Abstract
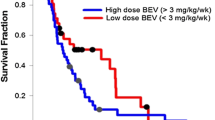
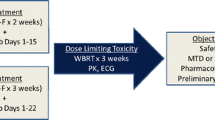
Laboratory and clinical studies support the concept that heparins, particularly the low molecular component, may serve as an inhibitor of angiogenesis, providing anti-neoplastic effects. Further, treatment with low molecular weight heparin (LMWH) may provide prophylaxis for thromboembolic events (TEE), in glioblastoma (GBM) patients. Dalteparin (5,000 U sub-Q daily) was given with and after conventional radiotherapy to newly diagnosed GBM patients. Forty-five patients were accrued between 5/02 and 9/04; 3 were ineligible. At time of progression, patients could continue dalteparin in addition to standard regimens. Pretreatment characteristics included: median age 61 (range 26–78); ECOG Performance status: 0 = 38%, 1 = 57%, 2 = 5%; gross total resection 45%. There were no grade 3/4 bleeding or thrombocytopenic events, and no TEE occurred while on dalteparin. Median time on dalteparin was 6.3 months, median time to progression was 3.9 months; median survival was 11.9 months. There was no significant improvement in survival when compared to the RTOG GBM database (with various radiation/drug doublets including BCNU) using recursive partitioning analysis. Historically the incidence of TEE in GBM patients is ∼30%. As this study suggests dalteparin reduces the incidence of TEE, and does not have significant overlapping toxicities with most other drugs; its testing in a combined modality approach with other medications may be warranted in future trials.

Similar content being viewed by others
Abbreviations
- ECOG:
-
Eastern Cooperative Oncology Group
- GBM :
-
Glioblastoma multiforme
- TEE:
-
Thromboembolic events
- LMWH:
-
Low molecular weight heparin
- RTOG:
-
Radiation Therapy Oncology Group
- KPS:
-
Karnofsky Performance Status
- RPA:
-
Recursive partitioning analysis
- DVT:
-
Deep vein thrombophlebitis
- MST:
-
Median survival time
References
Siragusa S, Cosmi B, Piovella F, Hirsh J, Ginsberg S (1996) Low-molecular-weight heparins and unfractionated heparin in the treatment of patients with acute venous thromboembolism: results of a meta-analysis. J Am Med 100:269–277
Folkman J, Langer R, Linhardt RJ, Haudenschild C, Taylor S (1983) Angiogenesis inhibition and tumor regression caused by heparin or a heparin fragment in the presence of cortisone. Science 221:719–725
Norrby K (1993) Heparin and angiogenesis: A low-molecular-weight fraction inhibits and a high-molecular-weight fraction stimulates angiogenesis systemically. Haemostasis 23(suppl 1):141–149
Bitan M, Mohsen M, Levi E, Wygoda MR, Miao H, Lider O, Svahn CM, Ekre HP, Ishai-Michaeli R, Bar-Shavit R, Vlodavsky I, Peretz T (1995) Structural requirements for inhibition of melanoma lung colonization by heparanase inhibiting species of heparin. Isr J Med Sci 31:106–118
Collen A, Smorenburg SM, Peters E, Lupu F, Koolwijk P, van Noordan C, van Hinsbergh VWM (2000) Unfractionated and low molecular weight heparin affect fibrin structure and angiogenisis in vitro. Cancer Res 60:6196–6200
Castellot Jr JJ, Choay J, Lormeau J, Petitou M, Sache E, Kamovsky MJ (1986) Structural determinants of the capacity of heparin to inhibit the proliferation of vascular smooth muscle cells. II. Evidence for a pentasaccharide sequence that contains a group. J Cell Biol 102:1979–1984
Teicher BA, Holden SA, Ara G, Dupuis NP, Liu F, Yuan J, Ikebe M, Kakeji Y (1995) Influence of an anti-angiogenic treatment on 9L gliosarcoma: oxygenation and response to cytotoxic therapy. Int J Cancer 61:732–737
Wachsberger P, Burd R, Dicker AP (2003) Tumor response to ionizing radiation combined with antiangiogenesis or vascular targeting agents. Clin Cancer Res 9:1957–1971
Dunn IF, Hesse O, Black PM (2004) Growth factors in glioma angiogenesis: FGFs, PDGF, EGF, and TGFs. J Neurooncol 50:121–137
Brisman R, Mendell J (1973) Thromboembolism and brain tumor. J Neurosurg 38:337–338
