Abstract
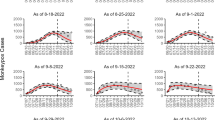
The global impact of COVID-19 has heightened concerns about emerging viral infections, among which monkeypox (MPOX) has become a significant public health threat. To address this, our study employs a comprehensive approach using three statistical techniques: Distribution fitting, ARIMA modeling, and Random Forest machine learning to analyze and predict the spread of MPOX in the top ten countries with high infection rates. We aim to provide a detailed understanding of the disease dynamics and model theoretical distributions using country-specific datasets to accurately assess and forecast the disease’s transmission. The data from the considered countries are fitted into ARIMA models to determine the best time series regression model. Additionally, we employ the random forest machine learning approach to predict the future behavior of the disease. Evaluating the Root Mean Square Errors (RMSE) for both models, we find that the random forest outperforms ARIMA in six countries, while ARIMA performs better in the remaining four countries. Based on these findings, robust policy-making should consider the best fitted model for each country to effectively manage and respond to the ongoing public health threat posed by monkeypox. The integration of multiple modeling techniques enhances our understanding of the disease dynamics and aids in devising more informed strategies for containment and control.





Similar content being viewed by others
References
Tiwari PK, Rai RK, Khajanchi S, Gupta RK, Misra AK (2021) Dynamics of coronavirus pandemic: effects of community awareness and global information campaigns. Eur Phys J Plus 136(10):994. https://doi.org/10.1140/epjp/s13360-021-01997-6
Cho CT, Wenner HA (1973) Monkeypox virus. Bacteriol Rev 37(1):1–18. https://doi.org/10.1128/br.37.1.1-18.1973
Magnus PV, Andersen EK, Petersen KB, Birch-Andersen A (2009) A pox-like disease in cynomolgus monkeys. Acta Pathol Microbiol Scand 46(2):156–176. https://doi.org/10.1111/j.1699-0463.1959.tb00328.x
Odom MR, Curtis Hendrickson R, Lefkowitz EJ (2009) Poxvirus protein evolution: family wide assessment of possible horizontal gene transfer events. Virus Res 144(1–2):233–249. https://doi.org/10.1016/j.virusres.2009.05.006
Diven DG (2001) An overview of poxviruses. J Am Acad Dermatol 44(1):1–16. https://doi.org/10.1067/mjd.2001.109302
Vivancos R, Anderson C, Blomquist P, Balasegaram S, Bell A, Bishop L, Brown CS, Chow Y, Edeghere O, Florence I, Logan S, Manley P, Crowe W, McAuley A, Shankar AG, Mora-Peris B, Paranthaman K, Prochazka M, Ryan C et al (2022) Community transmission of monkeypox in the United Kingdom, April to May 2022. Eurosurveillance. https://doi.org/10.2807/1560-7917.ES.2022.27.22.2200422
World Health Organization. Mpox (Monkeypox) outbreak: global trends, world health organization (2022) https://worldhealthorg.shinyapps.io/MPOX_global/. Accessed 20 Dec 2022
Adler H, Gould S, Hine P, Snell LB, Wong W, Houlihan CF, Osborne JC, Rampling T, Beadsworth MB, Duncan CJ, Dunning J, Fletcher TE, Hunter ER, Jacobs M, Khoo SH, Newsholme W, Porter D, Porter RJ, Ratcliffe L et al (2022) Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis 22(8):1153–1162. https://doi.org/10.1016/S1473-3099(22)00228-6
Miura F, van Ewijk CE, Backer JA, Xiridou M, Franz E, Op de Coul E, Brandwagt D, van Cleef B, van Rijckevorsel G, Swaan C, van den Hof S, Wallinga J (2022) Estimated incubation period for monkeypox cases confirmed in the Netherlands. EuroSurveillance 27(24):2200448. https://doi.org/10.2807/1560-7917.ES.2022.27.24.2200448
Rao AK, Schulte J, Chen T-H, Hughes CM, Davidson W, Neff JM, Markarian M, Delea KC, Wada S, Liddell A, Alexander S, Sunshine B, Huang P, Honza HT, Rey A, Monroe B, Doty J, Christensen B, Delaney L et al (2022) Monkeypox in a traveler returning from Nigeria—Dallas, Texas, July 2021. MMWR Morb Mortal Wkly Rep 71(14):509–516. https://doi.org/10.1585/mmwr.mm7114a1
CDC, US Department of Health, and Human Services (2006) Principles of epidemiology in public health practice: an introduction to applied epidemiology and biostatistics, Atlanta, GA: U.S. Department of health and human services, centers for disease control and prevention. https://stacks.cdc.gov/view/cdc/6914. Accessed 17 June 2023
