Abstract
Purpose
There are no reports on the use of neoadjuvant chemotherapy (NAC) in non-squamous cell cervical carcinoma. We examined the effectiveness and safety of paclitaxel/carboplatin (TC) and docetaxel/carboplatin (DC).
Methods
Stage Ib2 to IIb disease was present in 23 patients scheduled for radical hysterectomy. We administered 1–3 courses of either the TC or the DC regimen. Anti-tumor effects were found superior by Response Evaluation Criteria in Solid Tumors. Safety was assessed with National Cancer Institute Common Terminology Criteria for Adverse Events.
Results
Median age was 50 years (range 32–63 years), with stage Ib2 in 6 cases (26.1 %) and IIb in 17 cases (73.9 %). Complete response was achieved in 5 cases (21.7 %), partial response in 13 (56.5 %), stable disease in 5 (21.7 %); the response rate was 78.3 %, and surgery completion rate was 78.3 %. Leukopenia or neutropenia ≥grade 3 was seen in 12 (52.2 %) and 21 (91.3 %) cases, respectively, with grade 3 febrile neutropenia in 2 cases (8.7 %) and no anemia or thrombocytopenia ≥grade 3. Median progression-free survival was 26 months (95 % Cl, 13.5–38.5 months); median overall survival was 35 months (95 % Cl, 20.9–49.1 months).
Conclusion
NAC for non-squamous cell cervical carcinoma showed potent anti-tumor effects and manageable adverse events.
Similar content being viewed by others
Introduction
The methods used to treat bulky stage Ib2 to IIb cervical cancers differ between Japan and Western countries. In Western countries, concurrent chemoradiation therapy (CCRT) has been recommended as a standard treatment for such tumors, based on the results of multiple large-scale randomized trials and meta-analyses [1–7]. In Japan, Korea, and Italy, among other countries, the neoadjuvant chemotherapy (NAC) approach has been introduced to clinical practice and is extensively utilized [8, 9]. An Italian phase III, controlled study involving patients with locally advanced stage Ib2 to IIb squamous cell carcinoma of the cervix showed that NAC prior to radical hysterectomy improves patient outcomes compared with conventional radiation therapy alone [10].
There are no previous reports on the use of NAC for bulky non-squamous cell carcinoma of the cervix. We present the results of an ongoing pilot study on its efficacy and safety.
Subjects and methods
Subjects
We studied 23 patients with locally advanced non-squamous cell carcinoma of the uterine cervix (clinical stage Ib2 to IIb) between January 2002 and September 2011. All patients were scheduled to undergo radical hysterectomy and gave informed consent for this study.
Inclusion criteria
The following inclusion criteria were employed: (1) histologically verified non-squamous cell carcinoma of the uterine cervix; (2) locally advanced disease, stage Ib2–IIb; (3) between 20 and 74 years of age; (4) Eastern Cooperative Oncology Group performance status 0–2; (5) no prior treatment; (6) presence of a measurable bulky mass in the uterine cervix on magnetic resonance imaging (MRI); (7) hematologic and biochemical findings within the following parameters, WBC count ≥4,000/mm3, neutrophil count ≥2,000/mm3, platelet count ≥100,000/mm3, hemoglobin ≥10.0 g/dL, AST and ALT levels ≤2 times the upper limit of normal reference range, serum total bilirubin level ≤1.5 mg/dL, serum creatinine ≤1.5 mg/dL, and creatinine clearance ≥60 mL/min; (8) life expectancy ≥6 months; and (9) written informed consent personally given by the subject.
Exclusion criteria
Exclusion criteria were as follows: (1) overt infection; (2) serious complication(s), for example, cardiac disease, poorly controlled diabetes mellitus, malignant hypertension, bleeding tendency; (3) multiple active cancers; (4) interstitial pneumonia or pulmonary fibrosis; (5) pulmonary effusions; (6) history of unstable angina or myocardial infarction within 6 months after registration, or a concurrent serious cardiac arrhythmia requiring treatment; (7) contraindications to treatment with paclitaxel, docetaxel, or carboplatin; (8) intestinal paralysis or ileus; (9) pregnancy, breast-feeding, or desire for future pregnancy; (10) history of serious drug hypersensitivity or drug allergy; and (11) judged unsafe for participation by the attending physician.
Medication administration and criteria for modification
Regimen
The choice of regimen was left to the attending physician. Paclitaxel/carboplatin (TC) therapy was administered to 4 patients and DC therapy to 19 patients. Courses of treatment were administered 21 days apart, with a intravenous paclitaxel dose of 175 mg/m2 or a docetaxel dose of 70 mg/m2 administered on Day 1, and intravenous carboplatin with area under the curve (AUC) 6 mg/mL per min also administered on Day 1. As a rule, maximum 3 courses of treatment were administered to each patient.