Kayser-Gatchalian MC, Kayser K (1975) Thrombosis and intracranial tumors. J Neurol 209:217–224
Sawaya R, Zuccarrello M, Elkalliny M, Nishiyama H (1992) Postoperative venous thromboembolism and brain tumors: Part I. Clinical profile. J Neurooncol 14:119–125
Sawaya R, Highsmith RF (1992) Postoperative venous thromboembolism and brain tumors: Part III. Biochemical profile. J Neurooncol 14:113–118
Nathanson M, Savitsky JP (1952) Platelet adhesive index studies in multiple sclerosis and other neurological disorders. Bull N Y Acad Med 28:462–468
Marras LC, Geerts WH, Perry JR (2000) The risk of venous thromboembolism is increased throughout the course of maligant glioma. Cancer 89:640–646
Millac P (1967) Platelet stickiness in patients with intracranial tumors. BMJ 4:25–26
Iberti TJ, Miller M, Abalos A, Fischer EP, Post KD, Benjamin E, Oropello JM, Wiltshire-Clement M, Rand JH (1994) Abnormal coagulation profile in brain tumor patients during surgery. Neurosurgery 34:389–395
Hamilton MG, Hull RD, Pineo GF (1994) Venous thromboembolism in neurosurgery and neurology patients: a review. Neurosurgery 34:280–296
Sawaya R, Highsmith RF (1988) Brain tumors and the fibrinolytic enzyme system. In: Kornblith PL, Walker MD (eds) Advances in neuro-oncology. Gutura, Mount Kisco, pp 103–157
Shlebak AA, Smith DB (1997) Incidence of objectively diagnosed thromboembolic disease in cancer patients undergoing cytotoxic chemotherapy and/or hormonal therapy. Cancer Chemother Pharmacol 39:462–466
Curran WJ Jr, Scott CB, Horton J, Nelson JS, Weinstein AS, Fishbach AJ, Chang CA, Rotman M Asbell SO, Krisch RE, Nelson DF (1993) Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst 85:704–710
Dixon DO, Simon R (1998) Sample size considerations for studies comparing survival curves using historical controls. J Clin Epidemiol 41:1209–1231
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Stupp R, Mason WP, Van Den Bent MJ, Weller M, Fisher B, Taphoorn M, Brandes AA, Cairncross G, Lacombe D, Mirimanoff RO (2004) Concomitant and adjuvant temozolomide and radiotherapy for newly diagnosed glioblastoma multiforme. Conclusive results of a randomized phase III trial by the EROTC Brain & RT groups and NICIC Clinical Trials Group. Proc Am Soc Clin Oncol 23:1 (abstract #2)
Rong Y, Durden DL, Van Meir EG, Brat DG (2006) Differential regulation of tissue factor expression by EGFR and EGFRvIII in GBM. Neurooncology 8:401
Seiferheld W, Mehta MP, Delrowe J,MacDonald D, Langer C, Scott C, Currqan WJ, Alfered Yung WK (2002) Five years of glioblastoma multiforme (GBM) phase II trials at the RTOG. Proc Am Soc Clin Oncol 21:71a (abstract #281)
Ruff RL, Posner JB (1983) Incidence and treatment of peripheral venous thrombosis in patients with glioma. Ann Neurol 13:334–336
Perry JR, Rogers L, Laperrier N, Julian J, Geerts W, Agnelli G, Malkin M, Sawaya R, Baker R, Levine M (2007) PRODIGE: a Phase III randomized placebo-controlled trial of thromboprophylaxis using dalteparin low molecular weight heparin (LMWH) in patients with newly diagnosed malignant glioma. J Clin Oncol 25:77s (Abstr 2011)
Acknowledgments
This study was conducted by the Eastern Cooperative Oncology Group (Robert L. Comis, M.D., Chair) and supported in part by Public Health Service Grants CA23318, CA66636, CA21115, CA21076, CA13650; RTOG U10 CA21661, CCOP U10 CA37422, and Stat U10 CA32115 grants from the National Cancer Institute, National Institutes of Health and the Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute, Kathleen Reader Memorial Research Fund. Dalteparin was supplied by Pfizer (formerly Pharmacia).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Robins, H.I., O’Neill, A., Gilbert, M. et al. Effect of dalteparin and radiation on survival and thromboembolic events in glioblastoma multiforme: a phase II ECOG trial. Cancer Chemother Pharmacol 62, 227–233 (2008). https://doi.org/10.1007/s00280-007-0596-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-007-0596-3