Kandula S, Yamana T, Pei S, Yang W, Morita H, Shaman J (2018) Evaluation of mechanistic and statistical methods in forecasting influenza-like illness. J R Soc Interface 15(144):20180174. https://doi.org/10.1098/rsif.2018.0174
Ren H, Li J, Yuan ZA, Hu JY, Yu Y, Lu YH (2013) The development of a combined mathematical model to forecast the incidence of hepatitis E in Shanghai China. BMC Infect Dis 13(1):421. https://doi.org/10.1186/1471-2334-13-421
Zhang X, Liu Y, Yang M, Zhang T, Young AA, Li X (2013) Comparative study of four time series methods in forecasting typhoid fever incidence in China. PLoS ONE 8(5):e63116. https://doi.org/10.1371/journal.pone.0063116
Thomson MC, Molesworth AM, Djingarey MH, Yameogo KR, Belanger F, Cuevas LE (2006) Potential of environmental models to predict meningitis epidemics in Africa. Tropical Med Int Health 11(6):781–788. https://doi.org/10.1111/j.1365-3156.2006.01630.x
Orbann C, Sattenspiel L, Miller E, Dimka J (2017) Defining epidemics in computer simulation models: how do definitions influence conclusions? Epidemics 19:24–32. https://doi.org/10.1016/j.epidem.2016.12.001
Kurbalija V, Radovanović M, Ivanović M, Schmidt D, Von Trzebiatowski GL, Burkhard HD, Hinrichs C (2014) Time-series analysis in the medical domain: a study of Tacrolimus administration and influence on kidney graft function. Comput Biol Med 50:19–31. https://doi.org/10.1016/j.compbiomed.2014.04.007
Bernal JL, Cummins S, Gasparrini A (2017) Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 46(1):348–355. https://doi.org/10.1093/ije/dyw098
Bernal JL, Soumerai S, Gasparrini A (2018) A methodological framework for model selection in interrupted time series studies. J Clin Epidemiol 103:82–91. https://doi.org/10.1016/j.jclinepi.2018.05.026
Polwiang S (2020) The time series seasonal patterns of dengue fever and associated weather variables in Bangkok (2003–2017). BMC Infect Dis 20(1):208. https://doi.org/10.1186/s12879-020-4902-6
Gaudart J, Touré O, Dessay N, Dicko AL, Ranque S, Forest L, Demongeot J, Doumbo OK (2009) Modelling malaria incidence with environmental dependency in a locality of Sudanese savannah area. Mali Malaria J 8:61. https://doi.org/10.1186/1475-2875-8-61
Wei W, Jiang J, Liang H, Gao L, Liang B, Huang J, Zang N, Liao Y, Yu J, Lai J, Qin F, Su J, Ye L, Chen H (2016) Application of a combined model with autoregressive integrated moving average (ARIMA) and generalized regression neural network (GRNN) in forecasting hepatitis incidence in heng county. China PloS One 11(6):e0156768. https://doi.org/10.1371/journal.pone.0156768
Zheng YL, Zhang LP, Zhang XL, Wang K, Zheng YJ (2015) Forecast model analysis for the morbidity of tuberculosis in Xinjiang. China PloS One 10(3):e0116832. https://doi.org/10.1371/journal.pone.0116832
He Z, Tao H (2018) Epidemiology and ARIMA model of positive-rate of influenza viruses among children in Wuhan, China: a nine-year retrospective study. Int J Infect Dis: Off Publ Int Soc Infect Dis 74:61–70. https://doi.org/10.1016/j.ijid.2018.07.003
ArunKumar KE, Kalaga DV, Kumar CMS, Kawaji M, Brenza TM (2022) Comparative analysis of gated recurrent units (GRU), long short-term memory (LSTM) cells, autoregressive Integrated moving average (ARIMA), seasonal autoregressive Integrated moving average (SARIMA) for forecasting COVID-19 trends. Alex Eng J 61(10):7585–7603. https://doi.org/10.1016/j.aej.2022.01.011
Prasad VK, Bhattacharya P, Bhavsar M, Verma A, Tanwar S, Sharma G, Bokoro PN, Sharma R (2022) ABV-CoViD: an ensemble forecasting model to predict availability of beds and ventilators for COVID-19 like pandemics. IEEE Access 10:74131–74151. https://doi.org/10.1109/ACCESS.2022.3190497
Cassels S, Clark SJ, Morris M (2008) Mathematical models for HIV transmission dynamics: tools for social and behavioral science research. J Acquir Immune Defic Syndr 47(Suppl 1):S34-39. https://doi.org/10.1097/QAI.0b013e3181605da3
Mondal J, Khajanchi S, Samui P (2022) Impact of media awareness in mitigating the spread of an infectious disease with application to optimal control. Eur Phys J Plus 137(8):983. https://doi.org/10.1140/epjp/s13360-022-03156-x
Bera S, Khajanchi S, Roy TK (2023) Stability analysis of fuzzy HTLV-I infection model: a dynamic approach. J Appl Math Comput 69(1):171–199. https://doi.org/10.1007/s12190-022-01741-y
