Abstract
Intestinal microbiota disorders can aggravate pulmonary inflammation during acute lung injury (ALI). As a traditional Chinese herb, Rhubarb can regulated the gut microbiota. Therefore, this study was conducted to test the hypothesis that rhubarb alleviates gut microbiota dysbiosis and inflammation. Feces were collected from patients with ALI to detect the gut microbiota using 16S rDNA sequencing. Subsequently, a mouse model of ALI was established using lipopolysaccharide to investigate changes in the gut microbiota, the peripheral blood was attained for detecting the Th17/Treg cell ratio and the serum level of HDAC6 and HDAC9, and the effect of rhubarb treatment on the gut microbiota and Th17/Treg ratio were also evaluated. The results indicated that both the Firmicutes phylum decreased and the Bacteroidetes phylum increased were identified in patients with ALI, which induced the alternation of histone metabolites. The mice models also showed a similar imbalance in the Firmicutes/Bacteroidetes ratio at phylum of level. Rhubarb treatment alleviated the damaged lung tissue, accelerated Alistipes, Clostridium, and Lactobacillus proliferation at the level of genus, increased the level of HDAC6 in both the mice lung tissue and serum, and markedly reduced the Treg cells and increased the Th17 cells in the spleen tissue. The study suggested that both patients and mouse models with ALI presented gut microbiota dysbiosis, and lead to a Th17/Treg cell imbalance in ALI mouse. Rhubarb promoted Alistipes, Clostridium, and Lactobacillus proliferation, increased the HDAC6 concentration, restored the Th17/Treg cell balance, and protected against ALI.





Similar content being viewed by others
Data Availability
The raw materials were uploaded to the NCBI BioProject (NO: SRP357547).
Change history
30 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00284-022-02885-7
References
Gotts Jeffrey E, Matthay Michael A (2014) Treating ARDS: new hope for a tough problem. Lancet Respir Med 2(2):84–85. https://doi.org/10.1016/S2213-2600(13)70285-6
Semple JW, McVey MJ, Kim M, Rebetz J, Kuebler WM, Kapur R (2018) Targeting transfusion-related acute lung injury: the journey from basic science to novel therapies. Crit Care Med 46:e452–e458. https://doi.org/10.1097/CCM.0000000000002989
Semple JW, Rebetz J, Kapur R (2019) Transfusion-associated circulatory overload and transfusion-related acute lung injury. Blood 133:1840–1853. https://doi.org/10.1182/blood-2018-10-860809
Rebetz J, Semple JW, Kapur R (2018) The pathogenic involvement of neutrophils in acute respiratory distress syndrome and transfusion-related acute lung injury. Transfus Med Hemother 45:290–298. https://doi.org/10.1159/000492950
Kapur R, Kasetty G, Rebetz J, Egesten A, Semple JW (2019) Osteopontin mediates murine transfusion-related acute lung injury via stimulation of pulmonary neutrophil accumulation. Blood 134:74–84. https://doi.org/10.1182/blood.2019000972
Calfee CS, Eisner MD, Ware LB, Thompson BT, Parsons PE, Wheeler AP, Korpak A, Matthay MA, Acute Respiratory Distress Syndrome Network, National Heart, Lung and Blood Institue (2007) Trauma-associated lung injury differs clinically and biologically from acute lung injury due to other clinical disorders. Crit Care Med 35:2243–2250. https://doi.org/10.1097/01.CCM.0000280434.33451.87
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD (2005) Incidence and outcomes of acute lung injury. N Engl J Med 353:1685–1693. https://doi.org/10.1056/NEJMoa050333
Sommer F, Anderson JM, Bharti R, Raes J, Rosenstiel P (2017) The resilience of the intestinal microbiota influences health and disease. Nat Rev Microbiol 15:630–638. https://doi.org/10.1038/nrmicro.2017.58
Zimmermann P, Messina N, Mohn WW et al (2019) Association between the intestinal microbiota and allergic sensitization, eczema, and asthma: A systematic review. J Allergy Clin Immunol 143:467–485
