Abstract
A vaccine to prevent infections caused by Staphylococcus aureus would have a tremendously beneficial impact on public health. In contrast to typical encapsulated bacterial pathogens, such as Streptococcus pneumoniae, H. influenzae, and Neisseria meningitides, the capsule of S. aureus is not clearly linked to strain virulence in vivo. Furthermore, it is not clear that natural infection caused by S. aureus induces a protective humoral immune response, as does infection caused by typical encapsulated bacteria. Finally, pure B cell or antibody deficiency, in either animal models or in patients, does not predispose to more frequent or more severe S. aureus infections, as it does for infections caused by typical encapsulated bacteria. Rather, primary immune mechanisms necessary for protection against S. aureus infections include professional phagocytes and T lymphocytes (Th17 cells, in particular) which upregulate phagocytic activity. Thus, it is not clear whether an antibody-mediated neutralization of S. aureus virulence factors should be the goal of vaccination. Rather, the selection of antigenic targets which induce potent T cell immune responses that react to the broadest possible array of S. aureus strains should be the focus of antigen selection. Of particular promise is the potential to select antigens which induce both humoral and T cell-mediated immunity in order to generate immune synergy against S. aureus infections. A single-antigen vaccine may achieve this immune synergy. However, multivalent antigens may be more likely to induce both humoral and T cell immunity and to induce protection against a broader array of S. aureus isolates. A number of candidate vaccines are in development, raising the promise that effective vaccines against S. aureus will become available in the not-so-distant future. Possible development programs for such vaccines are discussed.
Similar content being viewed by others
Introduction
Staphylococcus aureus is a ubiquitous pathogen. It is the most common cause of culture-confirmed skin and soft tissue infections (SSTIs) [1–4] and endocarditis [5], and is the second most common cause of bacteremia [6, 7]. S. aureus is also a predominant cause of a variety of nosocomial infections, including ventilator-associated pneumonia, intravenous catheter-associated infections, postsurgical wound infections, as well as invasive infections in neutropenic patients and in patients undergoing solid organ or hematopoeitic stem cell transplants [8].
Invasive infections caused by S. aureus continue to increase in frequency [9, 10]. Population-based estimates of the incidence of S. aureus infections have ranged from a low of approximately 30 per 100,000 [11, 12] for analyses restricted to invasive (beyond skin) disease to up to 600 per 100,000 based on extrapolation from a surveillance study in the USA [13]. In a separate study from Europe, the incidence of just bacteremia caused by S. aureus was reported to be 30 per 100,000 [14]. Given that >90% of infections caused by S. aureus are skin infections [15], incidences of S. aureus bacteremia of ∼30 per 100,000 support the estimate of approximately 600 per 100,000 total incidence of S. aureus disease reported by the CDC. Therefore, there may be 1.8 million cases of S. aureus infection (including skin infection) per year in the USA alone, which obviously provides a potentially massive market to stimulate interest in vaccine development.
Community-associated S. aureus infections were formerly nearly uniformly susceptible to penicillinase-resistant beta lactams (i.e., methicillin, oxacillin, etc.). However, over the past decade, a number of community-based outbreaks of methicillin-resistant S. aureus (MRSA) infections have emerged, initially in pediatric populations [16–18]. Community outbreaks of MRSA infections also have been seen in adults in multiple locales in the USA and across the globe, and in many places, MRSA has become the predominant S. aureus strain causing community-acquired infections [15, 19–23]. The rise in MRSA incidence underscores the need to develop new strategies to prevent invasive S. aureus infections.
Given its high incidence of causing life-threatening, drug-resistant infections, a vaccine to prevent S. aureus infections would have an enormous and beneficial impact on global and US health. The purpose of this review was to broadly discuss challenges to and the promise of developing S. aureus active vaccines. Issues ranging from fundamental immunology, to antigen targets, to practical considerations for development programs are discussed.
Fundamental immune underpinnings of a S. aureus vaccine
What type of immune response should be stimulated?
When rationally designing a vaccine against a specific disease, it is desirable to understand what mode of immunity, when induced, will serve to protect the host from the target infection. Vaccines which induce the protective mode of immunity can then be developed. There are two types of studies which can elucidate the nature of protective immunity against specific diseases. For example, natural infection may induce a specific type of memory immune response which protects against subsequent reinfection. Identification of the nature of that protective memory response in patients with previous natural infection can be used to elucidate what type of immune response to focus on when vaccinating immunologically naive patients.
A second means to elucidate the nature of protective immunity against a specific disease is definition of the nature of immune defects which specifically predispose to the disease. These two types of data—description of the type of immunity that is protective after natural infection and description of specific immune defects that predispose to infection—provide complementary information. Specifically, protective immunity after natural infection elucidates immunity that is sufficient to protect against reinfection, and immune defects that predispose to infection elucidate immunity that is necessary to protect against infection.
Based on these principles, the design of vaccines targeting toxin-mediated diseases is relatively straightforward: immunize with a detoxified toxin analogue to generate neutralizing antibodies (e.g., diphtheria, pertussis, tetanus toxoid). Similarly, for viral diseases, successful vaccines based on whole virus (e.g., hepatitis A virus), viral antigens (e.g., hepatitis B virus), or viral-like particles (e.g., human papilloma virus) have been designed to generate antibodies that block viral interaction with host cells and induce cytotoxic T lymphocytes to kill virally infected host cells [24]. In these examples, the vaccines are designed to induce an immune response which mimics protective immunity against natural disease caused by the target toxin or pathogen and also stimulates mechanisms of host defense which, when absent, predispose to the target disease.
Similarly, the underpinning of vaccination against typical encapsulated bacterial pathogens (e.g., Streptococcus pneumoniae, Hemophilus influenzae type b, Neisseria meningitidis) is based in part on the well-described hypersusceptibility to these infections of patients with congenital or acquired B cell/antibody deficiencies as well as the same hypersusceptibility of animal models in which B cell/antibody function is disrupted [25]. These clinical and experimental immunologic observations are further bolstered by data establishing that antibody concentrations correlate with protective immunity after natural infection caused by such encapsulated organisms [24]. Hence, vaccines against encapsulated bacterial pathogens are designed to stimulate antibodies that neutralize the anti-phagocytic capacity of the polysaccharide capsule of S. pneumoniae, H. influenzae, and N. meningitidis, enabling the host immune system to clear the organism [24].
After more than a half century of successful vaccine development for toxin, viral, and encapsulated bacterial diseases, it is perhaps not surprising that initial efforts to develop a staphylococcal vaccine were based on a presumption that the same immunologic mechanism would be protective: a humorally focused vaccine and one that targeted capsular polysaccharide just as for other bacterial pathogens. Unfortunately, efforts to date to develop such a vaccine have not been successful (discussed further below). A primary reason for such efforts not having been successful is likely that the fundamental immunopathogenesis of S. aureus infections differ from the immunology of toxin-based, viral, and typical encapsulated bacterial infections.
S. aureus immunology and immunopathogenesis
The nature of protective immunity sufficient to protect against reinfection following natural infection is not known for S. aureus
Unfortunately, in contrast to toxin, viral, and encapsulated bacterial infections, we have virtually no understanding of the correlates of protective immunity against S. aureus infection. It is clear that S. aureus invasive infections result in the generation of a memory immune response typified by specific antibody at higher titers post-infection than pre-infection [26–30]. However, it has not been established that the memory immune response occurring after natural infection with S. aureus results in protection against reinfection. One recent study found no relationship between specific anti-Panton Valentin leukocidin (PVL) antibody titers post-infection and risk of recurrence [28]. Furthermore, recurrence is a well-established clinical hallmark of S. aureus cutaneous abscesses [31, 32]. Indeed, in various studies analyzing widely disparate patient populations, approximately 10–30% of initial S. aureus cutaneous abscesses resulted in recurrence [33–39]. Hence, natural infection with S. aureus does not reliably result in an immune response which prevents future recurrence. Absent knowing that a protective memory response occurs after natural S. aureus infection, it is certainly not possible to define the nature of such protective memory responses.
Much has been published regarding the ability of S. aureus to subvert normal host defense mechanisms [40, 41]. Mechanisms of the organism implicated to achieve such immune subversion include the prevention of complement deposition, prevention of antibody-mediated opsonophagocytosis, evasion of phagocytic killing, toxin-mediated lysis of white blood cells, and dysregulated immune hyperactivation via superantigens. None of these mechanisms clearly affect the generation of a memory response to infection or elucidate why such responses would or would not be protective.
