Abstract
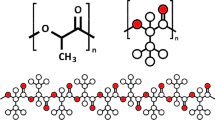
Recycled duck bones (DBs) and fish shells were processed into natural derivatives. Through innovative design, these natural derivatives were then combined with biocompatible polymer to create a new type of ecofriendly filament suitable for three-dimensional (3D) printing of scaffolds for bone regeneration. The DBs and fish shells were thermally processed to produce DB-derived hydroxyapatite (HA) and fish shell-derived Ca(OH)2 (TAS), respectively. Poly(ε-caprolactone) (PCL), HA, and TAS were combined and fabricated into new composite filaments, which were then transformed into scaffolds using 3D printing technology. The structure and antibacterial behaviors of the obtained composite scaffolds were studied. Alone, PCL showed no bacterial inhibition. MHA (a mix of 4, 8, 12, 16 wt%-HA and 0.8 wt% TAS) was added to PCL to form a PCL/MHA composite material, which significantly improved the functional properties of PCL and enhanced cell attachment and proliferation. The Ca(OH)2 content of TAS was responsible for the antibacterial effect. The PCL/MHA composites were porous and displayed enhanced osteoblast proliferation in vitro. The osteoblast cell population do not affected when cultured on the PCL/HA and PCL/MHA series composites according to cell cycle distribution analysis. The surfaces of the various PCL/HA and PCL/MHA composites showed elevated levels of calcium and phosphorus compounds when exposed to simulated body fluids. Calcium and phosphate ions were rapidly deposited on PCL/HA and PCL/MHA composite scaffolds in osteoblasts according to the cell mineralization assay. Our findings suggest great potential of the PCL/HA and PCL/MHA composite scaffolds in bone tissue engineering applications.










Similar content being viewed by others
References
Zhao Y, Wang Z, Zhao J, Hussain M, Wang M (2022) Additive manufacturing in orthopedics: a review. ACS Biomater Sci Eng 8(4):1367–1380. https://doi.org/10.1021/acsbiomaterials.1c01072
Liu H, Chen J, Qiao S, Zhang W (2022) Carbon-based nanomaterials for bone and cartilage regeneration: a review. ACS Biomater Sci Eng 7(10):4718–4735. https://doi.org/10.1021/acsbiomaterials.1c00759
Jishita Ravoor J, Mahendran Thangavel M, Renold Elsen S (2021) Comprehensive review on design and manufacturing of bio-scaffolds for bone reconstruction. ACS Appl Bio Mater 4(12):8129–8158. https://doi.org/10.1021/acsabm.1c00949
Zhang M, Liu J, Zhu T, Le H, Wang X, Guo J, Liu G, Ding J (2022) Functional macromolecular adhesives for bone fracture healing. ACS Appl Mater Interfaces 14(1):1–19. https://doi.org/10.1021/acsami.1c17434
Veiga A, Castro F, Rocha F, Oliveira AL (2020) Protein-based hydroxyapatite materials: tuning composition toward biomedical applications. ACS Appl Bio Mater 3(6):3441–3455. https://doi.org/10.1021/acsabm.0c00140
Ambekar RS, Kandasubramanian B (2019) Progress in the advancement of porous biopolymer scaffold: tissue engineering application. Ind Eng Chem Res 58(16):6163–6194. https://doi.org/10.1021/acs.iecr.8b05334
Bahraminasab M, Janmohammadi M, Arab S, Talebi A, Nooshabadi VT, Koohsarian P, Nourbakhsh MS (2021) Bone scaffolds: an incorporation of biomaterials, cells, and biofactors. ACS Biomater Sci Eng 7(12):5397–5431. https://doi.org/10.1021/acsbiomaterials.1c00920
