Abstract
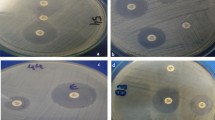
The prevalence of carbapenem resistance among bacterial isolates from selected water bodies receiving hospital effluents and adjoining aquaculture farms in Kerala, India, was studied. Klebsiella pneumoniae followed by Escherichia coli, Klebsiella oxytoca, Enterobacter aerogenes and Acinetobacter baumannii were the predominant isolates. Antibiotic sensitivity of these isolates was determined by Kirby–Bauer disc diffusion method. Nearly 60% of the Enterobacteriaceae isolates screened were multidrug resistant of which 16.6% were carbapenem resistant. The carbapenem-resistant Enterobacteriaceae were further screened for the presence of New Delhi metallo β-lactamase-1 and cephalosporin resistance encoding genes. All NDM-1 isolates were highly resistant to carbapenem, cephalosporin, aminoglycosides, quinolones, tetracycline, and sulphonamides. K. pneumoniae harboring blaNDM-1 gene and E. coli isolates with blaCTX-M-15 and blaSHV-11 genes were detected in hospital discharge points. In aquaculture farms too, carbapenem-resistant K. pneumoniae with blaNDM-1 gene and E. coli isolates with blaCTX-M-15 were observed, although there was no use of antibiotics in these farms. However, other carbapenemase genes such as blaTEM, blaVIM, blaIMP and blaGIM were not detected in any of these isolates. The results suggest the increased prevalence of carbapenem-resistant Enterobacteriaceae in the water bodies receiving hospital effluent and its dissemination to adjacent aquaculture farms, posing a serious threat to public health.


Similar content being viewed by others
References
Cahill N, Connor LO, Mahon B, Varley A, McGrath E, Ryan P, Cormican M, Brehony C, Jolley KA, Maiden MC, Brisse S, Morris D (2019) Hospital effluent: a reservoir for carbapenemase-producing Enterobacterales? Sci Total Environ 672:618–624. https://doi.org/10.1016/j.scitotenv.2019.03.428
Haller L, Chen H, Ng C, Le TH, Koh TH, Barkham T (2018) Occurrence and characteristics of extended-spectrum β-lactamase- and carbapenemase-producing bacteria from hospital effluents in Singapore. Sci Total Environ 615:1119–1125. https://doi.org/10.1016/j.scitotenv.2017.09.217
Nordmann P, Naas T, Poirel L (2011) Global spread of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis 17:1791–1798. https://doi.org/10.3201/eid1710.110655
Bush K, Jacoby GA (2010) Updated functional classification of beta-lactamases. Antimicrob Agents Chemother 54:969–976. https://doi.org/10.1128/AAC.01009-09
Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR (2009) Characterization of a new metallo-β-lactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother 53:5046–5054. https://doi.org/10.1128/AAC.00774-09
Chen Y, Zhou Z, Jiang Y, Yu Y (2011) Emergence of NDM-1 producing Acinetobacter baumannii in China. J Antimicrob Chemother 66:1255–1259. https://doi.org/10.1093/jac/dkr082
Piotrowska M, Kowalska S, Popowska M (2019) Diversity of β-lactam resistance genes in gram-negative rods isolated from a municipal wastewater treatment plant. Ann Microbiol 69:591–601. https://doi.org/10.1007/s13213-019-01450-1
Naas T, Poirel L, Nordmann P (2008) Minor extended-spectrum β-lactamase. Clin Microbiol Infect 14:42–52. https://doi.org/10.1111/j.1469-0691.2007.01861.x
