Abstract
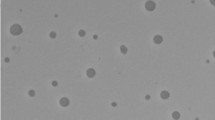
Azelaic acid (AA), a promising agent for acne and hyperpigmentation disorders, is associated with side effects viz. rashes, skin irritation, dryness, burning and stinging. Its poor solubility also pose challenge in the development of suitable formulation. Therefore, this research was aimed to design cyclodextrin nanosponges (CDNS) of AA to address above-mentioned challenges. Herein, the fabrication of CDNS by melt method was demonstrated employing β-cyclodextrin (β-CD) as polymer and diphenyl carbonate (DPC) as a cross-linker. AA was loaded in CDNS via lyophilization and appropriately characterized by Fourier transform infrared spectroscopy, thermogravimetric analysis, X-ray powder diffraction and nuclear magnetic resonance. For morphological evaluation, field emission scanning electron and transmission electron microscopy were also performed. The particle size of AANS was in nanorange, with acceptable zeta potential, low polydispersity index and delayed release. The safety of the nanoformulation was assessed using Human Epidermal Keratinocyte cell lines. Further, molecular docking studies for AA was carried out. In vitro antibacterial, antioxidant and antityrosinase assay were also conducted for prepared nanoformulation. The results of all the studies performed revealed that encapsulation of AA in nanosponges led to improvement in efficacy of drug in terms of solubility, release and safety, with adequate antimicrobial, antioxidant and antityrosinase activity.










Similar content being viewed by others
References
Jones G (2010) Beauty imagined: a history of the global beauty industry. Oxford University Press, Oxford
Seo YK, Kim SJ, Boo YC et al (2011) Effects of p-coumaric acid on erythema and pigmentation of human skin exposed to ultraviolet radiation. Clin Exp Dermatol Clin Dermatol 36:260–266
Singh BK, Park SH, Lee H-B et al (2016) Kojic acid peptide: a new compound with anti-tyrosinase potential. Ann Dermatol 28:555–561
Boo YC (2019) p-Coumaric acid as an active ingredient in cosmetics: a review focusing on its antimelanogenic effects. Antioxidants 8:275
Ghanbarzadeh S, Hariri R, Kouhsoltani M et al (2015) Enhanced stability and dermal delivery of hydroquinone using solid lipid nanoparticles. Colloids Surf B Biointerfaces 136:1004–1010
Rendon MI (2004) Utilizing combination therapy to optimize melasma outcomes. J Drugs Dermatol JDD 3:S27–34
Jow T, Hantash BM (2014) Hydroquinone-induced depigmentation: case report and review of the literature. Dermatitis 25:e1–e5
Lima LL, Lima RM, da Silva AF et al (2013) Azastilbene analogs as tyrosinase inhibitors: new molecules with depigmenting potential. Sci World J. https://doi.org/10.1155/2013/274643
Cabanes J, Chazarra S, Garcia-Carmona F (1994) Kojic acid, a cosmetic skin whitening agent, is a slow-binding inhibitor of catecholase activity of tyrosinase. J Pharm Pharmacol 46:982–985
Maeda K, Fukuda M (1996) Arbutin: mechanism of its depigmenting action in human melanocyte culture. J Pharmacol Exp Ther 276:765–769
Hu Z-M, Zhou Q, Lei T-C et al (2009) Effects of hydroquinone and its glucoside derivatives on melanogenesis and antioxidation: biosafety as skin whitening agents. J Dermatol Sci 55:179–184
Pillaiyar T, Manickam M, Namasivayam V (2017) Skin whitening agents: medicinal chemistry perspective of tyrosinase inhibitors. J Enzym Inhib Med Chem 32:403–425
Desmedt B, Courselle P, De Beer JO et al (2016) Overview of skin whitening agents with an insight into the illegal cosmetic market in Europe. J Eur Acad Dermatol Venereol 30:943–950
Stinco G, Bragadin G, Trotter D et al (2007) Relationship between sebostatic activity, tolerability and efficacy of three topical drugs to treat mild to moderate acne. J Eur Acad Dermatol Venereol JEADV 21:320–325. https://doi.org/10.1111/j.1468-3083.2006.01914.x
Reis C, Gomes A, Rijo P et al (2013) Evaluation of a new topical treatment for acne with azelaic acid-loaded nanoparticles. Microsc Microanal Off J Microsc Soc Am Microbeam Anal Soc Microsc Soc Can 19:1–10. https://doi.org/10.1017/S1431927613000536