Andraud M, Hens N, Marais C, Beutels P (2012) Dynamic epidemiological models for dengue transmission: a systematic review of structural approaches. PLoS ONE 7(11):e49085. https://doi.org/10.1371/journal.pone.0049085
Huppert A, Katriel G (2013) Mathematical modelling and prediction in infectious disease epidemiology. Clin Microbiol Infect 19(11):999–1005. https://doi.org/10.1111/1469-0691.12308
Xia ZQ, Wang SF, Li SL, Huang LY, Zhang WY, Sun GQ, Gai ZT, Jin Z (2015) Modeling the transmission dynamics of Ebola virus disease in Liberia. Sci Rep 5:13857. https://doi.org/10.1038/srep13857
Drake JM, Bakach I, Just MR, O’Regan SM, Gambhir M, Fung ICH (2015) Transmission models of historical ebola outbreaks. Emerg Infect Dis 21(8):1447–1450. https://doi.org/10.3201/eid2108.141613
Atinuke B, Bagbe AS (2019) Statistical analysis of ebola virus disease outbreak in some West Africa Countries using S-I-R model. Ann Biostat Biometric Appl. https://doi.org/10.33552/ABBA.2019.02.000540
Hayman DTS, Sam John R, Rohani P (2022) Transmission models indicate Ebola virus persistence in non-human primate populations is unlikely. J R Soc Interface 19(187):20210638. https://doi.org/10.1098/rsif.2021.0638
Driessche PVD (2017) Reproduction numbers of infectious disease models. Infect Dis Model 2(3):288–303. https://doi.org/10.1016/j.idm.2017.06.002
Dwivedi A, Keval R, Khajanchi S (2022) Modeling optimal vaccination strategy for dengue epidemic model: a case study of India. Phys Scr 97(8):085214. https://doi.org/10.1088/1402-4896/ac807b
Li YW, Peng B, Zhou R, Zhan C, Liu YZ et al (2020) Mathematical modeling and epidemic prediction of COVID-19 and its significance to epidemic prevention and control measures. Ann Infect Dis Epidemiol 5(1):1052
Moein S, Nickaeen N, Roointan A, Borhani N, Heidary Z, Javanmard SH, Ghaisari J, Gheisari Y (2021) Inefficiency of SIR models in forecasting COVID-19 epidemic: a case study of Isfahan. Sci Rep 11(1):4725. https://doi.org/10.1038/s41598-021-84055-6
Yang Q, Yi C, Vajdi A, Cohnstaedt LW, Wu H, Guo X, Scoglio CM (2020) Short-term forecasts and long-term mitigation evaluations for the COVID-19 epidemic in Hubei Province, China. Infect Dis Model 5:563–574. https://doi.org/10.1016/j.idm.2020.08.001
Alvarez MM, González-González E, Trujillo-de Santiago G (2021) Modeling COVID-19 epidemics in an excel spreadsheet to enable first-hand accurate predictions of the pandemic evolution in urban areas. Sci Rep 11(1):4327. https://doi.org/10.1038/s41598-021-83697-w
Wang J, Liu Y, Liu X, Shen K (2022) A modified SIR model for the COVID-19 epidemic in China. J Phys: Conf Ser 2148(1):012002. https://doi.org/10.1088/1742-6596/2148/1/012002
Bartholomew D (1971) Time series analysis forecasting and control, vol 22. Wiley, Hoboke, pp 199–201
Priebe S, Huxley P, Knight S, Evans S (1999) Application and results of the manchester short assessment of quality of life (MANSA). Int J Soc Psychiatry 45(1):7–12. https://doi.org/10.1177/002076409904500102
Qureshi M, Khan S, Bantan RAR, Daniyal M, Elgarhy M, Marzo RR, Lin Y (2022) Modeling and forecasting monkeypox cases using stochastic models. J Clin Med 11(21):6555. https://doi.org/10.3390/jcm11216555
Acknowledgements
We are thankful to Babasaheb Bhimrao Ambedkar University for providing us with the basic research infrastructure, which helped us in carrying out this work.
Funding
This work is supported by the Council of Scientific and Technology Research- Uttar Pradesh, Government of Uttar Pradesh, through Project No. CST/D-1310.
Author information
Authors and Affiliations
Contributions
SKY and YA: conceived the idea. SAK and VS: retrieved the data and performed the analysis. SKY: wrote the first draft. SKY and YA: edited the final version and coordinated the overall study.
Corresponding authors
Ethics declarations
Conflict of interest
We do not have any conflict of interest to report.
Ethical Approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, V., Khan, S.A., Yadav, S.K. et al. Modeling Global Monkeypox Infection Spread Data: A Comparative Study of Time Series Regression and Machine Learning Models. Curr Microbiol 81, 15 (2024). https://doi.org/10.1007/s00284-023-03531-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00284-023-03531-6