Abstract
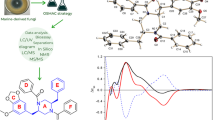
Antibiotic resistance is one of the major concerns and the biggest threats to the world population. The incidents of antibiotic resistance in Candida spp. were frequently recorded. In the present investigation, antifungal potential of ascorbic acid (AA) was evaluated. According to the in vitro analysis, the zone of inhibition of AA (24.75 ± 0.35 mm) against C. albicans was greater as compared to other vitamins tested. AA significantly modulate the growth of C. albicans at 25 mg/ml. The highest percentage (94.67%) of cell viability was observed in untreated cells, and low cell viability (29.36%) was observed in cells treated with 50 mg/ml of AA (2 × MIC). Further, AO/EB (acridine orange/ethidium bromide), propidium iodide staining, and real-time qPCR confirmed the loss of membrane integrity due to membrane lesions that caused cell death. Lanosterol 14-α-demethylase (L-14α-DM) is the product of ERG11 and acted as superior drug target of C. albicans. Molecular docking analysis confirmed that active interaction of ascorbic acid with L-14α-DM. Based on the present investigation, the efficiency of AA was effectively proved through the in vitro and in silico analysis. This finding has evidenced the effectiveness of AA as a potential candidate against C. albicans.





Similar content being viewed by others
References
Swamydas M, Break TJ, Lionakis MS (2015) Mononuclear phagocyte-mediated antifungal immunity: the role of chemotactic receptors and ligands. Cell Mol Life Sci 72(11):2157–2175
Naglik JR, Challacombe SJ, Hube B (2003) Candida albicans secreted aspartyl proteinases in virulence and pathogenesis. Microbiol Mol Biol Rev 67(3):400–428
Skrodeniene E, Dambrauskiene A, Vitkauskiene A (2006) Susceptibility of yeasts to antifungal agents in Kaunas University of Medicine Hospital. Medicina 42(4):294–299
Velayuthan R, Samudi C, Lakhbeer Singh H, Ng K, Shankar E, Denning D (2018) Estimation of the burden of serious human fungal infections in Malaysia. J Fungi 4(1):38
Alvarez-Rueda N, Fleury A, Morio F, Pagniez F, Gastinel L, Le Pape P (2011) Amino acid substitutions at the major insertion loop of Candida albicans sterol 14alpha-demethylase are involved in fluconazole resistance. PLoS ONE 6(6):e21239
Sanglard D (2016) Emerging threats in antifungal-resistant fungal pathogens. Front Med 3:11
Monk BC, Sagatova AA, Hosseini P, Ruma YN, Wilson RK, Keniya MV (2020) Fungal lanosterol 14α-demethylase: a target for next-generation antifungal design. Biochim Biophys Acta Proteins Proteomics 1868(3):140206
Parker JE, Warrilow AG, Price CL, Mullins JG, Kelly DE, Kelly SL (2014) Resistance to antifungals that target CYP51. J Chem Biol 7(4):143–161
Lee W, Lee DG (2015) Fungicidal mechanisms of the antimicrobial peptide Bac8c. Biochim Biophys Acta Biomembr 1848(2):673–679
Rad KK, Falahati M, Roudbary M, Farahyar S, Nami S (2016) Overexpression of MDR-1 and CDR-2 genes in fluconazole resistance of Candida albicans isolated from patients with vulvovaginal candidiasis. Curr Med Mycol 2(4):24
Verrax J, Calderon PB (2008) The controversial place of vitamin C in cancer treatment. Biochem Pharmacol 76(12):1644–1652
Stephensen CB, Marquis GS, Jacob RA, Kruzich LA, Douglas SD, Wilson CM (2006) Vitamins C and E in adolescents and young adults with HIV infection. Am J Clin Nutr 83(4):870–879
Wilson JX (2009) Mechanism of action of vitamin C in sepsis: ascorbate modulates redox signaling in endothelium. BioFactors 35(1):5–13
Monacelli F, Acquarone E, Giannotti C, Borghi R, Nencioni A (2017) Vitamin C, aging and Alzheimer’s disease. Nutrients 9(7):670