Liu C-H, Huang H-Y (2012) Antimicrobial activity of curcumin-loaded myristic acid microemulsions against Staphylococcus epidermidis. Chem Pharm Bull (Tokyo) 60:1118–1124. https://doi.org/10.1248/cpb.c12-00220
Nguyen QH, Bui TP (1995) Azelaic acid: pharmacokinetic and pharmacodynamic properties and its therapeutic role in hyperpigmentary disorders and acne. Int J Dermatol 34:75–84
Halder RM, Richards GM (2004) Topical agents used in the management of hyperpigmentation. Skin Ther Lett 9:1–3
Kumar A, Rao R, Yadav P (2019) Azelaic acid: a promising agent for dermatological applications. Curr Drug Ther. https://doi.org/10.2174/1574885514666190904160228
Oge LK, Muncie HL, Phillips-Savoy AR (2015) Rosacea: diagnosis and treatment. Am Fam Physician 92:187–196
Grimes PE (2009) Management of hyperpigmentation in darker racial ethnic groups. Semin Cutan Med Surg 28(2):77–85
Töpert M, Rach P, Siegmund F (1989) Pharmacology and toxicology of azelaic acid. Acta Derm Venereol Suppl (Stockh) 143:14–19
Müller RH, MaÈder K, Gohla S (2000) Solid lipid nanoparticles (SLN) for controlled drug delivery—a review of the state of the art. Eur J Pharm Biopharm 50:161–177
Kumar S, Rao R (2019) Analytical tools for cyclodextrin nanosponges in pharmaceutical field: a review. J Incl Phenom Macrocycl Chem 94:1–20
Hollman PH, Katan MB (1999) Dietary flavonoids: intake, health effects and bioavailability. Food Chem Toxicol 37:937–942
Kumar S, Trotta F, Rao R (2018) Encapsulation of babchi oil in cyclodextrin-based nanosponges: physicochemical characterization, photodegradation, and in vitro cytotoxicity studies. Pharmaceutics 10:169
Pushpalatha R, Selvamuthukumar S, Kilimozhi D (2018) Cross-linked, cyclodextrin-based nanosponges for curcumin delivery—physicochemical characterization, drug release, stability and cytotoxicity. J Drug Deliv Sci Technol 45:45–53. https://doi.org/10.1016/j.jddst.2018.03.004
Garrido B, González S, Hermosilla J et al (2019) Carbonate-β-cyclodextrin-based nanosponge as a nanoencapsulation system for piperine: physicochemical characterization. J Soil Sci Plant Nutr 19:620–630. https://doi.org/10.1007/s42729-019-00062-7
Anandam S, Selvamuthukumar S (2014) Fabrication of cyclodextrin nanosponges for quercetin delivery: physicochemical characterization, photostability, and antioxidant effects. J Mater Sci 49:8140–8153
Ramírez-Ambrosi M, Caldera F, Trotta F et al (2014) Encapsulation of apple polyphenols in β-CD nanosponges. J Incl Phenom Macrocycl Chem 80:85–92. https://doi.org/10.1007/s10847-014-0393-7
Swaminathan S, Vavia PR, Trotta F et al (2013) Structural evidence of differential forms of nanosponges of beta-cyclodextrin and its effect on solubilization of a model drug. J Incl Phenom Macrocycl Chem 76:201–211
Rao M, Bajaj A, Khole I et al (2013) In vitro and in vivo evaluation of β-cyclodextrin-based nanosponges of telmisartan. J Incl Phenom Macrocycl Chem 77:135–145. https://doi.org/10.1007/s10847-012-0224-7
Hua S (2014) Comparison of in vitro dialysis release methods of loperamide-encapsulated liposomal gel for topical drug delivery. Int J Nanomed 9:735
ElMeshad AN, Mortazavi SM, Mozafari MR (2014) Formulation and characterization of nanoliposomal 5-fluorouracil for cancer nanotherapy. J Liposome Res 24:1–9
Patel N, Padia N, Vadgama N et al (2016) Formulation and evaluation of microsponge gel for topical delivery of fluconazole for fungal therapy. J Pharm Investig 46:221–238
Rajeshwari HR, Dhamecha D, Jagwani S et al (2017) Formulation of thermoreversible gel of cranberry juice concentrate: evaluation, biocompatibility studies and its antimicrobial activity against periodontal pathogens. Mater Sci Eng C 75:1506–1514
Kumar PM, Ghosh A (2017) Development and evaluation of silver sulfadiazine loaded microsponge based gel for partial thickness (second degree) burn wounds. Eur J Pharm Sci 96:243–254
RCSB PDB - Search Results. https://www.rcsb.org/pdb/results/results.do?tabtoshow=Current&qrid=31D5FFB5. Accessed 25 Feb 2020
Huey R, Morris GM, Olson AJ, Goodsell DS (2007) A semiempirical free energy force field with charge-based desolvation. J Comput Chem 28:1145–1152