Indeed, clinical experience suggests that protective immunity may actually develop post-infection in some patients, although it likely does so variably for reasons that we do not understand. For example, while recurrent infections are common in patients with S. aureus cutaneous abscesses, many patients never develop recurrences despite the ubiquity of the pathogen. Furthermore, for those who do develop recurrences, eventually, even repeated recurrences typically cease.
More compelling regarding the role of adaptive cell-mediated immunity in protecting against recurrent S. aureus infections is the fact that patients with defects in T cell immunity (e.g., HIV) clearly have higher recurrence rates than patients with intact T cell function; 50–70% of HIV-infected patients with an initial S. aureus abscess develop recurrence [39, 42–44], which is approximately two- to threefold higher than the previously discussed recurrence rate in non-HIV-infected patients. Similarly, as discussed further below, patients with genetic defects in STAT3, resulting in hyper-IgE syndrome (also called Job’s syndrome) and defective Th17 cell function, experience recurrent and often severe S. aureus abscesses [45–49]. These results strongly suggest that an intact cell-mediated immune axis results in immunological memory that reduces the risk of recurrence of S. aureus infections compared with patients with defective cell-mediated immunity. Furthermore, as mentioned, many patients never develop recurrence of cutaneous abscesses, suggesting that immunity may develop in some patients after initial cutaneous infection. Why protective memory immunity may develop post-infection with S. aureus in some patients and not in others is not clear, and immunological differences which distinguish protective from non-protective responses have never been elucidated.
Hence, in contrast to diseases for which vaccines have been successfully deployed (i.e., toxin-mediated, viral, and typical encapsulated bacteria), we simply do not know the correlates of protective immunity after natural infection for S. aureus. This absence of understanding of immune correlates of protection greatly complicates preclinical selection and optimization of vaccine candidates, and further complicates clinical development, since surrogate markers for protection cannot be known during phase I and II clinical trials. Quite simply, until a vaccine against S. aureus is shown in the clinic to prevent infection caused by S. aureus, only clinical outcome data can be used to evaluate the efficacy of a S. aureus vaccine. Once an effective vaccine is developed, immunological markers can be compared as to their efficacy to determine which markers serve as correlates of protective immunity. Then and only then can such markers serve to reliably focus and simplify the preclinical selection and clinical development of subsequent S. aureus vaccine candidates.
Critical lessons from available natural experiments: what type of host defense mechanism(s) is necessary to protect against S. aureus infections?
It is clearly established that patients deficient in B lymphocytes or with congenital or acquired deficiency in specific antibody production are at a markedly higher risk of acquiring infections caused by typical encapsulated bacteria and a variety of viral infections [50–52]. These infections are not only more common but also typically far more severe when they occur in B lymphocyte- or antibody-deficient patients. Hence, not only are antibodies sufficient for protection against such infections (because they result in natural immunity post-infection) but they also appear to be necessary to protect against such infections.
What do similar natural experiments tell us regarding S. aureus infections? The immunopathogenesis of S. aureus infections stands in contrast to typical encapsulated bacterial infections. Patients with pure B cell or antibody deficiency, or asplenic states, are not at a higher risk of S. aureus infections, nor do they have especially severe S. aureus infections when such infections occur [25]. The exception that proves the rule is that antibody-deficient patients with recurrent respiratory tract infections that lead to anatomical abnormalities (e.g., loss of normal ciliary function, bronchiectesis, lung blebs) are at increased risk of S. aureus superinfections [51, 52]. These infections do not occur until later in life, after patients have experienced sufficient numbers of upper respiratory infections caused by encapsulated bacterial pathogens to cause the anatomical abnormalities. Hence, these S. aureus infections are the result of the anatomical abnormalities, not the antibody deficiency per se. Thus, in contrast to viral infections and encapsulated bacterial infections, B cells and antibody are not necessary for host defense against S. aureus infections.
Patients who are definitively at increased risk of developing S. aureus infections are those with disruptions of anatomical barriers (e.g., by cutaneous burns, intravenous catheters, endotracheal tubes, surgical or traumatic wounds, post-viral ciliary airway disruption) and those with quantitative (e.g., chemotherapy-induced neutropenia) or qualitative (e.g., chronic granulomatous disease, leukocyte adhesion deficiency, Chediak–Higashi syndrome) neutrophil disorders.
As mentioned, the increased risk of S. aureus infections in HIV-infected patients supports the concept that T cell dysfunction is a risk factor for such infections. Furthermore, the role of T cells in host defense against S. aureus infections is supported by the recent elucidation that STAT3 deficiency results in hyper-IgE syndrome [45–49]. STAT3 is a critical upstream regulator of Th17 differentiation, and Th17 dysfunction or absence is a prominent immunological phenotype in hyper-IgE syndrome. Hyper-IgE syndrome patients and those with Th17 defects have a markedly increased risk in developing both cutaneous and pulmonary infections caused by S. aureus. These findings provide a critical clue to the link between T cell function and neutrophil function in host defense against S. aureus infections. Specifically, Th17 cells are potent inducers of neutrophil chemotaxis to sites of infection and enhance the activation of neutrophils at sites of infection [53, 54]. Disruption of the Th17 axis therefore results in a delayed, diminished recruitment of neutrophils and a diminished activation of the phagocytes, which facilitate long-term bacterial persistence and chronic inflammation at sites of infection.
Recently, murine models have been described to recapitulate, in well-controlled experiments, the above clinical findings. Specifically, we reported for the first time that B cell-deficient mice are no more susceptible to systemic/bloodstream infection caused by S. aureus compared with wild-type mice [55]. In contrast, T cell-deficient mice were hypersusceptible to infection. gp91phox−/− superoxide-deficient mice (a model of chronic granulomatous disease) were also hypersusceptible to infection. Furthermore, Th17 cells were necessary for vaccine-induced protection against S. aureus infection in the murine model, and such cells acted by enhancing neutrophil recruitment to sites of infection and by enhancing killing of S. aureus by neutrophils [56].
We have also found that IFN-γ-deficient mice are hypersusceptible to infection caused by S. aureus inoculated intravenously [55, 57]. Others have found that dual IL-17A/F-deficient mice had an increased incidence of developing spontaneous skin infections caused by S. aureus [58]. Hence, a new immunologic strategy to develop an anti-S. aureus vaccine may be to induce memory T cells which are capable of increasing the rapidity and strength of phagocyte recruitment to sites of infection, facilitating clearance of the organism from tissues.
In contrast to the systemic model of infection, in the skin model of infection, B cell deficiency resulted in the exacerbation of the size of the dermonecrotic lesion, whereas T cell deficiency and IL-17A deficiency resulted in smaller dermonecrotic lesions (manuscript submitted). The impact of lymphocyte and IL-17A deficiency on lesion size was due to alterations in inflammatory response, and lesion size correlated better with inflammatory cytokine and neutrophil influx levels than with tissue bacterial burden. Hence, the size of cutaneous infections appears to be driven as much by the inflammatory response to the organism as by the number of organisms present. Vaccination resulted in a more balanced Th1–Th2 inflammatory response while still enhancing neutrophil influx, leading to the amelioration of lesion size.
Thus, clinical experience with patients with congenital or acquired immune defects combined with data from carefully controlled murine models indicates that antibodies are not required for host defense against S. aureus infections. In contrast, normal anatomical barriers to infection and normal numbers and functions of neutrophils are critical to host defense against S. aureus infections. T cells play a critical role in regulating the downstream phagocytic response, both by enhancing the recruitment and activation of neutrophils to better kill S. aureus at sites of infection and also possibly by restraining out-of-control inflammation in cutaneous lesions. These data do not support the concept that vaccination against S. aureus should be designed to stimulate the same type of immunity as for toxin, viral, or encapsulated bacterial infections.
A review of past and present S. aureus vaccines: focus on antigen selection
Capsular polysaccharide vaccines
For many years, efforts to develop an anti-S. aureus vaccine candidate were focused on capsular polysaccharide as a putative protective antigen. The leading effort in this regard was StaphVAX, a bivalent vaccine comprising S. aureus capsular polysaccharide types 5 and 8 bound to pseudomonal exotoxoid A as a carrier. In phase II clinical trials, the vaccine resulted in high antibody titers that lasted for approximately 6 months in patients undergoing chronic hemodialysis [59–61]. Furthermore, a booster dose appeared to maintain antibody levels for more than a year. Unfortunately, in a large pivotal phase III trial, StaphVAX did not reduce the incidence of invasive S. aureus infections in hemodialysis patients [62]. This lack of protective efficacy occurred despite the presence of impressive, opsonophagocytic, anti-capsular antibody concentrations in immunized patients. Thus, the induction of specific immune serum to S. aureus does not necessarily result in protection, and anti-capsular antibodies are not inherently protective against S. aureus as they are against, for example, S. pneumoniae.