Kirillova A, Yeazel TR, Asheghali D, Petersen SR, Dort S, Gall K, Becker ML (2021) Fabrication of biomedical scaffolds using biodegradable polymers. Chem Rev 121(18):11238–11304. https://doi.org/10.1021/acs.chemrev.0c01200
Moore KM, Murthy AB, Graham-Gurysh EG, Hingtgen SD, Bachelder EM, Ainslie KM (2020) Polymeric biomaterial scaffolds for tumoricidal stem cell glioblastoma therapy. ACS Biomater Sci Eng 6(7):3762–3777. https://doi.org/10.1021/acsbiomaterials.0c00477
Jing L, Wang X, Leng B, Zhan N, Liu H, Wang S, Lu Y, Sun J, Huang D (2021) Engineered nanotopography on the microfibers of 3D-printed PCL scaffolds to modulate cellular responses and establish an in vitro tumor model. ACS Appl Bio Mater 4(2):1381–1394. https://doi.org/10.1021/acsabm.0c01243
Lin GB, Ma PX (2014) Synthetic biodegradable functional polymers for tissue engineering: a brief review. Sci China Chem 57(4):490–500. https://doi.org/10.1007/s11426-014-5086-y
Xu Y, Meng Q, Jin X, Liu F, Yu J (2020) Biodegradable scaffolds for urethra tissue engineering based on 3D printing. ACS Appl Bio Mater 3(4):2007–2016. https://doi.org/10.1021/acsabm.9b01151
Xu N, Ye X, Wei D, Zhong J, Chen Y, Xu G, He D (2014) 3D artificial bones for bone repair prepared by computed tomography-guided fused deposition modeling for bone repair. ACS Appl Mater Interfaces 6(17):14952–14963. Doi:https://doi.org/10.1021/am502716t.
Thijssen Q, Cornelis K, Alkaissy R, Locs J, Damme LV, Schaubroeck D, Willaert R, Snelling S, Mouthuy PA, Vlierberghe SV (2022) Tough photo-cross-linked PCL-hydroxyapatite composites for bone tissue engineering. Biomacromol 23(3):1366–1375. https://doi.org/10.1021/acs.biomac.1c01584
Cestari F, Petretta M, Yang Y, Motta A, Grigolo B, Sglava VM (2021) 3D printing of PCL/nano-hydroxyapatite scaffolds derived from biogenic sources for bone tissue engineering. Sustain Mater Technol 29: e00318. https://doi.org/10.1016/j.susmat.2021.e00318.
Cho YS, Choi S, Lee SH, Kim KK, Cho YS (2019) Assessments of polycaprolactone/hydroxyapatite composite scaffold with enhanced biomimetic mineralization by exposure to hydroxyapatite via a 3D-printing system and alkaline erosion. Eur Polym J 113:340–348. https://doi.org/10.1016/j.eurpolymj.2019.02.006
Tülü G, Kaya BÜ, Çetin ES, Köle M (2021) Antibacterial effect of silver nanoparticles mixed with calcium hydroxide or chlorhexidine on multispecies biofilms. Odontology 109:802–811. https://doi.org/10.1007/s10266-021-00601-8
Rahul VG, Wilson J, Thomas LV, Nair PD (2022) Assessing the 3D printability of an elastomeric poly(caprolactone-co-lactide) copolymer as a potential material for 3D printing tracheal scaffolds. ACS Omega 7(8):7002–7011. https://doi.org/10.1021/acsomega.1c06679
Bisht B, Hope A, Mukherjee A, Paul MK (2021) Advances in the fabrication of scaffold and 3D printing of biomimetic bone graft. Ann Biomed Eng 49(4):1128–1150. https://doi.org/10.1007/s10439-021-02752-9
Bahraminasab M (2020) Challenges on optimization of 3D-printed bone scaffolds. Biomed Eng Online 19:69. https://doi.org/10.1186/s12938-020-00810-2