Criteria for initiating the second course of treatment
The second course was postponed by a maximum of 2 weeks when blood analysis performed within 2 days prior to the planned start did not satisfy the following criteria: (1) neutrophil count ≥1,000/mm3; (2) platelet count ≥75,000/mm3.
Carboplatin dose-reduction criteria
The carboplatin dose for the second course was reduced from AUC 6 mg/mL per min to AUC 5 mg/mL per min if the patient experienced grade 4 thrombocytopenia or grade 3 thrombocytopenia accompanied by bleeding. If signs of toxicity remained after this dose reduction, the third course of treatment was reduced to AUC 4.
Paclitaxel dose-reduction criteria
The paclitaxel dose for the second course was reduced from 175 to 135 mg/m2 in patients exhibiting grade 2 or higher severe peripheral nerve toxicity during the first course. If this grade of nerve toxicity persisted after the dose reduction, the paclitaxel dose for the third course was reduced to 110 mg/m2.
Docetaxel dose-reduction criteria
The docetaxel dose for the second course was reduced from 70 to 60 mg/m2 if the patient experienced grade 4 neutropenia lasting 7 days or longer or febrile neutropenia lasting 4 days or longer. If signs of toxicity remained after this dose reduction, the docetaxel dose for the third course was reduced to 50 mg/m2.
Supportive therapy
A granulocyte colony-stimulating factor (G-CSF) preparation was administered to patients who developed grade 4 neutropenia during the first course of NAC. These patients were permitted prophylactic G-CSF during the second and subsequent courses of NAC. Anti-emetics were used for the preventive purpose.
Primary treatment
Patients with stage Ib2–IIb cervical carcinoma underwent radical hysterectomy unless the tumor responded to preoperative treatment with progressive disease (PD), at which time the tumor was up-staged. In cases in which surgery was not possible, CCRT was adopted.
Postoperative therapy
Postoperative radiotherapy, postoperative chemotherapy, or CCRT was additionally administered in patients with a positive surgical margin at the vaginal stump, lymphadenopathy, invasion of the cardinal ligament, or evident invasion of the vasculature.
Outcome evaluation
The primary endpoint was anti-tumor response. Secondary endpoints comprised adverse events, the surgery completion rate, the progression-free survival (PFS) period, and the overall survival (OS) period. Hematologic tests and urinalysis were performed before the start of treatment and, as a rule, once weekly after starting treatment. Electrocardiograms and chest radiographs were obtained before the start and at the end of treatment.
Evaluation of anti-tumor response
Anti-tumor response was evaluated using Response Evaluation Criteria in Solid Tumors guidelines. The baseline MRI findings were compared with the findings at the conclusion of treatment. For our efficacy evaluation, we adopted the best rating, without incorporating the response period.
Evaluation of adverse events
Adverse events were evaluated employing the National Cancer Institute Common Terminology Criteria for Adverse Events, version 3.0.
Statistical analysis
Progression-free survival (PFS), defined as the time from the start of the study treatment to documented tumor progression or death, and overall survival (OS), defined as the time from the start of treatment to the date of death, were calculated by the Kaplan–Meier method. The statistical data were obtained using StatMate III.
Results
Background variables
The median age of the 23 patients was 50 years (range 32–63 years). The performance status was 0 in 18 patients (78.3 %), and in 5 patients, the performance status was 1 (21.7 %). The clinical stage was Ib2 in 6 cases (26.1 %) and IIb in 17 cases (73.9 %). The histological type was mucinous adenocarcinoma in 10 cases (43.5 %), endometrioid adenocarcinoma in 5 (21.7 %), clear cell adenocarcinoma in 1 (4.3 %), and adenosquamous carcinoma in 7 (30.4 %). One course of NAC was administered in 1 patient (4.3 %), 2 courses in 17 patients (73.9 %), and 3 courses in 5 patients (21.7 %). The regimens comprised TC therapy in 4 cases (17.4 %) and DC therapy in 19 cases (82.6 %) (Table 1).
Anti-tumor response
A complete response was noted in 5 cases (21.7 %), partial response in 13 (56.5 %), and stable disease in 5 (21.7 %), with a overall response rate of 78.3 %. In subgroup analysis, the overall response rate of TC therapy and DC therapy was 100 and 73.7 %, respectively (Table 2).
