Abstract
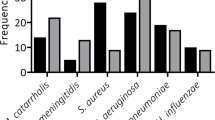
The spreading of multidrug resistance (MDR) strains in the hospital settings via contaminated surfaces have been increasingly reported where Gram-negative bacteria have been implicated in causing most nosocomial infections. This study aimed to determine the rate of contamination with multi-resistant gram-negative bacteria in the hospital environment. A cross-sectional study was conducted at Muhimbili National Hospital paediatric department, between July and August 2020. Non-repetitive surface swab samples were collected from predefined surfaces and medical device surfaces, and cultured on MacConkey agar with and without antibiotics. Isolates were identified using biochemical test and tested for antibiotic susceptibility using the Kirby-Bauer disk diffusion method. The rate of hospital contamination with Gram-negative bacteria across the Pediatrics units was 30%, with a high rate observed in oncology units (34.8%) and the malnutrition/diarrhoea ward (32.1%). Sink/washing basin had the highest frequency of bacterial contamination (74.2%). We observed a high rate of ESBL (32.5%), with Acinetobacter baumannii, Klebsiella pneumoniae, and E. coli being the predominant ESBL-producing Gram-negative bacteria, while carbapenemase-producing Gram-negative bacteria was detected at 22.8%. Highest resistance rates (63–100%) were observed against ceftriaxone and trimethoprim-sulfamethoxazole. Up to 51% of the Gram-negative bacteria showed resistant to meropenem. MDR strains were detected in 61.4% of Gram-negative bacteria isolated. In conclusion, we observed a high rate of MDR bacteria contaminating hospital surfaces. The higher rate of MDR calls for a need to strengthen infectious prevention control measures, including cleaning practices in the hospital environment, to reduce the risk of transmission of resistant strains to patients and healthcare workers.

Similar content being viewed by others
Data Availability
All data generated or analysed during this study are included in this published article.
Code Availability
Not applicable.
Abbreviations
- ATCC:
-
American Type Culture Collection
- AMZ:
-
Aztreonam
- CLSI:
-
Clinical and Laboratory Standards Institute
- CN:
-
Gentamicin
- CRO:
-
Ceftriaxone
- CIP:
-
Ciprofloxacin
- CI:
-
Confidence interval
- ESBL:
-
Extended-spectrum beta-lactamase
- IPC:
-
Infectious prevention and control
- MEM:
-
Meropenem
- mCIM:
-
Modified Carbapenem Inactivation Method
- MNH:
-
Muhimbili National Hospital
- MUHAS:
-
Muhimbili University of Health and Allied Sciences
- MDR:
-
Multidrug resistance
- NA:
-
Not applicable
- PICU:
-
Intensive care unit
- PRT:
-
Piperacillin-tazobactam
- R3–R6:
-
Resistant to 3, 4, 5, or 6 classes of antimicrobials
- SPSS:
-
Statistical Packages for Social Sciences
- SXT:
-
Trimethoprim-sulfamethoxazole
- WHO:
-
World Health Organization
References
Ayukekbong JA, Ntemgwa M, Atabe AN (2017) The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control 6:47. https://doi.org/10.1186/s13756-017-0208-x
World Health Organization. WHO publishes list of bacteria for which new antibiotics are urgently needed; (2017). Available from: http://www.who.int/mediacentre/news/releases/2017/bacteria‑antibiotics‑needed/en/. (Last accessed on 2022 July 26)
Ruppé E, Woerther P, Barbier F (2015) Mechanisms of antimicrobial resistance in Gram-negative bacilli. Ann Intensive Care 5:21. https://doi.org/10.1186/s13613-015-0061-0
Haque M, Sartelli M, McKimm J, Abu Bakar M (2018) Health care-associated infections – an overview. Infection and drug resistance. Infect Drug Resist 11:2321–2333. https://doi.org/10.2147/IDR.S177247
Siegel JD, Grossman L (2008) Pediatric infection prevention and control. Princ Pract Pediatr Infect Dis. https://doi.org/10.1016/B978-0-7020-3468-8.50008-0
Chemaly RF, Simmons S, Dale C Jr, Ghantoji SS, Rodriguez M, Gubb J, Stachowiak J, Mark Stibich M (2014) The role of the healthcare environment in the spread of multidrug-resistant organisms: update on current best practices for containment. Ther Adv Infect Dis 2(3–4):79–90. https://doi.org/10.1177/2049936114543287