Korzeniewska E, Harnisz M (2013) Beta-lactamase-producing Enterobacteriaceae in hospital effluents. J Environ Manag 123:1–7. https://doi.org/10.1016/j.jenvman.2013.03.024
Bradford PA (2001) Extended-spectrum β-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 14:933–951. https://doi.org/10.1128/CMR.14.4.933-951.2001
Bush K (2018) Past and present perspectives on β-lactamases. Antimicrob Agents Chemother 62:e01076–e1118. https://doi.org/10.1128/AAC.01076-18
Diwan V, Chandran SP, Tamhankar AJ, Lundborg CS, Macaden R (2012) Identification of extended-spectrum β-lactamase and quinolone resistance genes in Escherichia coli isolated from hospital wastewater from Central India. J Antimicrob Chemother 67:857–859. https://doi.org/10.1093/jac/dkr564
Hirsch R, Ternes T, Haberer K, Kratz KL (1999) Occurrence of antibiotics in the aquatic environment. Sci Total Environ 225:109–118. https://doi.org/10.1016/S0048-9697(98)00337-4
Walsh TR, Weeks J, Livermore DM, Toleman MA (2011) Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: an environmental point prevalence study. Lancet Infect Dis 11:355–362. https://doi.org/10.1016/S1473-3099(11)70059-7
Holt JG, Krieg NR, Sneath PHA, Staley JT, Williams ST (1994) Bergey’s manual of determinative bacteriology, 9th edn. Lippincott Williams and Wilkins, Baltimore
Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH (2003) Manual of clinical microbiology, 8th edn. American Society for Microbiiology Press, Washington, DC
Bauer AW, Kirby WM, Sherris JC, Turck M (1966) Antibiotic susceptibility testing by standardized single disc method. Am J Clin Pathol 44:493–496
Clinical and Laboratory Standards Institute (2013) Performance standards for antimicrobial susceptibility testing; twenty-third informational supplement. Document M100-S23. Clinical and Laboratory Standards Institute, Wayne
Pasteran F, Mendez T, Guerriero L, Rapoport M, Corso A (2009) Sensitive screening tests for suspected class A carbapenemase production in species of Enterobacteriaceae. J Clin Microbiol 47:1631–1639. https://doi.org/10.1128/JCM.00130-09
Kostylev M, Otwell AE, Ruth E, Richardson RE, Suzuki Y (2015) Cloning should be simple: Escherichia coli DH5α-mediated assembly of multiple DNA fragments with short end homologies. PLoS ONE 10:1–15. https://doi.org/10.1371/journal.pone.0137466
Villegas MV, Correa A, Perez F, Zuluaga T, Radice M, Gutkind G, Casellas JM, Ayala J, Lolans K, Quinn JP, Colombian Nosocomial Resistance Study Group (2004) CTX-M-12 β-Lactamase in a Klebsiella pneumoniae clinical isolate in Colombia. Antimicrob Agents Chemother 48:629–631. https://doi.org/10.1128/aac.48.2.629-631.2004
Hujer KM, Hujer AM, Hulten EA, Bajaksouzian S, Adams JM, Donskey CJ, Ecker DJ, Massire C, Eshoo MW, Sampath R, Thomson JM, Rather PN, Craft DW, Fishbain JT, Ewell AJ, Jacobs MR, Paterson DL, Bonomo RA (2006) Analysis of antibiotic resistance genes in multidrug-resistant Acinetobacter sp. isolates from military and civilian patients treated at the Walter Reed Army Medical Center. Antimicrob Agents Chemother 50:4114–4123. https://doi.org/10.1128/AAC.00778-06
Deshpande P, Rodrigues C, Shetty A, Kapadia F, Hedge A, Soman R (2010) New Delhi Metallo-beta lactamase (NDM-1) in Enterobacteriaceae: treatment options with carbapenems compromised. J Assoc Physicians India 58:147–149
Sharma J, Sharma M, Ray P (2010) Detection of TEM & SHV genes in Escherichia coli & Klebsiella pneumoniae isolates in a tertiary care hospital from India. Indian J Med Res 132:332–336
