Abstract
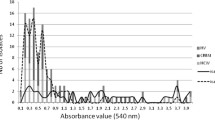
Staphylococcus epidermidis, a human commensal, is an important opportunistic, biofilm-forming pathogen and the main cause of late onset sepsis in preterm infants, worldwide. In this study we describe the characteristics of S. epidermidis strains causing late onset (>72 h) bloodstream infection in preterm infants and skin isolates from healthy newborns. Attachment and biofilm formation capability were analyzed in microtiter plates and with transmission electron microscopy (TEM). Clonal relationship among strains was studied with pulsed-field gel electrophoresis. Antimicrobial susceptibility testing was performed, as well as the detection of biofilm-associated genes and of the invasiveness marker IS256 with polymerase chain reaction. Blood and skin isolates had similar attachment and biofilm-forming capabilities and biofilm formation was not related to the presence of specific genes. Filament-like membrane structures were seen by TEM early in the attachment close to the device surface, both in blood and skin strains. Nine of the ten blood isolates contained the IS256 and were also resistant to methicillin and gentamicin in contrast to skin strains. S. epidermidis strains causing bloodstream infection in preterm infants exhibit higher antibiotic resistance and are provided with an invasive genetic equipment compared to skin commensal strains. Adhesion capability to a device surface seems to involve bacterial membrane filaments.

Similar content being viewed by others
References
Banner MA, Cunniffe JG, Macintosh RL, Foster TJ, Rohde H, Mack D, Hoyes E, Derrick J, Upton M, Handley PS (2007) Localized tufts of fibrils on Staphylococcus epidermidis NCTC 11047 are comprised of the accumulation-associated protein. J Bacteriol 189(7):2793–2804. doi:10.1128/JB.00952-06
Botelho AM, Nunes Z, Asensi MD, Gomes MZ, Fracalanzza SE, Figueiredo AM (2012) Characterization of coagulase-negative staphylococci isolated from hospital indoor air and a comparative analysis between airborne and inpatient isolates of Staphylococcus epidermidis. J Med Microbiol 61(Pt 8):1136–1145. doi:10.1099/jmm.0.035931-0
Bouza E, Alvarado N, Alcala L, Perez MJ, Rincon C, Munoz P (2007) A randomized and prospective study of 3 procedures for the diagnosis of catheter-related bloodstream infection without catheter withdrawal. Clin Infect Dis 44(6):820–826. doi:10.1086/511865
Bowden MG, Chen W, Singvall J, Xu Y, Peacock SJ, Valtulina V, Speziale P, Hook M (2005) Identification and preliminary characterization of cell-wall-anchored proteins of Staphylococcus epidermidis. Microbiology 151(Pt 5):1453–1464. doi:10.1099/mic.0.27534-0
Bradford R, Abdul Manan R, Daley AJ, Pearce C, Ramalingam A, D’Mello D, Mueller Y, Uahwatanasakul W, Qu Y, Grando D, Garland S, Deighton M (2006) Coagulase-negative staphylococci in very-low-birth-weight infants: inability of genetic markers to distinguish invasive strains from blood culture contaminants. Eur J Clin Microbiol Infect Dis 25(5):283–290. doi:10.1007/s10096-006-0130-2
Cheung GY, Otto M (2010) Understanding the significance of Staphylococcus epidermidis bacteremia in babies and children. Curr Opin Infect Dis 23(3):208–216
Costa SF, Miceli MH, Anaissie EJ (2004) Mucosa or skin as source of coagulase-negative staphylococcal bacteraemia? Lancet Infect Dis 4(5):278–286. doi:10.1016/S1473-3099(04)01003-5
D’Angio CT, McGowan KL, Baumgart S, St Geme J, Harris MC (1989) Surface colonization with coagulase-negative staphylococci in premature neonates. J Pediatr 114(6):1029–1034
de Silva GD, Kantzanou M, Justice A, Massey RC, Wilkinson AR, Day NP, Peacock SJ (2002) The ica operon and biofilm production in coagulase-negative Staphylococci associated with carriage and disease in a neonatal intensive care unit. J Clin Microbiol 40(2):382–388
Eftekhar F, Speert DP (2009) Biofilm formation by persistent and non-persistent isolates of Staphylococcus epidermidis from a neonatal intensive care unit. J Hosp Infect 71(2):112–116. doi:10.1016/j.jhin.2008.09.008
Gazzola S, Cocconcelli PS (2008) Vancomycin heteroresistance and biofilm formation in Staphylococcus epidermidis from food. Microbiology 154(Pt 10):3224–3231. doi:10.1099/mic.0.2008/021154-0
Gu J, Li H, Li M, Vuong C, Otto M, Wen Y, Gao Q (2005) Bacterial insertion sequence IS256 as a potential molecular marker to discriminate invasive strains from commensal strains of Staphylococcus epidermidis. J Hosp Infect 61(4):342–348. doi:10.1016/j.jhin.2005.04.017
Hennig S, Ziebuhr W (2010) Characterization of the transposase encoded by IS256, the prototype of a major family of bacterial insertion sequence elements. J Bacteriol 192(16):4153–4163. doi:10.1128/JB.00226-10