Chia PY, Sengupta S, Kukreja A, Ponnampalavanar SL, Tek Ng O, Marimuthu K (2020) The role of hospital environment in transmissions of multidrug-resistant gram-negative organisms. Antimicrob Resist Infect Control 9:29. https://doi.org/10.1186/s13756-020-0685-1
Manoukian S, Stewart S, Dancer S, Graves N, Mason H, McFarland A (2018) Estimating excess length of stay due to healthcare associated infections: a systematic review and meta-analysis of statistical methodology. J Hosp Infect 100(2):222–235. https://doi.org/10.1016/j.jhin.2018.06.003
Kramer A, Schwebke I, Kampf G (2006) How long do nosocomial pathogens persist on inanimate surfaces? a systematic review. BMC Infect Dis 6:130. https://doi.org/10.1186/1471-2334-6-130
Carling PC, Parry MF, Bruno-Murtha L, Dick B (2010) Improving environmental hygiene in 27 intensive care units to decrease multidrug-resistant bacterial transmission. Crit Care Med 38(4):1054–1059. https://doi.org/10.1097/CCM.0b013e3181cdf705
Mcdonnell G, Russell AD (1999) Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev 12(1):147–179. https://doi.org/10.1128/cmr.12.1.147
Chen KH, Chen LR, Wang YK (2014) Contamination of medical charts: an important source of potential infection in hospitals. PLoS One 9(2):e78512. https://doi.org/10.1371/journal.pone.0078512
Morgan DJ, Rogawski E, Thom KA, Kristie Johnson J, Perencevich EN, Shardell M, Leekha S, Harris AD (2012) Transfer of multidrug-resistant bacteria to healthcare workers’ gloves and gowns after patient contact increases with environmental contamination. Crit Care Med 40(4):1045–1051. https://doi.org/10.1097/CCM.0b013e31823bc7c8
Getachew H, Derbie A, Mekonnen D (2018) Surfaces and air bacteriology of selected wards at a referral hospital, Northwest Ethiopia: a cross-sectional study. Int J Microbiol ID6413179:7. https://doi.org/10.1155/2018/6413179
Tajeddin E, Rashidan M, Razaghi M, Javadi SSS, Sherafat SJ, Alebouyeh M, Sarbazi RM, Mansouri N, Zali MR (2016) The role of the intensive care unit environment and healthcare workers in the transmission of bacteria associated with hospital acquired infections. J Infect Public Health 9(1):13–23. https://doi.org/10.1016/j.jiph.2015.05.010
Chaoui L, Mhand R, Mellouki F, Rhallabi N (2019) Contamination of the surfaces of a health care environment by multidrug-resistant (MDR) bacteria. Int J Microbiol ID3236526:7. https://doi.org/10.1155/2019/3236526
Moremi N, Claus H, Silago V, Kabage P, Abednego R, Matee M, Vogel U, Mshana SE (2019) Hospital surface contamination with antimicrobial-resistant Gram-negative organisms in Tanzanian regional and tertiary hospitals: the need to improve environmental cleaning. J Hosp Infect 102:98–100. https://doi.org/10.1016/j.jhin.2018.09.001
Silago V, Mruma EC, Msemwa B, Mtemisika CI, Phillip S, Ndagula RA, Said MM, Martha MF, Mshana SE (2022) Predominance of Acinetobacter spp, harboring the blaIMP gene, contaminating the hospital environment in a tertiary hospital in Mwanza, Tanzania: a cross-sectional laboratory-based study. Pathogens 11(1):63. https://doi.org/10.3390/pathogens11010063
Manyahi J, Majigo M, Kibwana U, Kamori D, Lyamuya EF (2022) Colonization of extended-spectrum beta-lactamase producing Enterobacterales and meticillin-resistant S. aureus in the intensive care unit at a tertiary hospital in Tanzania: implications for infection control and prevention. Infect Prev Pract 4(2):100212. https://doi.org/10.1016/j.infpip.2022.100212
Manyahi J, Kibwana U, Mgimba E, Majigo M (2020) Multidrug resistant bacteria predict mortality in bloodstream infection in a tertiary setting in Tanzania. PLoS One 15(3):e0220424. https://doi.org/10.1371/journal.pone.0220424
Clinical and laboratory standard institute (2019). Performance standards for antimicrobial susceptibility testing; twenty-eighth informational supplement CLSI Document M100–S20. Wayne, PA: Clinical and Laboratory Standards Institute. https://infostore.saiglobal.com/en-us/Standards/CLSI-M100-S20-20ED-2010-357589_SAIG_CLSI_CLSI_814507/