Aside from the immunological concerns regarding the role of B cells in host defense against S. aureus, another factor limiting a capsular polysaccharide approach is that many clinical isolates lack a capsule. For example, the major genetic background causing epidemic community-acquired MRSA infection, USA300, elaborates no detectable capsular polysaccharide [63]. Furthermore, in the phase II trial of StaphVax, 20% of isolates were identified as having type 336 capsular antigen [61], which has subsequently been reported to be polyribitol phosphate N-acetylglucosamine (resembles cell wall teichoic acid) and is not a capsular polysaccharide at all [64, 65]—that is, 20% of isolates in the trial had no detectable capsule.
Surface antigen passive immunization
Passive vaccine strategies targeting S. aureus surface antigens have also been attempted. The Aurexis(™) anti-staphylococcal monoclonal antibody targets the microbial surface components recognizing adhesive matrix molecule, clumping factor A. A phase II clinical trial of Aurexis(™) as an adjunctive therapy in patients with established S. aureus bacteremia resulted in a non-significant trend toward improved outcomes for treated patients [66]. However, in another study, high-titer anti-clumping factor A polyclonal antibody resulted in no clinical benefit among high-risk premature neonates and did not reduce the risk of developing invasive staphylococcal infection [67]. Another surface target is wall techoic acid. Biosynexis has a chimeric monoclonal antibody targeting wall techoic acid in phase III clinical trials for the prevention of staphylococcus sepsis in very low birth neonates (NCT00646399). The results of the trial are anticipated in 2011.
The failure of an active, polysaccharide capsular-based vaccine despite a successful induction of opsonophagocytic antibodies, combined with the failure of passive immunization against S. aureus surface proteins in clinical trials, highlights a logical disconnect between these humoral-based strategies deployed against S. pneumoniae, H. influenzae, and N. meningitidis versus a similar approach against S. aureus.
Virulence factors as target antigens
Another strategy to develop a S. aureus vaccine has been based on the notion that the neutralization of virulence factors elaborated by the bacterium could ameliorate or prevent disease. Numerous virulence factors have been targeted by vaccination, including alpha hemolysin, PVL, clumping factor A, fibrinogen binding protein, enolase (laminin-binding protein), and protein A. A recent study found that antibodies against LukD and LukF (leukocidins), alpha toxin, and SEA (in addition to antibodies against numerous other antigens) were generated after S. aureus bacteremia in mice [68]. Different vaccines targeting such antigens have been shown to provide varying levels of protection to mice against systemic infection caused by S. aureus. For example, active vaccination with a detoxified alpha hemolysin and passive immunization against alpha hemolysin ameliorated the size of skin lesions and the severity of pneumonia in mice infected with a USA300 strain of MRSA [69–71]. Vaccination with PVL subunits also ameliorated the severity of pneumonia and skin infections in mice infected with MRSA [72]. A variety of adhesins, including clumping factor A, clumping factor B, enolase, and fibrinogen-binding protein, have all been shown to ameliorate the severity of systemic S. aureus infection or prevent nasal colonization by S. aureus in mice [73–79].
Some of these vaccine candidates have thus far only been shown to be effective when administered with Freund’s adjuvant, which is too toxic for clinical use. Similarly, when administered with Freund’s adjuvant, a vaccine containing multiple antigens was more effective than a single-antigen vaccine against IV infection [80]. The enhanced efficacy of a multi-antigen vaccine in this study has become important to the belief that virulence factor neutralization can be an effective strategy for a S. aureus vaccine, but that multiple factors must be neutralized by vaccination because S. aureus elaborates so many factors that contribute to its pathogenesis [77, 80–82]. Working on this hypothesis, a pentastaph vaccine containing capsular polysaccharide types 5 and 8, techoic acid (cell wall antigen type 336), Panton Valentin leukocidin, and alpha hemolysin has been developed initially by Nabi and then acquired by Glaxo Smith Kline. That vaccine is currently in phase I clinical trials (NCT01160172).
It must be emphasized that an antibody-mediated neutralization of virulence factors has never been established to be an effective mechanism of protection against S. aureus infection. It is not at all clear that virulence factors, whether toxins or surface adhesins, make better antigens than any other types of targets which induce potent immune responses. Nevertheless, it is possible that a multivalent vaccine will result in superior efficacy because it could facilitate the development of a vaccine that: (1) results in the induction of both humoral and cell-mediated immunity by distinct antigens and (2) results in a greater probability that any one antigen included will trigger a potent immunodominant response in highly genetically diverse populations since both mice and humans have extremely variable antibody responses to a diverse array of antigens from S. aureus post-infection [29, 68]. Furthermore, it is clear that different anatomical sites of infection (e.g., lung, blood, skin) result in different immunodominant antigenic foci for the immune response [68]. Therefore, a multivalent vaccine may have a greater chance of preventing S. aureus infections at multiple anatomical sites than a monovalent vaccine.
Iron acquisition as target antigens
Iron is of fundamental importance to microbial pathogenesis, and S. aureus is no exception [83–87]. Prevention of iron uptake by S. aureus results in the inhibition of bacterial growth and bacterial death [88, 89]. S. aureus has evolved numerous iron uptake mechanisms which facilitate iron acquisition in the host during infection in various anatomical contexts. Many of the proteins involved in iron acquisition have been or are being targeted as vaccine candidates.
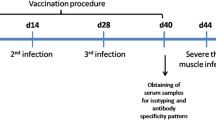
The leading vaccine candidate at the current time is based upon the S. aureus iron-binding protein (IsdB) [90]. IsdB was initially identified as a promising candidate vaccine antigen by probing S. aureus open reading frames in an Escherichia coli expression library using serum from patients infected with S. aureus or control serum [91]. Proteins identified by the immune serum but not control serum would be recognized as immunogenic after infection with S. aureus. Such a screening method is a logical means to identify immunogenic antigens from S. aureus, although the resulting protection cannot be inferred from this method. Thus, once IsdB was identified as a robustly immunogenic S. aureus antigen across multiple donors’ immune serum, the protein was produced and tested for efficacy as a vaccine antigen in a murine model of S. aureus i.v. tail vein infection resulting in sepsis [90]. For all six S. aureus strains tested, inbred and outbred mice immunized with IsdB plus aluminum hydroxide adjuvant had superior survival post-infection than adjuvant control mice. The protein was found to be highly conserved across S. aureus strains. Furthermore, the protein was immunogenic in macaque monkeys. A humanized monoclonal antibody targeting IsdB was found to protect mice in a murine sepsis model and to reduce bacteremia and prevent central venous catheter colonization in a rat model [92].
Three doses (5, 30, or 90 μg) of aluminum adjuvanted IsdB vaccine were compared with saline placebo in a double-blinded, phase I clinical trial [93]. The two higher doses were more immunogenic, and the vaccine was well tolerated. The vaccine was then studied in a very large blinded, randomized, placebo-controlled phase II study of patients undergoing elective cardiothoracic surgery (NCT00518687). Unfortunately, IsdB was the latest S. aureus vaccine candidate to fail in clinical trials. The precise reason for the phase II clinical trial being stopped prematurely is not yet completely understood.
IsdA is also a target of immune response during S. aureus infection in mice [68]. Another multicomponent vaccine platform targeting iron acquisition in S. aureus is being developed by Syntiron in collaboration with Sanofi Pasteur. Other vaccines are in development as well, in trials sponsored by Pfizer and Novartis, both of which are multicomponent vaccines and are entering phase I clinical trials.
An antigen that induces protective Th17-based immunity
Another novel vaccine strategy against S. aureus is based on the immunologic cross-reactivity of the candidal recombinant N-terminus of Als3p (rAls3p-N) vaccine against S. aureus cell wall preparations [55, 57]. The precise antigenic targets of S. aureus that cross-react to rAls3p-N have not been identified. However, specific immune cross-reactivity between lysostaphin cell wall preparations and rAls3p-N was established [55].