Bharti MN, Sharma PC (2016) Molecular characterization of Pseudomonas aeruginosa isolates recovered from human patients in Himachal Pradesh (India) for selective genes: extended spectrum β-lactamase (ESBL), ampicillin class C (AmpC) and metallo β-lactamase (MBL) genes. Int J Pharm Sci Res 7:4905–4916
Manyi-Loh C, Mamphweli S, Meyer E, Okoh A (2018) Antibiotic use in agriculture and its consequential resistance in environmental sources: potential public health implications. Molecules 23:1–48. https://doi.org/10.3390/molecules23040795
Diwan V, Tamhankar AJ, Khandal RK, Sen S, Aggarwal M, Marothi Y, Iyer RV, Sundblad-Tonderski K, Stalsby-Lundborg C (2010) Antibiotics and antibiotic-resistant bacteria in waters associated with a hospital in Ujjain. India. BMC Public Health 10:414
Watkinson AJ, Murky EJ, Colin DW, Costanzia SD (2009) The occurrence of antibiotics in an urban watershed: from wastewater to drinking water. Sci Total Environ 1:2711–2723. https://doi.org/10.1016/j.scitotenv.2008.11.059
Hsu LY, Tan TY, Tam VH, Kwa A, Fisher DA, Koh TH (2010) Surveillance and correlation of antibiotic prescription and resistance of gram-negative bacteria in Singaporean hospitals. Antimicrob Agents Chemother 54:1173–1178. https://doi.org/10.1128/AAC.01076-09
Baroud M, Dandache I, Araj GF, Wakim R, Kanji S, Kanafani Z, Khairallah M, Sabra A, Shehab M, Dbaibo G, Matar GM (2013) Underlying mechanisms of carbapenem resistance in extended-spectrum β-lactamase-producing Klebsiella pneumoniae and Escherichia coli isolates at a tertiary care centre in Lebanon: role of OXA-48 and NDM-1 carbapenemases. Int J Antimicrob Agents 41:75–79. https://doi.org/10.1016/j.ijantimicag.2012.08.010
Garcia-Fernandez A, Miriagou V, Papagiannitsis GA, Venditti M, Mancini C, Carattoli A (2010) An ertapenem-resistant extended-spectrum-β-lactamase-producing Klebsiella pneumoniae clone carries a novel OmpK36 porin variant. Antimicrob Agents Chemother 54:4178–4184. https://doi.org/10.1128/AAC.01301-09
Le TH, Charmaine NG, Chen H, Yi XZ, Koh TH, Barkham TMS, Zhou Z, Gina KY-H (2016) Occurrence and characterization antibiotic-resistant bacteria and genetic determinants of hospital wastewater in a tropical country. Antimicrob Agents Chemother 60:7449–7456. https://doi.org/10.1128/AAC.01556-16
Picao RC, Cardoso JP, Campana EH, Nicoletti AG, Petrolini FV, Assis DM, Juliano L, Gales AC (2013) The route of antimicrobial resistance from the hospital effluent to the environment: focus on the occurrence of KPC producing Aeromonas spp. and Enterobacteriaceae in sewage. Diagn Microbiol Infect Dis 76:80–85. https://doi.org/10.1016/j.diagmicrobio.2013.02.001
Stuart CJ, Leverstein-Van Hall MA (2010) Guidelines for the phenotypic screening and the confirmation of carbapenemases in Enterobacteriaceae. Int J Antimicrob Agents 36:205–210. https://doi.org/10.1016/j.ijantimicag.2010.05.014
Gniadkowski M (2001) Evolution and epidemiology of extended-spectrum beta lactamases (ESBLs) and ESBL-producing microorganisms. Clin Microbiol Infect 7:597–608. https://doi.org/10.1046/j.1198-743x.2001.00330.x
Fomda BA, Khan A, Zahoor D (2014) NDM-1 (New Delhi metallo beta lactamase-1) producing Gram-negative bacilli: emergence & clinical implications. Indian J Med Res 140:672–678