Srividya G, Deepthi B, Lakshminarasaiah S (2017) Ascorbic acid enhances ciprofloxacin antibacterial activity in vitro against isolates of Escherichia coli from subclinical mastitis cases of buffaloes. Int J Vet Sci Anim Husb 2(5):21–24
Krishnan A (2013) Estimation of antimicrobial activity of ascorbic acid in superoxide dismutase level in microbial culture with amino penicillin–ampicillin. Int J Pharm Sci Rev Res 20(2):167–169
Genc GE, Erdogan O, Demir C, Kisa O, Satana D (2019) In vitro antifungal activity of a medicinal plant extract mixture against candida species isolated from patients with oral stomatitis. Iran Red Crescent Med J 21(4):e87251
Ganeshkumar A, Suvaithenamudhan S, Elanthamilan E, Arun G, Dileepan GAB, Prabhusaran N, Rajaram R (2020) New insight of red seaweed derived Callophycin A as an alternative strategy to treat drug resistance vaginal candidiasis. Bioorg Chem 104:104256
Gong Y, Liu W, Huang X, Hao L, Li Y, Sun S (2019) Antifungal activity and potential mechanism of n-butylphthalide alone and in combination with fluconazole against Candida albicans. Front Microbiol. https://doi.org/10.3389/fmicb.2019.01461
Prasath KG, Tharani H, Kumar MS, Pandian SK (2020) Palmitic acid inhibits the virulence factors of Candida tropicalis: biofilms, cell surface hydrophobicity, ergosterol biosynthesis and enzymatic activity. Front Microbiol 11:864
Kwolek-Mirek M, Zadrag-Tecza R (2014) Comparison of methods used for assessing the viability and vitality of yeast cells. FEMS Yeast Res 14(7):1068–1079
Patel M, Srivastava V, Ahmad A (2020) Dodonaea viscosa var angustifolia derived 5, 6, 8-trihydroxy-7, 4′ dimethoxy flavone inhibits ergosterol synthesis and the production of hyphae and biofilm in Candida albicans. J Ethnopharmacol 259:112965
Chen L, Xu Y, Zhou C, Zhao J, Li C, Wang R (2010) Overexpression of CDR1 and CDR2 genes plays an important role in fluconazole resistance in Candida albicans with G487T and T916C mutations. J Int Med Res 38(2):536–545
Zhou Y, Liao M, Zhu C, Hu Y, Tong T, Peng X, Li M, Feng M, Cheng L, Ren B (2018) ERG3 and ERG11 genes are critical for the pathogenesis of Candida albicans during the oral mucosal infection. Int J Oral Sci 10(2):9
Harder E, Damm W, Maple J, Wu C, Reboul M, Xiang JY, Wang L, Lupyan D, Dahlgren MK, Knight JL (2015) OPLS3: a force field providing broad coverage of drug-like small molecules and proteins. J Chem Theory Comput 12(1):281–296
Wright WC, Chenge J, Wang J, Girvan HM, Yang L, Chai SC, Huber AD, Wu J, Oladimeji PO, Munro AW (2020) Clobetasol propionate is a heme-mediated selective inhibitor of human cytochrome P450 3A5. J Med Chem 63(3):1415–1433
Halgren TA (2009) Identifying and characterizing binding sites and assessing druggability. J Chem Inf Model 49(2):377–389
Halgren T (2007) New method for fast and accurate binding-site identification and analysis. Chem Biol Drug Des 69(2):146–148
Pérez-Benito L, Keränen H, van Vlijmen H, Tresadern G (2018) Predicting binding free energies of pde2 inhibitors. The difficulties of protein conformation. Sci Rep 8(1):4883
Friesner RA, Murphy RB, Repasky MP, Frye LL, Greenwood JR, Halgren TA, Sanschagrin PC, Mainz DT (2006) Extra precision Glide: Docking and scoring incorporating a model of hydrophobic enclosure for protein−ligand complexes. J Med Chem 49(21):6177–6196
Suvaithenamudhan S, Parthasarathy S (2017) Molecular dynamics simulations of novel potential inhibitors for penicillin binding protein 2B of the resistant 5204 strain of Streptococcus pneumoniae. Curr Comput Aided Drug Des 13(3):234–248