The immunology of this vaccine offers new insights into immunologic mechanisms by which vaccines may be effective at protecting against invasive S. aureus infections. The rAls3p-N vaccine induced high antibody concentrations, but these antibodies were not protective when used to passively immunize against S. aureus intravenous challenge [55]. Concentrations of anti-rAls3p-N antibodies in individual mice did not correlate well with the risk of death from staphylococcal infection [94]. Furthermore, the vaccine was equally effective in B cell-deficient mice as in wild-type mice, but had no efficacy in T cell-deficient mice [55]. The adoptive transfer of immune B220+ B cells did not transfer protection, but the transfer of CD4+ T cells did transfer protection. The vaccine was ineffective in IFN-γ- and IL-17A-deficient mice, and in gp91phox−/− mice that are unable to produce superoxide. These mice are therefore used as an animal model for chronic granulomatous disease [94]. Cross-adoptive transfer experiments confirmed that functional phagocytes were operative in vaccine-mediated protection at the downstream effector stage, not the upstream lymphocyte priming stage. Finally, vaccination increased the recruitment and activation of phagocytes at sites of tissue infection in mice, and cytokines produced by vaccine-primed lymphocytes markedly improved the ability of phagocytes to kill S. aureus. Hence, the rAls3p-N vaccine demonstrates that it is feasible to induce a protective immune response in mice against S. aureus in the absence of the induction of protective antibodies and by inducing a protective Th1/Th17 response.
Clinical and animal model experience has indicated that hosts deficient in phagocytes, or phagocytic function, are specifically predisposed to S. aureus infection [25, 57]. This concept strongly suggests that vaccines can be developed to specifically enhance phagocytic-mediated host defense mechanisms against S. aureus. Nevertheless, recent experiences confirm that it is possible to induce and identify protective antibodies even against diseases which are clearly not dependent on antibody-mediated protection. Examples include disseminated candidiasis and invasive aspergillosis [95–97]. Therefore, the available immunopathogenesis data do not preclude the development of a humoral-based vaccine against S. aureus. Rather, they suggest that cell-mediated vaccines merit additional focus and raise the possibility of combining antigens that stimulate both humoral and cellular responses against the pathogenic organism. Indeed, the latter may be the most likely strategy to result in a strongly protective vaccine against S. aureus.
How to target potential patients for a S. aureus vaccine development program?
Risk factors for S. aureus infections are well described
Although patients with no risk factors frequently developed skin infections caused by S. aureus in the community, risk factors associated with a higher risk of developing staphylococcal infections are well characterized. Distinct patient populations develop invasive S. aureus infections in health care-associated and in community settings. Health care-associated risk factors for invasive S. aureus infections include the presence of indwelling catheters, endotracheal intubation, and foreign bodies (e.g. peritoneal dialysis catheters, prosthetic joints and orthopedic implants, prosthetic heart valves, etc.), stay in an ICU, and surgical procedures/trauma [8, 11, 14]. Patients not in a health care setting who are at a higher risk of developing invasive S. aureus infections include patients with chronic defects in cell-mediated immunity (e.g., HIV-infected, those on corticosteroids, etc.); patients with poorly characterized immune dysfunctions associated with metabolic or nutritional disorders (e.g., diabetics, alcoholics, cancer patients, dialysis patients); and patients with congenital phagocytic defects (e.g., chronic granulomatous disease, Chediak–Higashi syndrome, Job’s syndrome, Wiskott–Aldrich Syndrome, etc.) [8, 11, 14]. In aggregate, the number of people at risk of an invasive staphylococcal infection numbers in the many millions per year in the USA alone. However, vaccination strategies targeting community versus nosocomial disease would likely differ substantively in development plans.
Vaccines targeting community-onset S. aureus infections
More than 90% of community-onset S. aureus infections are SSTIs, typically presenting as cutaneous abscesses or cellulitis. Abscesses are treatable with incision and drainage; the need for adjunctive antibacterial therapy in this setting is an open question as available studies to date have been underpowered [98]. However, cellulitis requires antibacterial therapy. Furthermore, the remainder of such infections is more invasive and may lead to community-onset bacteremia, endocarditis, deep tissue abscesses, osteomyelitis, etc. As mentioned, while specific risk factors do identify subjects with higher than normal risk of developing community-onset S. aureus infections, everyone is at risk of such infections.
Two general strategies for developing a vaccine against community-onset S. aureus infections are apparent (Table 1): first is the large-scale vaccination of the general public to prevent infections on a population basis; second is the focused vaccination on high-risk individuals who have a defined period of extra risk.
Large-scale vaccination of the general public requires a much larger clinical development program, but would result in a much larger market should efficacy be established in a pivotal phase III study. Because so many patients would be vaccinated relative to the small number who would otherwise develop infection in this development strategy, there would be little tolerability for adverse events (even if such events resulted in only mild or temporary changes quality of life rather than in long-term sequelae). Furthermore, it is likely that the market size would be somewhat mitigated by a lower per unit price since the number of infections prevented per vaccinated individual would be relatively small and most of the infections prevented would be non-life-threatening simple abscesses. Finally, such a vaccine would either require prolonged resulting immunity or would require periodic boosting, given the indefinite risk of community-onset infection among the general public.
In contrast, a development strategy for community-onset S. aureus infection focused on high-risk individuals would be designed quite differently. Perhaps the most feasible (but not the only) trial design for preventing community-onset S. aureus infection in super-high-risk individuals would be to enroll military recruits prior to the initiation of basic training. Multiple publications have described frequent S. aureus infections in military personnel [99–104]. A high attack rate in healthy individuals has been found during military basic training [100, 102, 103]. In one study, the attack rate of S. aureus infections during just the 8- to 10-week period of basic training for new recruits was 3.5% (29/812). Furthermore, of patients colonized in the nose with S. aureus at baseline, the attack rate of S. aureus infections during basic training doubled to 7% (17/253). Of patients colonized with MRSA at baseline, the attack rate was much higher (38%). Based on this attack rate in the control arm, if patients known to be colonized with MRSA at baseline were the target population for enrollment in a clinical trial of a vaccine to prevent subsequent infection, only 90 patients per arm would be required to achieve an 80% power to detect a 50% decrease in infection attack rate (α = 0.05).
The advantages of studying a vaccine for efficacy in military recruits include a high enrollment rate of eligible study subjects, a relatively high and defined attack rate in the control arm over a short period of time, the enrollment of subjects with healthy immune systems, and the relative ease of data capture given the close monitoring of enrolled subjects that is feasible in such a situation. Such a study would be far smaller and less expensive than would occur in a large-scale!! population-based development program. As well, the tolerability for minor adverse events (such as discomfort at the injection site, brief fever, etc.) would be higher in military recruits than in a program targeting the general population. The trade-off would be the potential loss of efficacy by enrolling subjects already known to be colonized with infection (if, for example, the vaccine’s primary benefit was to prevent colonization as an initial step in the pathway eventually leading to infection) and the resulting approval for a narrower indication, which would result in a smaller overall market. However, the smaller market size would be partially mitigated by the likely ability to charge a higher dollar amount per unit dose since the number of infections prevented per vaccine recipient would be substantially higher. Other possible populations at specific risk of focusing a community-onset S. aureus vaccine development program could include students or professional athletes, although the attack rate is less well defined in these populations and likely lower than in military recruits. Furthermore, household contacts of index patients [105], prison inmates (at time of entry into prison) [106, 107], and those with a history of prior S. aureus infection [33–39, 105] all have high subsequent attack rates and would be populations reasonable to target for a clinical trial.
Vaccines targeting health care-associated S. aureus infections
In contrast to community-onset infections caused by S. aureus, nosocomial infections caused by S. aureus are typically life-threatening. Such infections include ventilator-associated pneumonia, catheter-associated bacteremia, and postsurgical wound infections. The prevention of such infections would not just improve quality of life but would also reduce mortality. Furthermore, a recent study found that patients with specific risk factors had rates of S. aureus bacteremia in excess of 10% [108]. Hence, targeting patients with these risk factors would enable the achievement of an attack rate feasible for an adequately powered phase III clinical trial. Since the risk of mortality and serious morbidity is greater for hospital-acquired S. aureus infections, the quality-adjusted life years saved of administering an anti-S. aureus vaccine to prevent hospital-acquired infections would be substantially greater than for preventing community-acquired infections. Hence, even though the number of eligible subjects would be smaller, the cost per dose charged by a sponsor for an indication to prevent hospital-acquired infections would likely be substantially greater than for an indication to prevent community-onset infection.