Assem M, Wifi-Muhamed-Naguib A, Elsherif R, Saad A, Ismail DK, Hasanin A, Bassyouni R, Gomaa MSH (2017) Emergence of gram-negative bacilli with concomitant blaNDM-1 and blaOXA-48-like genes in Egypt. Am J Intern Med 5:1–6
Rolain JM, Parola P, Cornaglia G (2010) New Delhi metallo-beta-lactamase (NDM-1) towards a new pandemia? Clin Microbiol Infect 16:1699–1701. https://doi.org/10.1111/j.1469-0691.2010.03385.x
Poirel L, Ros A, Carricajo A, Berthelot P, Pozzetto B, Bernabeu S, Nordmann P (2011) Extremely drug-resistant Citrobacter freundii isolate producing NDM-1 and other carbapenemases identified in a patient returning from India. Antimicrob Agents Chemother 55:447–448. https://doi.org/10.1128/AAC.01305-10
Bharadwaj R, Joshi S, Dohe V, Gaikwad V, Kulkarni G, Shouche Y (2012) Prevalence of New Delhi metallo-beta-lactamase (NDM-1)-positive bacteria in a tertiary care centre in Pune, India. Int J Antimicrob Agents 39:265–266. https://doi.org/10.1016/j.ijantimicag.2011.09.027
Kumarasamy K, Kalyanasundaram A (2012) Emergence of Klebsiella pneumonoae isolate co-producing NDM-1 with KPC-2 from India. J Antimicrob Chemother 67:243–244. https://doi.org/10.1093/jac/dkr431
D’Andrea MM, Arena F, Pallecchi L, Rossolini GM (2013) CTX-M-type beta-lactamases: a successful story of antibiotic resistance. Int J Med Microbiol 303:305–317. https://doi.org/10.1016/j.ijmm.2013.02.008
Canton R, González-Alba JM, Galán JC (2012) CTX-M enzymes: origin and diffusion. Front Microbiol 3:1–19. https://doi.org/10.3389/fmicb.2012.00110
Ibrahimagic A, Bedenic B, Kamberovic F, Uzunovic S (2015) High prevalence of CTX-M-15 and first report of CTX-M-3, CTX-M-22, CTX-M-28 and plasmid mediated AmpC beta-lactamase producing Enterobacteriaceae causing urinary tract infections in Bosnia and Herzegovina in hospital and community settings. J Infect Chemother 21:363–369. https://doi.org/10.1016/j.jiac.2015.01.003
Khan FA, Hellmark B, Ehricht R, Soderquist B, Jass J (2018) Related carbapenemase-producing Klebsiella isolates detected in both a hospital and associated aquatic environment in Swedan. Eur J Clin Microbiol Infect Dis 37:2241–2251. https://doi.org/10.1007/s10096-018-3365-9
Limansky AS, Mussi MA, Viale AM (2002) Loss of a 29-kilodalton outer membrane protein in Acinetobacter baumannii is associated with imipenem resistance. J Clin Microbiol 40:4776–4778. https://doi.org/10.1128/JCM.40.12.4776-4778.2002
Warner DM, Yang Q, Duval V, Chen M, Xu Y, Levy SB (2013) Involvement of MarR and YedS in carbapenem resistance in a clinical isolate of Escherichia coli from China. Antimicrob Agents Chemother 57:1935–1937. https://doi.org/10.1128/AAC.02445-12
Islam MA, Islam M, Hasan R, Hossain MI, Nabi A, Rahman M, Goessens WHF, Endtz HP, Boehm AB, Faruquea SM (2017) Environmental spread of New Delhi Metallo-β-Lactamase-1-producing multidrug-resistant bacteria in Dhaka Bangladesh. Appl Environ Microbiol 83:e00793–e817. https://doi.org/10.1128/AEM.00793-17
Schluter A, Szczepanowski R, Puhler A, Top EM (2007) Genomics of IncP-1 antibiotic resistance plasmids isolated from wastewater treatment plants provides evidence for a widely accessible drug resistance gene pool. FEMS Microbiol Rev 31:449–477. https://doi.org/10.1111/j.1574-6976.2007.00074.x
Kelly BG, Vespermann A, Bolton DJ (2009) Gene transfer events and their occurrence in selected environments. Food Chem Toxicol 47:978–983. https://doi.org/10.1016/j.fct.2008.06.012
