p < 0.001), severe tubular injury parameters [NAG (p < 0.001), RBP (p < 0.001), C3 (p < 0.001)], higher scores of AI (p = 0.001) and CI (p = 0.004), higher proportions of glomerular sclerosis (0.033) and crescents (p < 0.001), severe tubulointerstitial lesions (p < 0.001) and interstitial inflammation (p < 0.001), lower rate of complete remission (33.9 vs 68.2 %) and higher rate of treatment failure (46.8 vs 7.9 %). The 3-, 5- and 10-year cumulative renal survival rates of RPGN and non-RPGN patients were 65.1 versus 53.9 versus 42.9 and 96.9 versus 94.9 versus 91.7 %, respectively. Multivariate analysis revealed that SCr concentration and the proportion of crescents were the most important risk factors for end-stage renal disease (ESRD) in severe LN with RPGN (p < 0.001). In conclusion, RPGN occurred in 3.6 % of LN and is associated with severe renal manifestations, serious sclerotic and crescentic glomeruli lesions, severe tubulointerstitial inflammation, atrophy and fibrosis, prominent leukocyte infiltration and worse treatment response. Multivariate analysis revealed that SCr concentration and the proportion of crescents were the most important risk factors for ESRD. 57.1 % of severe LN patients with RPGN might progress to ESRD within 10 years.


Similar content being viewed by others
References
Sumethkul V, Chalermsanyakorn P, Changsirikulchai S, Radinahamed P (2000) Lupus nephritis: a challenging cause of rapidly progressive crescentic glomerulonephritis. Lupus 9:424–428
Masani NN, Imbriano LJ, D’Agati VD, Markowitz GS (2005) Sle and rapidly progressive glomerulonephritis. Am J Kidney Dis 45:950–955
Jennette JC (2003) Rapidly progressive crescentic glomerulonephritis. Kidney Int 63:1164–1177
Glassock R (1978) A clinical and immunopathologic dissection of rapidly progressive glomerulonephritis. Nephron 22:253–264
Yeung C, Wong K, Wong W, Ng M, Chan K, Ng W (1984) Crescentic lupus glomerulonephritis. Clin Nephrol 21:251–258
Andrassy K, Küster S, Waldherr R, Ritz E (1991) Rapidly progressive glomerulonephritis: analysis of prevalence and clinical course. Nephron 59:206–212
Niaudet P (2000) Treatment of lupus nephritis in children. Pediatr Nephrol 14:158–166
Bogdanović R, Nikolić V, Pašić S, Dimitrijević J, Lipkovska-Marković J, Erić-Marinković J, Ognjanović M, Minić A, Stajić N (2004) Lupus nephritis in childhood: a review of 53 patients followed at a single center. Pediatr Nephrol 19:36–44
Weening JJ, D D’AGATI V, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F (2004) The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int 65:521–530
Mosca M, Pasquariello A, Tavoni A, Moriconi L, Moneta I, Innocenti M, Bencivelli W, Bombardieri S (1997) Predictors of renal outcome in diffuse proliferative glomerulonephritis in systemic lupus erythematosus. Lupus 6:371–378
Sumboonnanonda A, Vongjirad A, Suntornpoch V, Laohapand T, Parichatikanond P (1998) Renal pathology and long-term outcome in childhood sle. J Med Assoc Thail 81:830–834
Huong D, Papo T, Beaufils H, Wechsler B, Bletry O, Baumelou A, Godeau P, Piette J (1999) Renal involvement in systemic lupus erythematosus. A study of 180 patients from a single center. Medicine 78:148–166
Wang L-C, Yang Y-H, Lu M-Y, Chiang B-L (2003) Retrospective analysis of mortality and morbidity of pediatric systemic lupus erythematosus in the past two decades. J Microbiol Immunol Infect 36:203–208