Klingenberg C, Ronnestad A, Anderson AS, Abrahamsen TG, Zorman J, Villaruz A, Flaegstad T, Otto M, Sollid JE (2007) Persistent strains of coagulase-negative staphylococci in a neonatal intensive care unit: virulence factors and invasiveness. Clin Microbiol Infect 13(11):1100–1111. doi:10.1111/j.1469-0691.2007.01818.x
Kozitskaya S, Cho SH, Dietrich K, Marre R, Naber K, Ziebuhr W (2004) The bacterial insertion sequence element IS256 occurs preferentially in nosocomial Staphylococcus epidermidis isolates: association with biofilm formation and resistance to aminoglycosides. Infect Immun 72(2):1210–1215
Mack D, Fischer W, Krokotsch A, Leopold K, Hartmann R, Egge H, Laufs R (1996) The intercellular adhesin involved in biofilm accumulation of Staphylococcus epidermidis is a linear beta-1,6-linked glucosaminoglycan: purification and structural analysis. J Bacteriol 178(1):175–183
Marchini G, Nelson A, Edner J, Lonne-Rahm S, Stavreus-Evers A, Hultenby K (2005) Erythema toxicum neonatorum is an innate immune response to commensal microbes penetrated into the skin of the newborn infant. Pediatr Res 58(3):613–616
Milisavljevic V, Wu F, Cimmotti J, Haas J, Della-Latta P, Larson E, Saiman L (2005) Genetic relatedness of Staphylococcus epidermidis from infected infants and staff in the neonatal intensive care unit. Am J Infect Control 33(6):341–347. doi:10.1016/j.ajic.2005.02.003
Mittendorf R, Roizen N, Moawad A, Khoshnood B, Lee KS (1999) Association between cerebral palsy and coagulase-negative staphylococci. Lancet 354(9193):1875–1876. doi:10.1016/s0140-6736(99)01111-3
Nelson A, Hultenby K, Hell E, Riedel HM, Brismar H, Flock JI, Lundahl J, Giske CG, Marchini G (2009) Staphylococcus epidermidis isolated from newborn infants express pilus-like structures and are inhibited by the cathelicidin-derived antimicrobial peptide LL37. Pediatr Res 66(2):174–178. doi:10.1203/PDR.0b013e3181a9d80c
Nilsson M, Frykberg L, Flock JI, Pei L, Lindberg M, Guss B (1998) A fibrinogen-binding protein of Staphylococcus epidermidis. Infect Immun 66(6):2666–2673
Otto M (2011) Molecular basis of Staphylococcus epidermidis infections. Semin Immunopathol. doi:10.1007/s00281-011-0296-2
Stepanovic S, Vukovic D, Hola V, Di Bonaventura G, Djukic S, Cirkovic I, Ruzicka F (2007) Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS 115(8):891–899. doi:10.1111/j.1600-0463.2007.apm_630.x
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33(9):2233–2239
Vandecasteele SJ, Peetermans WE, Merckx R, Rijnders BJ, Van Eldere J (2003) Reliability of the ica, aap and atlE genes in the discrimination between invasive, colonizing and contaminant Staphylococcus epidermidis isolates in the diagnosis of catheter-related infections. Clin Microbiol Infect 9(2):114–119
Wei W, Cao Z, Zhu YL, Wang X, Ding G, Xu H, Jia P, Qu D, Danchin A, Li Y (2006) Conserved genes in a path from commensalism to pathogenicity: comparative phylogenetic profiles of Staphylococcus epidermidis RP62A and ATCC12228. BMC Genomics 7:112. doi:10.1186/1471-2164-7-112
Williams RJ, Henderson B, Sharp LJ, Nair SP (2002) Identification of a fibronectin-binding protein from Staphylococcus epidermidis. Infect Immun 70(12):6805–6810
Vuong C, Kocianova S, Yu J, Kadurugamuwa JL, Otto M (2008) Development of real-time in vivo imaging of device-related Staphylococcus epidermidis infection in mice and influence of animal immune status on susceptibility to infection. J Infect Dis 198(2):258–261. doi:10.1086/589307
Vuong C, Otto M (2002) Staphylococcus epidermidis infections. Microbes and infection/Institut Pasteur 4(4):481–489
Acknowledgments
We are grateful to Eva Andersson, Birgitta Byström, and Ingrid Lindell for invaluable technical assistance. Parts of this study were presented as a poster presentation at the 3rd Congress of the European Academy of Paediatric Societies, Copenhagen 23–26 October 2010. The study was supported by Grants from the Swedish Research Council (Grant No. 0855), ALF (Karolinska Institutet–Stockholm County Council, Agreement on Medical Research and Training) funding, and the Karolinska Institute Research Funds, as well as from Stiftelsen Samariten, Stiftelsen Barncentrum, Sällskapet Barnavård, Lilla Barnets Fond, and Frimurarbarnhuset Stockholm.
Conflict of interests
The authors have no conflict of interests
Ethical standards
This study was approved by the regional ethical committee for medical research (EPN) in Stockholm, Sweden (2007/674-31/1).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hell, E., Giske, C.G., Hultenby, K. et al. Attachment and Biofilm Forming Capabilities of Staphylococcus epidermidis Strains Isolated from Preterm Infants. Curr Microbiol 67, 712–717 (2013). https://doi.org/10.1007/s00284-013-0425-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-013-0425-3