Lorenzo P, Adriana A, Jessica S, Carles B, Marinella F, Marta L, Luis BJ, Pierre S (2018) Antibiotic resistance in urban and hospital wastewaters and their impact on a receiving freshwater ecosystem. Chemosphere 206:70–82. https://doi.org/10.1016/j.chemosphere.2018.04.163
Rafraf ID, Lekunberri I, Sànchez-Melsio A, Aouni M, Borrego CM, Balcázar JL (2016) Abundance of antibiotic resistance genes in five municipal wastewater treatment plants in the Monastir Governorate, Tunisia. Environ Pollut 219:353–358. https://doi.org/10.1016/j.envpol.2016.10.062
Faleye AC, Adegoke AA, Ramluckan K, Fick J, Bux F, Stenstrom TA (2019) Concentration and reduction of antibiotic residues in selected wastewater treatment plants and receiving water bodies in Durban, South Africa. Sci Total Environ 678:10–20. https://doi.org/10.1016/j.scitotenv.2019.04.410
Wang Q, Wang P, Yang Q (2018) Occurrence and diversity of antibiotic resistance in untreated hospital wastewater. Sci Total Environ 621:990–999. https://doi.org/10.1016/j.scitotenv.2017.10.128
Barancheshme F, Munir M (2018) Strategies to combat antibiotic resistance in the wastewater treatment plants. Front Microbiol 8:1–12. https://doi.org/10.3389/fmicb.2017.02603
Larsson DGJ, Andremont A, Bengtsson-Palme J, Brandt KK, de Roda Husman AM, Fagerstedt P, Fick J, Flach CF, Gaze WH, Kuroda M, Kvint K, Laxminarayan R, Manaia CM, Nielsen KM, Plant L, Ploy MC, Segovia C, Simonet P, Smalla K, Snape J, Topp E, van Hengel AJ, Verner-Jeffreys DW, Virta MPJ, Wellington EM, Wernersson AS (2018) Critical knowledge gaps and research needs related to the environmental dimensions of antibiotic resistance. Environ Int 117:132–138. https://doi.org/10.1016/j.envint.2018.04.041
Acknowledgements
The authors wish to thank the authorities of the Kerala University of Fisheries and Ocean Studies for providing funds and facilities to carry out the work.
Author information
Authors and Affiliations
Contributions
SKG is responsible for performing the experiments and drafting the manuscript. RK assisted the first author in some of the experiments, RK helped in the editing, DP is responsible for conception and planning of the study, critical review and editing of the article. RP, PM and DP work together in the Kerala Antimicrobial Resistance Strategic Action Plan and were involved in critical review and editing of the article.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors the corresponding author states that there is no conflict of interest.
Ethical Standards
All experiments were performed in strict accordance with the guidelines of the Committee for Purpose of Control and Supervision of Experiments on Animals (CPCSEA) registration number: 1174/ac/08/CPCSEA. The protocol was reviewed and approved by the institutional animal ethics committee of Kerala University of Fisheries and Ocean Studies, India.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kalasseril, S.G., Krishnan, R., Vattiringal, R.K. et al. Detection of New Delhi Metallo-β-lactamase 1 and Cephalosporin Resistance Genes Among Carbapenem-Resistant Enterobacteriaceae in Water Bodies Adjacent to Hospitals in India. Curr Microbiol 77, 2886–2895 (2020). https://doi.org/10.1007/s00284-020-02107-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-020-02107-y