Another clinical development pathway for an active vaccine is the prevention of reinfection in patients who have experienced a S. aureus infection. Lucero et al. [109] conducted a population-based surveillance study of MRSA infections to estimate the impact of a vaccine on preventing such infections. The authors evaluated the potential for a vaccine to prevent MRSA infections in three vaccination strategies, including: (1) all individuals ≥65 years of age, (2) all individuals ≥65 years of age plus persons 15–64 years of age with a history of previous invasive MRSA infection, and (3) all individuals ≥65 years of age plus persons 15–64 years of age at hospital discharge (hospitalization for any indication). Their baseline estimate of disease burden was 38 cases per 100,000, which likely grossly underestimates (by approximately nine- or tenfold) the true incidence of MRSA infections if simple abscesses are included [13, 110]. Thus, the analysis focuses primarily on deep, invasive infections. They estimated that the greatest impact on disease reduction would occur if patients were targeted at hospital discharge (17% reduction in MRSA cases predicted). By comparison, vaccination of all adults >65 years old or all patients with a previous episode of MRSA infection were predicted to result in 12% or 14% reductions in MRSA infections, respectively.
Will compromised hosts respond to a vaccine against S. aureus?
A vaccination program focused on the prevention of community-onset infection would predominantly target immune competent individuals. In contrast, a vaccination program focused on preventing health care-associated S. aureus infections would by necessity involve vaccinating patients with a variety of comorbidities. In particular, vaccination of acutely ill inpatients at risk of invasive S. aureus infections would require the effective vaccination of a variety of types of critically ill patients. The question is raised, are such patients likely to respond to vaccination with a sufficiently potent response to generate protective immunity?
However, numerous clinical studies have confirmed that most patients with even substantial and specific defects in cell-mediated immunity respond to a variety of vaccines. For example, HIV-infected patients and patients with active uncontrolled malignancies, including leukemia, have been shown to generate immune responses to and be protected from infection by a variety of vaccines [111–132]. Therefore, the concept that immunocompromised patients can be protected from invasive infection by immunization has been well validated and extensively documented in both immunogenicity and clinical outcomes studies. Given the established vaccine immunogenicity and clinical efficacy in patients with HIV infection and cancer/chemotherapy-related neutropenia, it is highly likely that patients with poorly characterized immune defects due to acute critical illness will also respond to vaccination.
Summary
Failed efforts to develop a S. aureus vaccine to date do not diminish the real potential for effective vaccines to become available in the clinic within the next 10 years. Over the past decade, we have learned critically important lessons regarding the fundamental immunopathogenesis of S. aureus infections and regarding the mechanisms of immune protection against infection. Previous S. aureus vaccine efforts have focused on capsular polysaccharides as an extrapolation from a half century of successful efforts to develop vaccines against infections caused by typical encapsulated bacterial pathogens. However, the fundamental mechanisms of host defense which protect against typical encapsulated bacterial infections differ from those operative against S. aureus. The former are primarily defended against by opsonophagocytic antibodies. In contrast, protection against S. aureus infections requires intact phagocytic function and is markedly enhanced by Th1/Th17 adaptive immunity. These facts do not preclude the possibility of developing a vaccine which is operative by inducing protective antibodies. Rather, they indicate that vaccines targeting S. aureus do not have to focus on stimulating neutralizing or opsonophagocytic antigens and that cell-mediated focused vaccines can effectively protect against S. aureus infections.
Furthermore, these facts indicate that antigenic targets of vaccination do not have to be focused on virulence factors, with the intention of neutralizing such factors and/or inhibiting their function. Any S. aureus antigens which induce a potent immune response that effectively targets the organism for destruction by enhancing phagocytic effectors can serve as an effective vaccine antigen, whether the antigen is a capsular component, a cell surface adhesion, a virulence factor, or simply a housekeeping protein which is present at high concentrations and is accessible to immune recognition. More important than the biological role of the microbial antigen is the induction of a potent immune response in as broad a population of targeted patients as possible.
The concept of developing a vaccine based on multivalent antigens has been popularized in recent years. The purported benefit of multivalent antigens has previously been described as targeting multiple virulence factors for a pathogen which is so complex and deploys numerous virulence factors to cause disease. However, perhaps a more relevant promise of multivalent vaccines is the ability to incorporate distinct antigens that (1) induce complementary, non-overlapping immune mechanisms of protection, such as a humoral-inducing antigen and a Th1 or Th17 cell-mediated inducing antigen, and (2) are capable of inducing potent immunity even in diverse human populations which intrinsically respond to myriad different S. aureus antigens with great variability. In contrast, a single antigen will only be effective in a smaller subset of patients who respond particularly well to that specific antigen and may not be capable of inducing potent protection by both humoral- and cell-mediated immunity.
A wide variety of clinical development programs should be feasible for a S. aureus vaccine targeting community-onset or health care-associated infections. These varied possible programs will facilitate clinical development by providing numerous options to companies of varying sizes and financial resources and also create multiple niches which could accommodate multiple vaccines in the market place. Given all that has been learned about S. aureus immunopathogenesis and vaccinology in the last decade, there is reason for considerable optimism that one or more S. aureus vaccines will become available for clinical use in the coming decade.
References
Sigurdsson AF, Gudmundsson S (1989) The etiology of bacterial cellulitis as determined by fine-needle aspiration. Scand J Infect Dis 21:537–542
Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN et al (2001) Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997–1999. Clin Infect Dis 32(Suppl 2):S114–S132
Carratala J, Roson B, Fernandez-Sabe N, Shaw E, del Rio O, Rivera A et al (2003) Factors associated with complications and mortality in adult patients hospitalized for infectious cellulitis. Eur J Clin Microbiol Infect Dis 22:151–157
Brook I, Frazier EH (1995) Clinical features and aerobic and anaerobic microbiological characteristics of cellulitis. Arch Surg 130:786–792
Fowler VG Jr, Miro JM, Hoen B, Cabell CH, Abrutyn E, Rubinstein E et al (2005) Staphylococcus aureus endocarditis: a consequence of medical progress. Jama 293:3012–3021
Wisplinghoff H, Seifert H, Tallent SM, Bischoff T, Wenzel RP, Edmond MB (2003) Nosocomial bloodstream infections in pediatric patients in United States hospitals: epidemiology, clinical features and susceptibilities. Pediatr Infect Dis J 22:686–691
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317
Moreillon P, Que Y-A, Glauser MP (2005) Staphylococcus aureus (including staphylococcal toxic shock). In: Mandell GL, Bennett JE, Dolin R (eds) Principles and practice of infectious diseases, 6th edn. Elsevier, Philadelphia, pp 2321–2351
Hoen B, Alla F, Selton-Suty C, Beguinot I, Bouvet A, Briancon S et al (2002) Changing profile of infective endocarditis: results of a 1-year survey in France. JAMA 288:75–81
Frimodt-Moller N, Espersen F, Skinhoj P, Rosdahl VT (1997) Epidemiology of Staphylococcus aureus bacteremia in Denmark from 1957 to 1990. Clin Microbiol Infect 3:297–305
Laupland KB, Church DL, Mucenski M, Sutherland LR, Davies HD (2003) Population-based study of the epidemiology of and the risk factors for invasive Staphylococcus aureus infections. J Infect Dis 187:1452–1459
Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S et al (2007) Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298:1763–1771
Chambers HF (2005) Community-associated MRSA—resistance and virulence converge. N Engl J Med 352:1485–1487
Jensen AG, Wachmann CH, Poulsen KB, Espersen F, Scheibel J, Skinhoj P et al (1999) Risk factors for hospital-acquired Staphylococcus aureus bacteremia. Arch Intern Med 159:1437–1444
Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA et al (2005) Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med 352:1436–1444
From the Centers for Disease Control and Prevention (1999) Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997–1999. JAMA 282:1123–1125