Adverse events
Grade 3 or higher severe leukopenia or neutropenia was seen in 12 (52.2 %) and 21 (91.3 %) cases, respectively. Grade 3 febrile neutropenia was noted in 2 cases (8.7 %). The G-CSF preparation was used in 13 (56.5 %) of the 23 patients; it was administered during 19 (38.8 %) of the 49 total cycles. The mean duration of G-CSF treatment during each course was 2.6 days. No patients experienced grade 3 or higher severe anemia or thrombocytopenia. The only sign of grade 3 or higher severe non-hematologic toxicity was nausea, seen in 1 case (4.3 %). No patients had signs of grade 2 or higher severe neurotoxicity (Table 3).
In 3 cases (13.0 %), the second course of treatment was postponed due to a low neutrophil count; in all 3 patients, the second course was initiated within 7 days of its scheduled time. Both patients (10.0 %) with grade 3 febrile neutropenia for 4 days or longer had received DC therapy prior to the development of this complication. In these 2 cases, doses were reduced for the second course of treatment: docetaxel from 70 to 60 mg/m2 and carboplatin from AUC 6 to AUC 5.
Surgery completion and adjuvant therapy
Radical hysterectomy after NAC was completed in 18 of the 23 patients, giving a surgery completion rate of 78.3 %. Adjuvant therapy after radical hysterectomy consisted of no treatment in 3 cases (13.0 %), radiotherapy in 2 cases (8.7 %), chemotherapy in 15 cases (65.2 %), and CCRT in 3 cases (13.0 %).
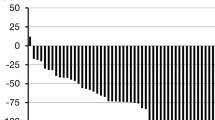
Survival
The median follow-up period was 31 months (range 9–90 months). The median progression-free survival period was 26 months (95 % Cl, 13.5–38.5 months), and the median overall survival period was 35 months (95 % Cl, 20.9–49.1 months) (Fig. 1). The 5 patients in whom surgery was not complete died of their primary disease within 35 months. Their median PFS and OS were 8 months (3–12 months) and 21 months (10–35 months), respectively.
Discussion
The incidence of non-squamous cell carcinoma of the uterine cervix has been steadily rising in Japan, currently accounting for approximately 10–15 % of all cervical cancer cases. Lymph node metastasis is more frequent with this disease, compared with invasive squamous cell carcinoma [11], and its sensitivity to radiotherapy and chemotherapy is considered to be lower [12]. Thus, squamous and non-squamous cell carcinomas must be analyzed separately. It is advisable and desirable to try new therapeutic strategies in non-squamous cell carcinoma, but the number of published studies involving this type of cervical cancer is small, with the number of cases analyzed in these reports also small. Thus, no high-level evidence regarding treatment has been obtained for this type of cervical carcinoma.
The response rates of adenocarcinoma are reportedly 20 % to cisplatin [13], 15 % to ifosfamide [14], 14 % to 5-fluorouracil [15], and 12 % to oral etoposide [16]; these response rates are lower than those of squamous cell carcinoma. According to Curtin et al. [17], however, the response rate of adenocarcinoma to paclitaxel is as high as 31 %, even when the agent is used independently. Docetaxel has also been attracting interest as an agent of NAC. Nagao et al. evaluated the efficacy of combined chemotherapy using a DC regimen (docetaxel 60 mg/m2 and carboplatin at AUC 6 on day 1, repeating the combination every 21 days) in 17 patients with advanced or recurrent cervical cancer, including 6 with adenocarcinoma and 1 with adenosquamous carcinoma. A partial response was obtained in 6 of the 7 cases with adenocarcinoma (including the case of adenosquamous carcinoma); the response rate was 86 % [18]. Considering these findings, we conducted a pilot study involving standard regimens of TC and DC, conventionally used for the treatment of ovarian cancer.
In the analysis of adverse events, severe neutropenia developed in 91.3 % of patients, but subsided in response to short-term treatment with a G-CSF preparation. During the first course of DC therapy, grade 3 febrile neutropenia developed in 2 cases; the dose of both agents was reduced for the next course of treatment. All signs, specific to taxanes, of peripheral neuropathy were grade 1 or less, allowing for continuation of treatment while preserving the quality of life of the individual patients. No serious adverse events occurred, and the response rate was 78.3 %. This study demonstrated a high response rate of bulky non-squamous cell carcinoma of the cervix to NAC using taxanes (paclitaxel or docetaxel) and carboplatin. It also demonstrated the safety of the medications in this regimen. The completion rate of radical hysterectomy, however, was only 78.3 %; thus, the treatment outcomes in this study were not satisfactory. Possible reasons for the low surgery completion rate include the rapid progression of non-squamous cell carcinoma, frequent invasion of tissues and organs surrounding the uterus, and frequent lymph node metastasis.