Hochberg MC (1997) Updating the american college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Lewis EJ, Hunsicker LG, Lan S-P, Rohde RD, Lachin JM (1992) A controlled trial of plasmapheresis therapy in severe lupus nephritis. N Engl J Med 326:1373–1379
Chen YE, Korbet SM, Katz RS, Schwartz MM, Lewis EJ (2008) Value of a complete or partial remission in severe lupus nephritis. Clin J Am Soc Nephrol 3:46–53
Katz SM (1982) Renal disease: classification and atlas of glomerular diseases. JAMA 248(16):2053–2054
Austin H, Muenz LR, Joyce KM, Antonovych TT, Balow JE (1984) Diffuse proliferative lupus nephritis: identification of specific pathologic features affecting renal outcome. Kidney Int 25:689–695
Solez K, Axelsen R, Benediktsson H, Burdick JF, Cohen AH, Colvin RB, Croke BP, Droz D, Dunnill MS, Halloran PF (1993) International standardization of criteria for the histologic diagnosis of renal allograft rejection: the banff working classification of kidney transplant pathology. Kidney Int 44:411
Hsieh C, Chang A, Brandt D, Guttikonda R, Utset TO, Clark MR (2011) Predicting outcomes of lupus nephritis with tubulointerstitial inflammation and scarring. Arthritis Care Res 63:865–874
Banfi G, Bertani T, Boeri V, Faraggiana T, Mazzucco G, Monga G, Sacchi G (1991) Renal vascular lesions as a marker of poor prognosis in patients with lupus nephritis. Am J Kidney Dis 18:240–248
Appel G, Pirani C, D’Agati V (1994) Renal vascular complications of systemic lupus erythematosus. J Am Soc Nephrol 4:1499–1515
Descombes E, Droz D, Drouet L, Grünfeld J-P, Lesavre P (1997) Renal vascular lesions in lupus nephritis. Medicine 76:355–368
Schwartz M (1992) Lupus vasculitis. Contrib Nephrol 99:35
Illei GG, Austin HA, Crane M, Collins L, Gourley MF, Yarboro CH, Vaughan EM, Kuroiwa T, Danning CL, Steinberg AD (2001) Combination therapy with pulse cyclophosphamide plus pulse methylprednisolone improves long-term renal outcome without adding toxicity in patients with lupus nephritis. Ann Int Med 135:248–257
Chan T, Tse K, Tang CS, Lai K, Li F (2005) Long-term outcome of patients with diffuse proliferative lupus nephritis treated with prednisolone and oral cyclophosphamide followed by azathioprine. Lupus 14:265–272
Korbet SM, Lewis EJ, Schwartz MM, Reichlin M, Evans J, Rohde RD (2000) Factors predictive of outcome in severe lupus nephritis. Am J Kidney Dis 35:904–914
Mok CC, Ho CTK, Chan KW, Lau CS, Wong RWS (2002) Outcome and prognostic indicators of diffuse proliferative lupus glomerulonephritis treated with sequential oral cyclophosphamide and azathioprine. Arthritis Rheum 46:1003–1013
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH, Austin A, Bell A, Bloch DA, Corey PN, Decker JL (1992) Derivation of the sledai. A disease activity index for lupus patients. Arthritis Rheum 35:630–640
Moeller MJ, Smeets B (2013) Novel target in the treatment of rpgn: the activated parietal cell. Nephrol Dial Transpl 28:489–492
Keller F, Oehlenberg B, Kunzendorf U, Schwarz A, Offermann G (1989) Long-term treatment and prognosis of rapidly progressive glomerulonephritis. Clin Nephrol 31:190–197
Rees A, Cameron J (1998) Crescentic glomerulonephritis. In: Cameron JS, Davison AM, Grunfeld JP, Kerr D, Ritz E (eds) Oxford textbook of clinical nephrology, vol 1992. Oxford University Press, New York, pp 418–438
Ponticelli C, Imbasciati E, Brancaccio D, Tarantino A, Rivolta E (1974) Acute renal failure in systemic lupus erythematosus. Br Med J 3:716
Zhu D, Qu Z, Tan Y, Yu F, Zhao MH (2011) Acute kidney injury in chinese patients with lupus nephritis: a large cohort study from a single center. Lupus 20:1557–1565