Fergie JE, Purcell K (2001) Community-acquired methicillin-resistant Staphylococcus aureus infections in south Texas children. Pediatr Infect Dis J 20:860–863
Faden H, Ferguson S (2001) Community-acquired methicillin-resistant Staphylococcus aureus and intrafamily spread of pustular disease. Pediatr Infect Dis J 20:554–555
Chambers HF (2001) The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis 7:178–182
Bancroft E, Kilgore G, Jones A, Yasuda L, Lee NE, Ruane P, et al. (2003) Four outbreaks of community-associated methicillin-resistant Staphylococcus aureus in Los Angeles County. The 41st Annual Meeting of the Infectious Disease Society of America, San Diego, CA, October 2003
Sattler CA, Mason EO Jr, Kaplan SL (2002) Prospective comparison of risk factors and demographic and clinical characteristics of community-acquired, methicillin-resistant versus methicillin-susceptible Staphylococcus aureus infection in children. Pediatr Infect Dis J 21:910–917
Eady EA, Cove JH (2003) Staphylococcal resistance revisited: community-acquired methicillin resistant Staphylococcus aureus—an emerging problem for the management of skin and soft tissue infections. Curr Opin Infect Dis 16:103–124
Moran GJ, Amii RN, Abrahamian FM, Talan DA (2005) Methicillin-resistant Staphylococcus aureus in community-acquired skin infections. Emerg Infect Dis 11:928–930
Plotkin SA (2008) Vaccines: correlates of vaccine-induced immunity. Clin Infect Dis 47:401–409
Rich RR, Fleisher TA, Shearer WT, Kotzin BL, Schroeder HWJ (2001) Clinical immunology: principles and practice, 2nd edn. Mosby, New York
Espersen F, Hedstrom SA (1984) Recurrent staphylococcal furunculosis: antibody response against Staphylococcus aureus. Scand J Infect Dis 16:413–414
Monteil MA, Kaniuk AS, Hobbs JR (1990) Staphylococcal opsonization and anti-Staphylococcus aureus IgG subclass antibodies in patients with severe or recurrent S. aureus infections. FEMS Microbiol Immunol 2:259–262
Hermos CR, Yoong P, Pier GB (2010) High levels of antibody to Panton–Valentine leukocidin are not associated with resistance to Staphylococcus aureus-associated skin and soft-tissue infection. Clin Infect Dis 51:1138–1146
Verkaik NJ, Boelens HA, de Vogel CP, Tavakol M, Bode LG, Verbrugh HA et al (2010) Heterogeneity of the humoral immune response following Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis 29:509–518
Dryla A, Prustomersky S, Gelbmann D, Hanner M, Bettinger E, Kocsis B et al (2005) Comparison of antibody repertoires against Staphylococcus aureus in healthy individuals and in acutely infected patients. Clin Diagn Lab Immunol 12:387–398
Daum RS (2007) Clinical practice. Skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. N Engl J Med 357:380–390
Stryjewski ME, Chambers HF (2008) Skin and soft-tissue infections caused by community-acquired methicillin-resistant Staphylococcus aureus. Clin Infect Dis 46(Suppl 5):S368–S377
Schmitz GR, Bruner D, Pitotti R, Olderog C, Livengood T, Williams J et al (2010) Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection. Ann Emerg Med 56:283–287
Del Giudice P, Bes M, Hubiche T, Roudiere L, Blanc V, Lina G et al (2011) Clinical manifestations and outcome of skin infections caused by the community-acquired methicillin-resistant Staphylococcus aureus clone ST80-IV. J Eur Acad Dermatol Venereol 25:164–169
Sreeramoju P, Porbandarwalla NS, Arango J, Latham K, Dent DL, Stewart RM et al (2011) Recurrent skin and soft tissue infections due to methicillin-resistant Staphylococcus aureus requiring operative debridement. Am J Surg 201:216–220
David MZ, Mennella C, Mansour M, Boyle-Vavra S, Daum RS (2008) Predominance of methicillin-resistant Staphylococcus aureus among pathogens causing skin and soft tissue infections in a large urban jail: risk factors and recurrence rates. J Clin Microbiol 46:3222–3227
Davis SL, Perri MB, Donabedian SM, Manierski C, Singh A, Vager D et al (2007) Epidemiology and outcomes of community-associated methicillin-resistant Staphylococcus aureus infection. J Clin Microbiol 45:1705–1711
Shastry L, Rahimian J, Lascher S (2007) Community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections in men who have sex with men in New York City. Arch Intern Med 167:854–857
Rahimian J, Khan R, LaScalea KA (2007) Does nasal colonization or mupirocin treatment affect recurrence of methicillin-resistant Staphylococcus aureus skin and skin structure infections? Infect Control Hosp Epidemiol 28:1415–1416
Kim HK, Cheng AG, Kim HY, Missiakas DM, Schneewind O (2010) Nontoxigenic protein A vaccine for methicillin-resistant Staphylococcus aureus infections in mice. J Exp Med 207:1863–1870
Foster TJ (2005) Immune evasion by staphylococci. Nat Rev Microbiol 3:948–958
Crum-Cianflone NF, Burgi AA, Hale BR (2007) Increasing rates of community-acquired methicillin-resistant Staphylococcus aureus infections among HIV-infected persons. Int J STD AIDS 18:521–526
Graber CJ, Jacobson MA, Perdreau-Remington F, Chambers HF, Diep BA (2008) Recurrence of skin and soft tissue infection caused by methicillin-resistant Staphylococcus aureus in a HIV primary care clinic. J Acquir Immune Defic Syndr 49:231–233
Skiest D, Brown K, Hester J, Moore T, Crosby C, Mussa HR et al (2006) Community-onset methicillin-resistant Staphylococcus aureus in an urban HIV clinic. HIV Med 7:361–368
Milner JD, Brenchley JM, Laurence A, Freeman AF, Hill BJ, Elias KM et al (2008) Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature 452:773–776
Ma CS, Chew GY, Simpson N, Priyadarshi A, Wong M, Grimbacher B et al (2008) Deficiency of Th17 cells in hyper IgE syndrome due to mutations in STAT3. J Exp Med 205:1551–1557
Heimall J, Freeman A, Holland SM (2010) Pathogenesis of hyper IgE syndrome. Clin Rev Allergy Immunol 38:32–38
Minegishi Y (2009) Hyper-IgE syndrome. Curr Opin Immunol 21:487–492
Woellner C, Gertz EM, Schaffer AA, Lagos M, Perro M, Glocker EO et al (2010) Mutations in STAT3 and diagnostic guidelines for hyper-IgE syndrome. J Allergy Clin Immunol 125:424–432.e8
Schroeder HWJ (2001) Primary antibody deficiencies. In: Rich RR, Fleisher TA, Shearer WT, Kotzin BL, Schroeder HWJ (eds) Clinical immunology: principles and practice, 2nd edn. Mosby, New York, pp 34.31–34.15
Fried AJ, Bonilla FA (2009) Pathogenesis, diagnosis, and management of primary antibody deficiencies and infections. Clin Microbiol Rev 22:396–414
Wood P (2009) Primary antibody deficiencies: recognition, clinical diagnosis and referral of patients. Clin Med 9:595–599
Stockinger B, Veldhoen M (2007) Differentiation and function of Th17 T cells. Curr Opin Immunol 19:281–286
Romagnani S, Maggi E, Liotta F, Cosmi L, Annunziato F (2009) Properties and origin of human Th17 cells. Mol Immunol 47:3–7
Spellberg B, Ibrahim AS, Yeaman M, Lin L, Fu Y, Avanesian V et al (2008) The anti-fungal rAls3p-N vaccine protects mice against the bacterium Staphylococcus aureus. Infect Immun 76:4574–4580
Lin L, Ibrahim AS, Avanesian V, Xu X, Farber J, Fu Y, et al. (2009) Th17 cells are not required for host defense against murine disseminated candidiasis, but are required for vaccine-mediated protection. Abstract 951, 96th Annual Meeting of the American Association of Immunology, Seattle, WA
Lin L, Ibrahim AS, Xu X, Farber JM, Avanesian V, Baquir B et al (2009) Th1–Th17 cells mediate protective adaptive immunity against Staphylococcus aureus and Candida albicans infection in mice. PLoS Pathog 5:e1000703
Ishigame H, Kakuta S, Nagai T, Kadoki M, Nambu A, Komiyama Y et al (2009) Differential roles of interleukin-17A and -17F in host defense against mucoepithelial bacterial infection and allergic responses. Immunity 30:108–119
Robbins JB, Schneerson R, Horwith G, Naso R, Fattom A (2004) Staphylococcus aureus types 5 and 8 capsular polysaccharide–protein conjugate vaccines. Am Heart J 147:593–598
Fattom A, Fuller S, Propst M, Winston S, Muenz L, He D et al (2004) Safety and immunogenicity of a booster dose of Staphylococcus aureus types 5 and 8 capsular polysaccharide conjugate vaccine (StaphVAX) in hemodialysis patients. Vaccine 23:656–663
Shinefield H, Black S, Fattom A, Horwith G, Rasgon S, Ordonez J et al (2002) Use of a Staphylococcus aureus conjugate vaccine in patients receiving hemodialysis. N Engl J Med 346:491–496
Press Release (2005) Nabi Biopharmaceuticals announces results of StaphVAX(R) confirmatory phase III clinical trial. PRNewswire-FirstCall. http://www.prnewswire.com/cgi-bin/stories.pl?ACCT=104&STORY=/www/story/11-01-2005/0004205028&EDATE=. Accessed 4 April 2006
Montgomery CP, Boyle-Vavra S, Adem PV, Lee JC, Husain AN, Clasen J et al (2008) Comparison of virulence in community-associated methicillin-resistant Staphylococcus aureus pulsotypes USA300 and USA400 in a rat model of pneumonia. J Infect Dis 198:561–570
Verdier I, Durand G, Bes M, Taylor KL, Lina G, Vandenesch F et al (2007) Identification of the capsular polysaccharides in Staphylococcus aureus clinical isolates by PCR and agglutination tests. J Clin Microbiol 45:725–729
Sutter DE, Summers AM, Keys CE, Taylor KL, Frasch CE, Braun LE et al (2011) Capsular serotype of Staphylococcus aureus in the era of community-acquired MRSA. FEMS Immunol Med Microbiol 63:16–24
Inhibitex Inc. (2005) Inhibitex reports favorable results from Aurexis phase II trial for the treatment of staph bloodstream infections. Inhibitex Inc.