The treatment results and outcomes of all patients were shown in Table 4. Unfortunately, all patients with incomplete surgery ultimately experienced disease recurrence and died of their primary disease. Thus, the significance of NAC at present may not be to prolong survival time. Instead, in our view, NAC should be performed to fully optimize patients’ conditions with its antitumor effect in order to improve the chances of complete surgery. Further study is needed regarding the long-term outcomes of NAC.
References
Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, Fowler WC Jr, Clarke-Pearson DL, Liao SY (1999) Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol 17:1339–1348
Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, Rotman M, Gershenson DM, Mutch DG (1999) Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med 340:1137–1143
Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, Clarke-Pearson DL, Insalaco S (1999) Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med 340:1144–1153
Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL III, Walker JL, Gersell D (1999) Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage 1B cervical carcinoma. N Engl J Med 340:1154–1161
Peters WA III, Liu PY, Barrett RJ II, Stock RJ, Monk BJ, Berek JS, Souhami L, Grigsby P, Gordon W Jr, Alberts DS (2000) Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol 18:1606–1613
Thomas GM (1999) Improved treatment for cervical cancer—concurrent chemotherapy and radiotherapy. N Engl J Med 340:1198–1200
Green JA, Kirwan JM, Tierney JF, Symonds P, Fresco L, Collingwood M, Williams CJ (2001) Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systematic review and meta-analysis. Lancet 358:781–786
Sugiyama T, Nishida T, Kumagai S, Nishino S, Fujivoshi K, Okura N, Yakushiji M, Hiura M, Umesaki N (1999) Combination chemotherapy with irinotecan and cisplatin as neoadjuvant in locally advanced cervical cancer. Br J Cancer 81:95–98
Shoji T, Takatori E, Hatayama S, Omi H, Kagabu M, Honda T, Kumagai S, Morohara Y, Miura F, Yoshizaki A, Sugiyama T (2010) Phase II study of tri-weekly cisplatin and irinotecan as neoadjuvant chemotherapy for locally advanced cervical cancer. Oncol lett 1:515–519
Benedetti-Panici P, Greggi S, Colombo A, Amoroso M, Smaniotto D, Giannarelli D, Amunni G, Raspagliesi F, Zola P, Mangioni C, Landoni F (2002) Neoadjuvant chemotherapy and radical surgery versus exclusive radiotherapy in locally advanced squamous cell cervical cancer: results from the Italian multicenter randomized study. J Clin Oncol 20:179–188
Aoki Y, Sato T, Watanabe M, Sasaki M, Tsuneki I, Tanaka K (2001) Neoadjuvant chemotherapy using low-dose consecutive intraarterial infusion of cisplatin combined with 5FU for locally advanced cervical adenocarcinoma. Gynecol Oncol 83:496–499
Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, Favini G, Ferri L, Mangioni C (1997) Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet 350:535–540
Thigpen JT, Blessing JA, Fowler WC Jr, Hatch K (1986) Phase II trials of cisplatin and piperazinedione as single agents in the treatment of advanced or recurrent non-squamous cell carcinoma of the cervix: a Gynecologic Oncology Group Study. Cancer Treat Rep 70:1097–1100
Sutton GP, Blessing JA, DiSaia PJ, McGuire WP (1993) Phase II study of ifosfamide and mesna in nonsquamous carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol 49:48–50
Look KY, Blessing JA, Valea FA, McGehee R, Manetta A, Webster KD, Andersen WA (1997) Phase II trial of 5-fluorouracil and high-dose leucovorin in recurrent adenocarcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol 67:255–258
Rose PG, Blessing JA, Buller RE, Mannel RS, Webster KD (2003) Prolonged oral etoposide in recurrent or advanced non-squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol 89:267–270
Curtin JP, Blessing JA, Webster KD, Rose PG, Mayer AR, Fowler WC Jr, Malfetano JH, Alvarez RD (2001) Paclitaxel, an active agent in nonsquamous carcinomas of the uterine cervix: a Gynecologic Oncology Group Study. J Clin Oncol 19:1275–1278
Nagao S, Fujiwara K, Oda T, Ishikawa H, Koike H, Tanaka H, Kohno I (2005) Combination chemotherapy of docetaxel and carboplatin in advanced or recurrent cervix cancer. A pilot study. Gynecol Oncol 96:805–809
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Shoji, T., Takatori, E., Saito, T. et al. Neoadjuvant chemotherapy using platinum- and taxane-based regimens for bulky stage Ib2 to IIb non-squamous cell carcinoma of the uterine cervix. Cancer Chemother Pharmacol 71, 657–662 (2013). https://doi.org/10.1007/s00280-012-2052-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-012-2052-2