Zhongxing L, Shaohong W, Jinlong L, Limin Z, Yuanzheng W, Haipeng G, Jian C (2021) Three-dimensional printed hydroxyapatite bone tissue engineering scaffold with antibacterial and osteogenic ability. J Med Biol Eng 15:21. https://doi.org/10.1186/s13036-021-00273-6
Beheshtizadeh N, Lotfibakhshaiesh N, Pazhouhnia Z, Hoseinpour M, Nafari M (2020) A review of 3D bio-printing for bone and skin tissue engineering: a commercial approach. J Mater Sci 55:3729–3749. https://doi.org/10.1007/s10853-019-04259-0
Whitaker R, Hernaez-Estrada B, Hernandez RM, Santos-Vizcaino E, Spiller KL (2021) Immunomodulatory biomaterials for tissue repair. Chem Rev 121(18):11305–11335. https://doi.org/10.1021/acs.chemrev.0c00895
Seims KB, Hunt NK, Chow LW (2021) Strategies to control or mimic growth factor activity for bone, cartilage, and osteochondral tissue engineering. Bioconjugate Chem 32(5):861–878. https://doi.org/10.1021/acs.bioconjchem.1c00090
Wu CS, Wang SS, Wu DY, Shih WL (2021) Novel composite 3D-printed filament made from fish scale-derived hydroxyapatite, eggshell and polylactic acid via a fused fabrication approach. Addit Manuf 46:102169. https://doi.org/10.1016/j.addma.2021.102169
Wu CS, Wu DY, Wang SS (2021) Biodegradable composite containing fish-scale extracts. ACS Appl Bio Mater 4(1):462–469. https://doi.org/10.1021/acsabm.0c00955
Feng P, Wang K, Shuai Y, Peng S, Hu Y, Shuai C (2022) Hydroxyapatite nanoparticles in situ grown on carbon nanotube as a reinforcement for poly (ε-caprolactone) bone scaffold. Mater Today Adv 15:100272
Rathinavel S, Korrapati PS, Kalaiselvi P, Dharmalingam S (2021) Mesoporous silica incorporated PCL/curcumin nanofiber for wound healing application. Eur J Pharm Sci 167:106021. https://doi.org/10.1016/j.ejps.2021.106021
Son JS, Jang SH, Kwon TY, Kim KH, Kang SS, Choi SH (2014) Preliminary evaluation of bone graft substitute produced by bone of duck beak. Mater Lett 121:181–184. https://doi.org/10.1016/j.matlet.2014.01.141
Samanta A, Podder S, Ghosh CK, Bhattacharya M, Ghosh J, Mallik AK, Dey A, Mukhopadhyay AK (2017) ROS mediated high anti-bacterial efficacy of strain tolerant layered phase pure nano-calcium hydroxide. J Mech Behav Biomed Mater 72:110–112. https://doi.org/10.1016/j.jmbbm.2017.04.004
Silva M, Baltrus JP, Burnett DJ, Baltrusaitis J (2022) Water adsorption on hydroxyapatite and struvite as a function of relative humidity: application of BET and freundlich adsorption models. ACS Earth Space Chem 6:431–443. https://doi.org/10.1021/acsearthspacechem.1c00406
Contreras-Jimenez B, Gaytan-Martinez M, JdeD F-C, Avalos-Zuniga RA, Morales-Sanchez E (2014) Effect of steeping time and calcium hydroxide concentration on the water absorption and pasting profile of corn grits. J Food Eng 122:72–77. https://doi.org/10.1016/j.jfoodeng.2013.09.005
Zalewska J, Przekora A, Pałka K, Belcarz A (2022) Gypsum-related compensation of ions uptake by highly porous hydroxyapatite ceramics: consequences for osteoblasts growth and proliferation. Biomater Adv 133: 112665. https://doi.org/10.1016/j.msec.2022.112665
Hernandez-Ruiz KL, Lopez-Cervantes J, Sanchez-Machado DI, Martinez-Macias MdelR, Correa-Murrieta MaA, Sanches-Silva A (2022) Hydroxyapatite recovery from fish byproducts for biomedical applications. Sustain Chem Pharm 28: 100726. https://doi.org/10.1016/j.scp.2022.100726.