PR Newswire (2006) Inhibitex reports top-line results in phase III study of Veronate(R)
van den Berg S, Bowden MG, Bosma T, Buist G, van Dijl JM, van Wamel WJ et al (2011) A multiplex assay for the quantification of antibody responses in Staphylococcus aureus infections in mice. J Immunol Methods 365:142–148
Kennedy AD, Bubeck Wardenburg J, Gardner DJ, Long D, Whitney AR, Braughton KR et al (2010) Targeting of alpha-hemolysin by active or passive immunization decreases severity of USA300 skin infection in a mouse model. J Infect Dis 202:1050–1058
Ragle BE, Bubeck Wardenburg J (2009) Anti-alpha-hemolysin monoclonal antibodies mediate protection against Staphylococcus aureus pneumonia. Infect Immun 77:2712–2718
Bubeck Wardenburg J, Schneewind O (2008) Vaccine protection against Staphylococcus aureus pneumonia. J Exp Med 205:287–294
Brown EL, Dumitrescu O, Thomas D, Badiou C, Koers EM, Choudhury P et al (2009) The Panton–Valentine leukocidin vaccine protects mice against lung and skin infections caused by Staphylococcus aureus USA300. Clin Microbiol Infect 15:156–164
Schaffer AC, Solinga RM, Cocchiaro J, Portoles M, Kiser KB, Risley A et al (2006) Immunization with Staphylococcus aureus clumping factor B, a major determinant in nasal carriage, reduces nasal colonization in a murine model. Infect Immun 74:2145–2153
Arrecubieta C, Matsunaga I, Asai T, Naka Y, Deng MC, Lowy FD (2008) Vaccination with clumping factor A and fibronectin binding protein A to prevent Staphylococcus aureus infection of an aortic patch in mice. J Infect Dis 198:571–575
Narita K, Hu DL, Mori F, Wakabayashi K, Iwakura Y, Nakane A (2010) Role of interleukin-17A in cell-mediated protection against Staphylococcus aureus infection in mice immunized with the fibrinogen-binding domain of clumping factor A. Infect Immun 78:4234–4242
Gong R, Hu C, Xu H, Guo A, Chen H, Zhang G et al (2010) Evaluation of clumping factor A binding region A in a subunit vaccine against Staphylococcus aureus-induced mastitis in mice. Clin Vaccine Immunol 17:1746–1752
Gaudreau MC, Lacasse P, Talbot BG (2007) Protective immune responses to a multi-gene DNA vaccine against Staphylococcus aureus. Vaccine 25:814–824
Brouillette E, Lacasse P, Shkreta L, Belanger J, Grondin G, Diarra MS et al (2002) DNA immunization against the clumping factor A (ClfA) of Staphylococcus aureus. Vaccine 20:2348–2357
Glowalla E, Tosetti B, Kronke M, Krut O (2009) Proteomics-based identification of anchorless cell wall proteins as vaccine candidates against Staphylococcus aureus. Infect Immun 77:2719–2729
Stranger-Jones YK, Bae T, Schneewind O (2006) Vaccine assembly from surface proteins of Staphylococcus aureus. Proc Natl Acad Sci U S A 103:16942–16947
Projan SJ, Nesin M, Dunman PM (2006) Staphylococcal vaccines and immunotherapy: to dream the impossible dream? Curr Opin Pharmacol 6:473–479
Schaffer AC, Lee JC (2009) Staphylococcal vaccines and immunotherapies. Infect Dis Clin North Am 23:153–171
Mazmanian SK, Skaar EP, Gaspar AH, Humayun M, Gornicki P, Jelenska J et al (2003) Passage of heme-iron across the envelope of Staphylococcus aureus. Science 299:906–909
Skaar EP, Schneewind O (2004) Iron-regulated surface determinants (Isd) of Staphylococcus aureus: stealing iron from heme. Microbes Infect 6:390–397
Skaar EP, Humayun M, Bae T, DeBord KL, Schneewind O (2004) Iron-source preference of Staphylococcus aureus infections. Science 305:1626–1628
Park RY, Sun HY, Choi MH, Bai YH, Shin SH (2005) Staphylococcus aureus siderophore-mediated iron-acquisition system plays a dominant and essential role in the utilization of transferrin-bound iron. J Microbiol 43:183–190
Maresso AW, Schneewind O (2006) Iron acquisition and transport in Staphylococcus aureus. Biometals 19:193–203
Trivier D, Davril M, Houdret N, Courcol RJ (1995) Influence of iron depletion on growth kinetics, siderophore production, and protein expression of Staphylococcus aureus. FEMS Microbiol Lett 127:195–199
Aguila A, Herrera AG, Morrison D, Cosgrove B, Perojo A, Montesinos I et al (2001) Bacteriostatic activity of human lactoferrin against Staphylococcus aureus is a function of its iron-binding properties and is not influenced by antibiotic resistance. FEMS Immunol Med Microbiol 31:145–152
Kuklin NA, Clark DJ, Secore S, Cook J, Cope LD, McNeely T et al (2006) A novel Staphylococcus aureus vaccine: iron surface determinant B induces rapid antibody responses in rhesus macaques and specific increased survival in a murine S. aureus sepsis model. Infect Immun 74:2215–2223
Etz H, Minh DB, Henics T, Dryla A, Winkler B, Triska C et al (2002) Identification of in vivo expressed vaccine candidate antigens from Staphylococcus aureus. Proc Natl Acad Sci USA 99:6573–6578
Ebert T, Smith S, Pancari G, Clark D, Hampton R, Secore S et al (2010) A fully human monoclonal antibody to Staphylococcus aureus iron regulated surface determinant B (IsdB) with functional activity in vitro and in vivo. Hum Antibodies 19:113–128
Harro C, Betts R, Orenstein W, Kwak EJ, Greenberg HE, Onorato MT et al (2010) Safety and immunogenicity of a novel Staphylococcus aureus vaccine: results from the first study of the vaccine dose range in humans. Clin Vaccine Immunol 17:1868–1874
Lin L, Ibrahim AS, Baquir B, Avanesian V, Fu Y, Spellberg B (2009) Immunological surrogate marker of rAls3p-N vaccine-induced protection against Staphylococcus aureus. FEMS Immunol Med Microbiol 55:293–295
Pachl J, Svoboda P, Jacobs F, Vandewoude K, van der Hoven B, Spronk P et al (2006) A randomized, blinded, multicenter trial of lipid-associated amphotericin B alone versus in combination with an antibody-based inhibitor of heat shock protein 90 in patients with invasive candidiasis. Clin Infect Dis 42:1404–1413
Torosantucci A, Bromuro C, Chiani P, De Bernardis F, Berti F, Galli C et al (2005) A novel glyco-conjugate vaccine against fungal pathogens. J Exp Med 202:597–606
Torosantucci A, Chiani P, Bromuro C, De Bernardis F, Palma AS, Liu Y et al (2009) Protection by anti-beta-glucan antibodies is associated with restricted beta-1,3 glucan binding specificity and inhibition of fungal growth and adherence. PLoS ONE 4:e5392
Spellberg B, Boucher H, Bradley J, Das A, Talbot G (2011) To treat or not to treat: adjunctive antibiotics for uncomplicated abscesses. Ann Emerg Med 57:183–185
Cloran FJ (2006) Cutaneous infections with community-acquired MRSA in aviators. Aviat Space Environ Med 77:1271–1274
Ellis MW, Hospenthal DR, Dooley DP, Gray PJ, Murray CK (2004) Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin Infect Dis 39:971–979
LaMar JE, Carr RB, Zinderman C, McDonald K (2003) Sentinel cases of community-acquired methicillin-resistant Staphylococcus aureus onboard a naval ship. Mil Med 168:135–138
Morrison-Rodriguez SM, Pacha LA, Patrick JE, Jordan NN (2010) Community-associated methicillin-resistant Staphylococcus aureus infections at an Army training installation. Epidemiol Infect 138:721–729
Pagac BB, Reiland RW, Bolesh DT, Swanson DL (2006) Skin lesions in barracks: consider community-acquired methicillin-resistant Staphylococcus aureus infection instead of spider bites. Mil Med 171:830–832