Dhakar NK, Caldera F, Bessone F et al (2019) Evaluation of solubility enhancement, antioxidant activity, and cytotoxicity studies of kynurenic acid loaded cyclodextrin nanosponge. Carbohydr Polym 224:115168
Ansari KA, Vavia PR, Trotta F, Cavalli R (2011) Cyclodextrin-based nanosponges for delivery of resveratrol: in vitro characterisation, stability, cytotoxicity and permeation study. AAPS PharmSciTech 12:279. https://doi.org/10.1208/s12249-011-9584-3
Zainuddin R, Zaheer Z, Sangshetti JN, Momin M (2017) Enhancement of oral bioavailability of anti-HIV drug rilpivirine HCl through nanosponge formulation. Drug Dev Ind Pharm 43:2076–2084
Padamwar MN, Pokharkar VB (2006) Development of vitamin loaded topical liposomal formulation using factorial design approach: drug deposition and stability. Int J Pharm 320:37–44
Hsieh P-W, Al-Suwayeh SA, Fang C-L et al (2012) The co-drug of conjugated hydroquinone and azelaic acid to enhance topical skin targeting and decrease penetration through the skin. Eur J Pharm Biopharm 81:369–378. https://doi.org/10.1016/j.ejpb.2012.03.006
Organic Spectroscopy International. https://orgspectroscopyint.blogspot.com/. Accessed 19 Feb 2020
Olteanu AA, Aramă C-C, Radu C et al (2014) Effect of β-cyclodextrins based nanosponges on the solubility of lipophilic pharmacological active substances (repaglinide). J Incl Phenom Macrocycl Chem 80:17–24
Boukamp P, Petrussevska RT, Breitkreutz D et al (1988) Normal keratinization in a spontaneously immortalized aneuploid human keratinocyte cell line. J Cell Biol 106:761–771
Schürer N, Köhne A, Schliep V et al (1993) Lipid composition and synthesis of HaCaT cells, an immortalized human keratinocyte line, in comparison with normal human adult keratinocytes. Exp Dermatol 2:179–185
Charnock C, Brudeli B, Klaveness J (2004) Evaluation of the antibacterial efficacy of diesters of azelaic acid. Eur J Pharm Sci 21:589–596
Leeming JP, Holland KT, Bojar RA (1986) The in vitro antimicrobial effect of azelaic acid. Br J Dermatol 115:551–556
Holland KT, Bojar RA (1993) Antimicrobial effects of azelaic acid. J Dermatol Treat 4:S8–S11
Al-Marabeh S, Khalil E, Khanfar M et al (2017) A prodrug approach to enhance azelaic acid percutaneous availability. Pharm Dev Technol 22:578–586. https://doi.org/10.1080/10837450.2016.1200614
Lowe NJ, Rizk D, Grimes P et al (1998) Azelaic acid 20% cream in the treatment of facial hyperpigmentation in darker-skinned patients. Clin Ther 20:945–959
Sahoo NG, Kakran M, Shaal LA et al (2011) Preparation and characterization of quercetin nanocrystals. J Pharm Sci 100:2379–2390
Sapino S, Carlotti ME, Cavalli R et al (2013) Photochemical and antioxidant properties of gamma-oryzanol in beta-cyclodextrin-based nanosponges. J Incl Phenom Macrocycl Chem 75:69–76
Chawla S, DeLong MA, Visscher MO et al (2008) Mechanism of tyrosinase inhibition by deoxyarbutin and its second-generation derivatives. Br J Dermatol 159:1267–1274
Sharma VK, Choi J, Sharma N et al (2004) In vitro anti-tyrosinase activity of 5-(hydroxymethyl)-2-furfural isolated from Dictyophora indusiata. Phytother Res Int J Devoted Pharmacol Toxicol Eval Nat Prod Deriv 18:841–844
Acknowledgements
The researchers would like to acknowledge Dr. APJ Abdul Kalam central instrument laboratory, Department of Pharmaceutical Sciences, Guru Jambheshwar University of Science and Technology, Hisar for providing necessary facilities for present investigation. Jay Chem Marketing, Mumbai is also acknowledged for providing a gift sample of β-cyclodextrin. The authors also wish to thank Dr. Ajmer Singh, Department of pharmaceutical sciences, Chitkara university, Rajpura (India) for molecular docking studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumar, A., Rao, R. Enhancing efficacy and safety of azelaic acid via encapsulation in cyclodextrin nanosponges: development, characterization and evaluation. Polym. Bull. 78, 5275–5302 (2021). https://doi.org/10.1007/s00289-020-03366-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-020-03366-2