Denning DW, Bromley MJ (2015) How to bolster the antifungal pipeline. Science 347(6229):1414–1416
Perfect JR (2017) The antifungal pipeline: a reality check. Nat Rev Drug Discov 16(9):603
Levitz SM (2010) Innate recognition of fungal cell walls. PLoS Pathog 6(4):e1000758
Xing X, Liao Z, Tan F, Zhu Z, Jiang Y, Cao Y (2019) Effect of nicotinamide against Candida albicans. Front Microbiol 10:595
Sanguinetti M, Posteraro B, Lass-Flörl C (2015) Antifungal drug resistance among Candida species: mechanisms and clinical impact. Mycoses 58:2–13
Shirazi F, Kontoyiannis D (2015) Micafungin triggers caspase-dependent apoptosis in Candida albicans and Candida parapsilosis biofilms, including caspofungin non-susceptible isolates. Virulence 6(4):385–394
Ojha R, Manzoor N, Khan L (2009) Ascorbic acid modulates pathogenicity markers of Candida albicans. Int J Microbiol Res 1(1):19
Lone SA, Khan S, Ahmad A (2020) Inhibition of ergosterol synthesis in Candida albicans by novel eugenol tosylate congeners targeting sterol 14α-demethylase (CYP51) enzyme. Arch Microbiol 202(4):711–726
Douglas LM, Konopka JB (2016) Plasma membrane organization promotes virulence of the human fungal pathogen Candida albicans. J Microbiol 54(3):178–191
You Z, Zhang C, Ran Y (2020) The effects of clioquinol in morphogenesis, cell membrane and ion homeostasis in Candida albicans. BMC Microbiol 20(1):1–11
Onyewu C, Blankenship JR, Del Poeta M, Heitman J (2003) Ergosterol biosynthesis inhibitors become fungicidal when combined with calcineurin inhibitors against Candida albicans, Candida glabrata, and Candida krusei. Antimicrob Agents Chemother 47(3):956–964
Hargrove TY, Friggeri L, Wawrzak Z, Qi A, Hoekstra WJ, Schotzinger RJ, York JD, Guengerich FP, Lepesheva GI (2017) Structural analyses of Candida albicans sterol 14α-demethylase complexed with azole drugs address the molecular basis of azole-mediated inhibition of fungal sterol biosynthesis. J Biol Chem 292(16):6728–6743
Wang Y, Jia XM, Jia JH, Li MB, Cao YY, Gao PH, Liao WQ, Cao YB, Jiang YY (2009) Ascorbic acid decreases the antifungal effect of fluconazole in the treatment of candidiasis. Clin Exp Pharmacol Physiol 36(10):e40–e46
Marik PE, Khangoora V, Rivera R, Hooper MH, Catravas J (2017) Hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock: a retrospective before–after study. Chest 151(6):1229–1238
Mei H, Tu H (2018) Vitamin C and Helicobacter pylori infection: current knowledge and future prospects. Front Physiol 9:1103
Zabet MH, Mohammadi M, Ramezani M, Khalili H (2016) Effect of high-dose Ascorbic acid on vasopressor’s requirement in septic shock. J Res Pharm Pract 5(2):94
Acknowledgements
All the authors are thankful to Professor S. Parthasarathy for the guidance and critical comments on the study. Molecular dynamics studies were performed using High Performance Computing (HPC) Facility [DST-PURSE (Grant No. SR/FT/LS-113/2009)] at University Informatics Centre, Bharathidasan University, Tiruchirappalli. They would like to thank Dr. Aananth, Sivan Bioscience for his valuable comments on language of the manuscript. They show their gratitude to Editor and reviewers of this manuscript for their valuable suggestion toward the improvement of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ganeshkumar, A., Suvaithenamudhan, S. & Rajaram, R. In Vitro and In Silico Analysis of Ascorbic Acid Towards Lanosterol 14-α-Demethylase Enzyme of Fluconazole-Resistant Candida albicans. Curr Microbiol 78, 292–302 (2021). https://doi.org/10.1007/s00284-020-02269-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-020-02269-9