Wang H, Li X, Zhu Z, Wang H, Wei B, Bai X (2020) Hydrogen sulfide promotes lipopolysaccharide-induced apoptosis of osteoblasts by inhibiting the AKT/NF-kB signaling pathway. Biochem Biophys Res Commun 524:832–838. https://doi.org/10.1016/j.bbrc.2020.02.005
Chen M, Sun Y, Hou Y, Luo Z, Li M, Wei Y, Chen M, Tan L, Cai K, Hu Y (2022) Constructions of ROS-responsive titanium-hydroxyapatite implant for mesenchymal stem cell recruitment in peri-implant space and bone formation in osteoporosis microenvironment. Bioact Mater 18:56–71. https://doi.org/10.1016/j.bioactmat.2022.02.006
Liang B, Feng T, Yuan X, Zhao K, Li C, Han Y (2022) Proportion-dependent osteogenic activity of electrospun nanohydroxyapatite/polylactic acid fiber membrane in vitro and in vivo. Mater Des 219:110834
Chen Y, Li ZH, Zhou MR, Wu XC, Zhu ZH, Zhang JP, Xu JG, Ding DF (2022) A comparative analysis of the osteogenic capacity of osteoblasts from newborn and two-week-old rats. Acta Histochem 124:151858. https://doi.org/10.1016/j.acthis.2022.151858
Surya P, Nithin A, Sundaramanickam A, Sathish M (2021) Synthesis and characterization of nano-hydroxyapatite from Sardinella longiceps fish bone and its effects on human osteoblast bone cells. J Mech Behav Biomed Mater 119:104501. https://doi.org/10.1016/j.jmbbm.2021.104501
Narita H, Itoh S, Imazato S, Yoshitake F, Ebisu S (2010) An explanation of the mineralization mechanism in osteoblasts induced by calcium hydroxide. Acta Biomater 6:586–590. https://doi.org/10.1016/j.actbio.2009.08.005
Aghajanpour S, Esfandyari-Manesh M, Ghahri T, Ghahremani MH, Atyabi F, Heydari M, Motasadizadeh H, Dinarvand R (2022) Impact of oxygen-calcium-generating and bone morphogenetic protein-2 nanoparticles on survival and differentiation of bone marrow-derived mesenchymal stem cells in the 3D bio-printed scaffold. Colloids Surf B 216:112581. https://doi.org/10.1016/j.colsurfb.2022.112581
Lam NT, Quan VM, Boonrungsiman S, Sukyai P (2022) Effectiveness of bio-dispersant in homogenizing hydroxyapatite for proliferation and differentiation of osteoblast. J Colloid Interface Sci 611:491–502. https://doi.org/10.1016/j.jcis.2021.12.088
Vargas-Becerril N, Sánchez-Téllez DA, Zarazúa-Villalobos L, González-García DM, Álvarez-Pérez MA, de León-Escobedo C, Téllez-Jurado L (2020) Structure of biomimetic apatite grown on hydroxyapatite (HA). Ceram Int 46:28806–28813. https://doi.org/10.1016/j.ceramint.2020.08.044
Yilmaz B, Pazarceviren AE, Tezcaner A, Evis Z (2020) Historical development of simulated body fluids used in biomedical applications: a review. Microchem. J. 155:104713. https://doi.org/10.1016/j.microc.2020.104713
Saranti A, Tiron-Stathopoulos A, Papaioannou L, Gioti C, Ioannou A, Karakassides MA, Avgoustakis K, Koutselas I, Dimos K (2022) 3D-printed bioactive scaffolds for bone regeneration bearing carbon dots for bioimaging purposes. Smart Mater Med 3:12–19. https://doi.org/10.1016/j.smaim.2021.11.002
You BC, Meng CE, Nasir NFM, Tarmizi EZM, Fhan KS, Kheng ES, Majid MSA, Jamir MRM (2022) Dielectric and biodegradation properties of biodegradable nano-hydroxyapatite/starch bone scaffold. J Mater Res Technol 18:3215–3226
Teoh YY, Athanassiadis B, Walsh LJ (2018) Comparison of commercial calcium hydroxide pastes for prolonged antibacterial effect using a colourimetric assessment. Mater 11(3):348. https://doi.org/10.3390/ma11030348
Acknowledgements
The author sincerely appreciate projects sponsored by Ministry of Science and Technology (Taiwan, No. MOST 111-2221-E-244-001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, CS., Shih, WL. & Wang, SS. 3D-printed filament composing duck bones, fish shells, and poly(ε-caprolactone) via a fused fabrication: characterization, functionality, and application. Polym. Bull. 81, 5193–5214 (2024). https://doi.org/10.1007/s00289-023-04960-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-023-04960-w