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter G, Olsson-Liljequist B, Paterson DL, Rice LB, Stelling J, Struelens MJ, Vatopoulos A, Weber JT, Monnet DL (2012) Multidrugresistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18(3):268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Barnes SL, Morgan DJ, Harris AD, Carling PC, Thom KA (2014) Preventing the transmission of multidrug-resistant organisms:modeling the relative importance of hand hygiene and environmental cleaning interventions. Infect Control Hosp Epidemiol 35(9):1156–1162. https://doi.org/10.1086/677632
Shams AM, Rose LJ, Edwards JR, Cali S, Harris AD, Jacob JT, LaFae A, Pineles LL, Thom KA, McDonald LC, Arduino MJ, Noble-Wang JA (2016) Assessment of the overall and multidrug-resistant organism bioburden on environmental surfaces in healthcare facilities. Infect Control Hosp Epidemiol 37(12):1426–1432. https://doi.org/10.1017/ice.2016.198
Kizny Gordon AE, Mathers AJ, Cheong EYL, Gottlieb T, Kotay S, Walker AS, Peto TEA, Crook DW, Stoesser N (2017) The hospital water environment as a reservoir for carbapenem-resistant organisms causing hospital-acquired infections-a systematic review of the literature. Clin Infect Dis 64(10):1435–1444. https://doi.org/10.1093/cid/cix132
Aranega-Bou P, George RP, Verlander NQ, Paton S, Bennett A, Moore G, TRACE Investigators’ Group (2019) Carbapenem-resistant Enterobacteriaceae dispersal from sinks is linked to drain position and drainage rates in a laboratory model system. J Hosp Infect. 102(1):63–69. https://doi.org/10.1016/j.jhin.2018.12.007
Hota S, Hirji Z, Stockton K, Lemieux C, Dedier H, Wolfaardt G, Gardam MA (2009) Outbreak of multidrug-resistant Pseudomonas aeruginosa colonization and infection secondary to imperfect intensive care unit room design. Infect Control Hosp Epidemiol 30(1):25–33. https://doi.org/10.1086/592700
Suleyman G, Alangaden G, Bardossy AC (2018) The role of environmental contamination in the transmission of nosocomial pathogens and healthcare-associated infections. Curr Infect Dis Rep 20:12. https://doi.org/10.1007/s11908-018-0620-2
Worku T, Derseh D, Kumalo A (2018) Bacterial profile and antimicrobial susceptibility pattern of the isolates from stethoscope, thermometer, and inanimate surfaces of Mizan-Tepi University Teaching Hospital, Southwest Ethiopia. Int J Microbiol. https://doi.org/10.1155/2018/9824251
Leylabadlo HE, Pourlak T, Zahedi bialvaei A, Aghazadeh M, Asgharzadeh M, Kafil HS, (2017) Extended-spectrum beta-lactamase producing Gram negative bacteria in Iran: a review. Afr J Infect Dis 11(2):39–53. https://doi.org/10.21010/ajid.v11i2.6
Otter JA, Yezli S, Salkeld JA, French GL (2013) Evidence that contaminated surfaces contribute to the transmission of hospital pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am J Infect Control 41(5):S6-11. https://doi.org/10.1016/j.ajic.2012.12.004
Acknowledgements
We would like to thank the staff at the bacteriology research laboratory at MUHAS, especially Mr. Lushona Mathias, for the technical assistance towards this work. We would also like to thank MUHAS and MNH management for allowing us to conduct this study.
Funding
This research did not receive any funding; the research was funded by authors.
Author information
Authors and Affiliations
Contributions
AJ conceived the study. AJ, HI and JL collected data and performed the laboratory investigations. AJ and MM performed analysis and interpreted the data. AJ drafted the manuscript. JM, FM and MM revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Joachim, A., Manyahi, J., Issa, H. et al. Predominance of Multidrug-Resistant Gram-Negative Bacteria on Contaminated Surfaces at a Tertiary Hospital in Tanzania: A Call to Strengthening Environmental Infection Prevention and Control Measures. Curr Microbiol 80, 148 (2023). https://doi.org/10.1007/s00284-023-03254-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00284-023-03254-8