Yu F, Tan Y, Liu G, Wang S-x, Zou W-z, Zhao M-h (2009) Clinicopathological characteristics and outcomes of patients with crescentic lupus nephritis. Kidney Int 76:307–317
Schwartz MM, Roberts JL, Lewis EJ (1983) Necrotizing glomerulitis of systemic lupus erythematosus. Hum Pathol 14:158–167
Ferrario F, Napodano P, Giordano A, Gandini E, Boeri R, D’Amico G (1992) Peculiar type of focal and segmental lupus glomerulitis: glomerulonephritis or vasculitis? Contrib Nephrol 99:86
Najafi CC, Korbet SM, Lewis EJ, Schwartz MM, Reichlin M, Evans J (2001) Significance of histologic patterns of glomerular injury upon long-term prognosis in severe lupus glomerulonephritis. Kidney Int 59:2156–2163
Hill GS, Delahousse M, Nochy D, Bariety J (2005) Class iv-s versus class iv-g lupus nephritis: clinical and morphologic differences suggesting different pathogenesis. Kidney Int 68:2288–2297
Mittal B, Hurwitz S, Rennke H, Singh AK (2004) New subcategories of class iv lupus nephritis: are there clinical, histologic, and outcome differences? Am J Kidney Dis 44:1050–1059
Schwartz MM, Korbet SM, Lewis EJ (2008) The prognosis and pathogenesis of severe lupus glomerulonephritis. Nephrol Dial Transpl 23:1298–1306
Schwartz M, Korbet S, Katz R, Lewis E (2009) Evidence of concurrent immunopathological mechanisms determining the pathology of severe lupus nephritis. Lupus 18:149–158
Behara VY, Whittier WL, Korbet SM, Schwartz MM, Martens M, Lewis EJ (2010) Pathogenetic features of severe segmental lupus nephritis. Nephrol Dial Transpl 25:153–159
Chen S, Tang Z, Zhang Y, Liu Z, Zhang H, Hu W (2013) Significance of histological crescent formation in patients with diffuse proliferative lupus nephritis. Am J Nephrol 38:445–452
Küster S, Apenberg S, Andrassy K, Ritz E (1992) Antineutrophil cytoplasmic antibodies in systemic lupus erythematosus. Contrib Nephrol 99:94
Sen D, Isenberg DA (2003) Antineutrophil cytoplasmic autoantibodies in systemic lupus erythematosus. Lupus 12:651–658
Nasr SH, D’Agati VD, Park H-R, Sterman PL, Goyzueta JD, Dressler RM, Hazlett SM, Pursell RN, Caputo C, Markowitz GS (2008) Necrotizing and crescentic lupus nephritis with antineutrophil cytoplasmic antibody seropositivity. Clin J Am Soc Nephrol 3:682–690
Jennette JC, Xiao H, Falk RJ (2006) Pathogenesis of vascular inflammation by anti-neutrophil cytoplasmic antibodies. J Am Soc Nephrol 17:1235–1242
Couser WG (1988) Rapidly progressive glomerulonephritis: classification, pathogenetic mechanisms, and therapy. Am J Kidney Dis 11:449–464
Li X, Chen N (2013) Management of crescentic glomerulonephritis: what are the recent advances. Contrib Nephrol 181:229–239
Tang Z, Yang G, Yu C, Yu Y, Wang J, Hu W, Zeng C, Chen H, Liu Z, Li L (2008) Effects of mycophenolate mofetil for patients with crescentic lupus nephritis. Nephrology 13:702–707
Davies RJ, Sangle SR, Jordan NP, Aslam L, Lewis MJ, Wedgwood R, D’Cruz DP (2013) Rituximab in the treatment of resistant lupus nephritis: therapy failure in rapidly progressive crescentic lupus nephritis. Lupus 22:574–582
Sinha A, Puri K, Hari P, Dinda AK, Bagga A (2013) Etiology and outcome of crescentic glomerulonephritis. Indian Pediatr 50:283–288
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, S., Chen, H., Liu, Z. et al. Pathological spectrums and renal prognosis of severe lupus patients with rapidly progressive glomerulonephritis. Rheumatol Int 35, 709–717 (2015). https://doi.org/10.1007/s00296-014-3140-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-014-3140-x