Roberts SS, Kazragis RJ (2009) Methicillin-resistant Staphylococcus aureus infections in U.S. service members deployed to Iraq. Mil Med 174:408–411
Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB et al (2006) Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 355:666–674
Maree CL, Eells SJ, Tan J, Bancroft EA, Malek M, Harawa NT et al (2010) Risk factors for infection and colonization with community-associated methicillin-resistant Staphylococcus aureus in the Los Angeles County jail: a case–control study. Clin Infect Dis 51:1248–1257
Centers for Disease Control and Prevention (2003) Outbreaks of community-associated methicillin-resistant Staphylococcus aureus skin infections—Los Angeles County, California, 2002–2003. MMWR Morb Mortal Wkly Rep 52:88
Stryjewski ME, Kanafani ZA, Chu VH, Pappas PA, Harding T, Drew LA et al (2009) Staphylococcus aureus bacteremia among patients with health care-associated fever. Am J Med 122:281–289.e2
Lucero CA, Hageman J, Zell ER, Bulens S, Nadle J, Petit S et al (2009) Evaluating the potential public health impact of a Staphylococcus aureus vaccine through use of population-based surveillance for invasive methicillin-resistant S. aureus disease in the United States. Vaccine 27:5061–5068
Liu C, Graber CJ, Karr M, Diep BA, Basuino L, Schwartz BS et al (2008) A population-based study of the incidence and molecular epidemiology of methicillin-resistant Staphylococcus aureus disease in San Francisco, 2004–2005. Clin Infect Dis 46:1637–1646
King JC Jr, Vink PE, Farley JJ, Parks M, Smilie M, Madore D et al (1996) Comparison of the safety and immunogenicity of a pneumococcal conjugate with a licensed polysaccharide vaccine in human immunodeficiency virus and non-human immunodeficiency virus-infected children. Pediatr Infect Dis J 15:192–196
Kroon FP, van Dissel JT, Ravensbergen E, Nibbering PH, van Furth R (1999) Impaired antibody response after immunization of HIV-infected individuals with the polysaccharide vaccine against Salmonella typhi (Typhim-Vi). Vaccine 17:2941–2945
Souza D, dos Santos S, Lopes MH, Simonsen V, Caiaffa Filho HH (2004) Haemophilus influenzae type b immunization in adults infected with the human immunodeficiency virus. AIDS Res Hum Retroviruses 20:493–496
Rutstein RM, Rudy BJ, Cnaan A (1996) Response of human immunodeficiency virus-exposed and -infected infants to Haemophilus influenzae type b conjugate vaccine. Arch Pediatr Adolesc Med 150:838–841
Chokephaibulkit K, Phongsamart W, Vanprapar N, Chotpitayasunondh T, Chearskul S (2004) Catch-up vaccination against Haemophilus influenzae type b in human immunodeficiency virus-infected Thai children older than 2 years old. Vaccine 22:2018–2022
Dockrell DH, Poland GA, Steckelberg JM, Wollan PC, Strickland SR, Pomeroy C (1999) Immunogenicity of three Haemophilus influenzae type b protein conjugate vaccines in HIV seropositive adults and analysis of predictors of vaccine response. Vaccine 17:2779–2785
Read JS, Frasch CE, Rich K, Fitzgerald GA, Clemens JD, Pitt J et al (1998) The immunogenicity of Haemophilus influenzae type b conjugate vaccines in children born to human immunodeficiency virus-infected women. Women and Infants Transmission Study Group. Pediatr Infect Dis J 17:391–397
Levin MJ, Gershon AA, Weinberg A, Blanchard S, Nowak B, Palumbo P et al (2001) Immunization of HIV-infected children with varicella vaccine. J Pediatr 139:305–310
Tasker SA, Schnepf GA, Lim M, Caraviello HE, Armstrong A, Bavaro M et al (2004) Unintended smallpox vaccination of HIV-1-infected individuals in the United States military. Clin Infect Dis 38:1320–1322
Tedaldi EM, Baker RK, Moorman AC, Wood KC, Fuhrer J, McCabe RE et al (2004) Hepatitis A and B vaccination practices for ambulatory patients infected with HIV. Clin Infect Dis 38:1478–1484
Kemper CA, Haubrich R, Frank I, Dubin G, Buscarino C, McCutchan JA et al (2003) Safety and immunogenicity of hepatitis A vaccine in human immunodeficiency virus-infected patients: a double-blind, randomized, placebo-controlled trial. J Infect Dis 187:1327–1331
Madhi SA, Petersen K, Khoosal M, Huebner RE, Mbelle N, Mothupi R et al (2002) Reduced effectiveness of Haemophilus influenzae type b conjugate vaccine in children with a high prevalence of human immunodeficiency virus type 1 infection. Pediatr Infect Dis J 21:315–321
Klugman KP, Madhi SA, Huebner RE, Kohberger R, Mbelle N, Pierce N (2003) A trial of a 9-valent pneumococcal conjugate vaccine in children with and those without HIV infection. N Engl J Med 349:1341–1348
Guerrero M, Kruger S, Saitoh A, Sorvillo F, Cheng KJ, French C et al (1999) Pneumonia in HIV-infected patients: a case–control survey of factors involved in risk and prevention. Aids 13:1971–1975
Greenwood B (2005) Interpreting vaccine efficacy. Clin Infect Dis 40:1519–1520
Madhi SA, Kuwanda L, Cutland C, Klugman KP (2005) The impact of a 9-valent pneumococcal conjugate vaccine on the public health burden of pneumonia in HIV-infected and -uninfected children. Clin Infect Dis 40:1511–1518
Sinsalo M, Aittoniemi J, Kayhty H, Vilpo J (2002) Haemophilus influenzae type b (Hib) antibody concentrations and vaccination responses in patients with chronic lymphocytic leukaemia: predicting factors for response. Leuk Lymphoma 43:1967–1969
Feldman S, Gigliotti F, Shenep JL, Roberson PK, Lott L (1990) Risk of Haemophilus influenzae type b disease in children with cancer and response of immunocompromised leukemic children to a conjugate vaccine. J Infect Dis 161:926–931
Nordoy T, Aaberge IS, Husebekk A, Samdal HH, Steinert S, Melby H et al (2002) Cancer patients undergoing chemotherapy show adequate serological response to vaccinations against influenza virus and Streptococcus pneumoniae. Med Oncol 19:71–78
Leung TF, Li CK, Hung EC, Chan PK, Mo CW, Wong RP et al (2004) Immunogenicity of a two-dose regime of varicella vaccine in children with cancers. Eur J Haematol 72:353–357
Somjee S, Pai S, Parikh P, Banavali S, Kelkar R, Advani S (2002) Passive active prophylaxis against hepatitis B in children with acute lymphoblastic leukemia. Leuk Res 26:989–992
Arrowood JR, Hayney MS (2002) Immunization recommendations for adults with cancer. Ann Pharmacother 36:1219–1229
Acknowledgments
This work was supported by PHS R01 AI072052.
Disclosures
BS owns shares in NovaDigm Therapeutics Inc., which is developing vaccine technologies against S. aureus. In the last 12 months, he has served as a site investigator for a Cubist antibacterial clinical trial of S. aureus infection. He has also consulted for Pfizer, The Medicines Company, Achaogen, Trius, Glaxo Smith Kline, Eisai, Anacor, Zimek, Theravance, and Meiji.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is published as part of the Special Issue on Immunopathology of Staphylococcal Infections [34:3].
Rights and permissions
About this article
Cite this article
Spellberg, B., Daum, R. Development of a vaccine against Staphylococcus aureus . Semin Immunopathol 34, 335–348 (2012). https://doi.org/10.1007/s00281-011-0293-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-011-0293-5