Li Y, Liu XY, Ma MM, Qi ZJ, Zhang XQ, Li Z, Cao GH, Li J, Zhu WW, Wang XZ (2014) Changes in intestinal microflora in rats with acute respiratory distress syndrome. World J Gastroenterol 20:5849–5858. https://doi.org/10.3748/wjg.v20.i19.5849
Sze MA, Tsuruta M, Yang SW, Oh Y, Man SF, Hogg JC, Sin DD (2014) Changes in the bacterial microbiota in gut, blood, and lungs following acute LPS instillation into mice lungs. PLoS ONE 9:e111228. https://doi.org/10.1371/journal.pone.0111228
Kapur R, Kim M, Rebetz J, Hallström B, Björkman JT, Takabe-French A, Kim N, Liu J, Shanmugabhavananthan S, Milosevic S, McVey MJ, Speck ER, Semple JW (2018) Gastrointestinal microbiota contributes to the development of murine transfusion-related acute lung injury. Blood Adv 2(13):1651–1663. https://doi.org/10.1182/bloodadvances.2018018903
Yu ZX, Ji MS, Yan J, Cai Y, Liu J, Yang HF, Li Y, Jin ZC, Zheng JX (2015) The ratio of Th17/Treg cells as a risk indicator in early acute respiratory distress syndrome. Crit Care 19:82. https://doi.org/10.1186/s13054-015-0811-2
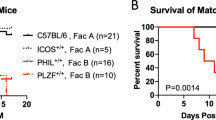
Kapur R, Kim M, Aslam R, McVey MJ, Tabuchi A, Luo A, Liu J, Li Y, Shanmugabhavananthan S, Speck ER, Zufferey A, Yousef G, Zhang H, Rondina MT, Weyrich AS, Porcelijn L, Kuebler WM, Slutsky AS, Semple JW (2017) T regulatory cells and dendritic cells protect against transfusion-related acute lung injury via IL-10. Blood 129:2557–2569. https://doi.org/10.1182/blood-2016-12-758185
Luo A, Leach ST, Barres R, Hesson LB, Grimm MC, Simar D (2017) The microbiota and epigenetic regulation of T helper 17/regulatory T cells: in search of a balanced immune system. Front Immunol 8:417. https://doi.org/10.3389/fimmu.2017.00417
Huang Z, Xu Y, Wang Q, Gao X (2019) Metabolism and mutual biotransformations of anthraquinones and anthrones in rhubarb by human intestinal flora using UPLC-Q-TOF/MS. J Chromatogr B Anal Technol Biomed Life Sci 1104:59–66. https://doi.org/10.1016/j.jchromb.2018.10.008
Wang Z, Elekwachi C, Jiao J, Wang M, Tang S, Zhou C, Tan Z, Forster RJ (2017) Changes in metabolically active bacterial community during rumen development, and their alteration by rhubarb root powder revealed by 16S rRNA amplicon sequencing. Front Microbiol 8:159. https://doi.org/10.3389/fmicb.2017.00159
Yao P, Cui M, Li Y, Deng Y, Wu H (2015) Effects of rhubarb on intestinal flora and toll-like receptors of intestinal mucosa in rats with severe acute pancreatitis. Pancreas 44:799–804. https://doi.org/10.1097/MPA.0000000000000339
Song YD, Li XZ, Wu YX, Shen Y, Liu FF, Gao PP, Sun L, Qian F (2018) Emodin alleviates alternatively activated macrophage and asthmatic airway inflammation in a muring asthma model. Acta Pharmacol Sin 39:1317–1325. https://doi.org/10.1038/aps.2017.147
Xiao M, Zhu T, Zhang W, Wang T, Shen YC, Wan QF, Wen FQ (2014) Emodin ameliorates LPS-induced acute lung injury, involving the inactivation of NF-κB in mice. Int J Mol Sci 15:19355–19368. https://doi.org/10.3390/ijms151119355
Zeng YQ, Dai Z, Lu F, Lu Z, Liu X, Chen C, Qu P, Li D, Hua Z, Qu Y, Zou C (2016) Emodin via colonic irrigation modulates gut microbiota and reduces uremic toxins in rats with chronic kidney disease. Oncotarget 7:17468–17478. https://doi.org/10.3390/ijms151119355
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS (2012) Acute respiratory distress syndrome: the Berlin definition. JAMA 307:2526–2533
Kapur R, Rebetz J, van der Velden S, Semple JW (2021) Pancreatic involvement in murine antibody-mediated transfusion-related acute lung injury? Transfusion 61:987–989. https://doi.org/10.1111/trf.16240
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly-y M, Glickman JN, Garrett WS (2013) The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostatsis. Science 341:569–573
Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, deRoos P, Liu H, Cross JR, Pfeffer K, Coffer PJ, Rudensky AY (2013) Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504:451–455. https://doi.org/10.1038/nature12726
Neyrinck AM, Etxeberria U, Taminiau B, Daube G, Van Hul M, Everard A, Cani PD, Bindels LB, Delzenne NM (2017) Rhubarb extract prevents hepatic inflammation induced by acute alcohol intake, an effect related to the modulation of the gut microbiota. Mol Nutr Food Res. https://doi.org/10.1002/mnfr.201500899
Jialing L, Yangyang G, Jing Z, Xiaoyi T, Ping W, Liwei S, Simin C (2020) Changes in serum inflammatory cytokine levels and intestinal flora in a self-healing dextran sodium sulfate-induced ulcerative colitis murine model. Life Sci 263:118587. https://doi.org/10.1016/j.lfs.2020.118587
Li YN, Huang F, Liu L, Qiao HM, Li Y, Cheng HJ (2012) Effect of oral feeding with Clostridium leptum on regulatory T-cell responses and allergic airway inflammation in mice. Ann Allergy Asthma Immunol 109:201–207. https://doi.org/10.1016/j.anai.2012.06.017
Tao R, de Zoeten EF, Ozkaynak E, Chen C, Wang L, Porrett PM, Li B, Turka LA, Olson EN, Greene MI, Wells AD, Hancock WW (2007) Deacetylase inhibtion promotes the generation and function of regulatory T cells. Nat Med 13:1299–1307. https://doi.org/10.1038/nm1652
Liu L, Zhou X, Shetty S, Hou G, Wang Q, Fu J (2019) HDAC6 inhibition blocks inflammatory signaling and caspase-1 activation in LPS-induced acute lung injury. Toxicol Appl Pharmacol 370:178–183. https://doi.org/10.1016/j.taap.2019.03.017
Menden H, Xia S, Mabry SM, Noel-MacDonnell J, Rajasingh J, Ye SQ, Sampath V (2019) Histone deacetylase 6 regulates endotheliao MyD88-dependent canonical TLR signaling, lung inflammation, and alveolar remodeling in the developing lung. Am J Physiol Lung Cell Mol Physiol 317:L332–L346. https://doi.org/10.1152/ajplung.00247.2018
Zhang F, Li MY, Lan YT, Wang CB (2016) Imbalance of Th17/Tregs in rats with smoke inhalation-induced acute lung injury. Sci Rep 6:21348. https://doi.org/10.1038/srep21348
Luo S, Wen R, Wang Q, Zhao Z, Nong F, Fu Y, Huang S, Chen J, Zhou L, Luo X (2019) Rhubarb peony decoction ameliorates ulcerative colitis in mice by regulating gut microbiota to restoring Th17/Treg balance. J Ethnopharmacol 231:39–49. https://doi.org/10.1016/j.jep.2018.08.033
Sharma R, Tiku AB (2016) Emodin inhibits splenocyte proliferation and inflammation by modulating cytokine responses in a mouse model system. J Immunotoxicol 13:20–26. https://doi.org/10.3109/1547691X.2014.995243
Acknowledgements
We thank Traci Raley, MS, ELS, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac) for editing a draft of this manuscript.
Funding
Natural Science Foundation of Zhejiang Province (LY18H290008), Natural Science Foundation of China (81973590) and the Medical and Health Science and Technology Plan of Zhejiang Province (2019KY006) provided financial support in the form of researcher funding. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
TYT drafted the manuscript, WF and YW collected the samples and analyze data, TZ contributed to perform detection and prepare tables, LZJ conceived and planned the study design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
The study was conducted according to the World Medical Association Declaration of Helsinki in 1975, as revised in 1983, and was approved by the Ethic Committee of Zhejiang Hospital (Grant NO: 2019-28 (K)).
Consent to Participate
All subjects provided their informed written consent.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tang, T., Wang, F., Liu, J. et al. Rhubarb Alleviates Acute Lung Injury by Modulating Gut Microbiota Dysbiosis in Mice. Curr Microbiol 79, 116 (2022). https://doi.org/10.1007/s00284-022-02811-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00284-022-02811-x