Abstract
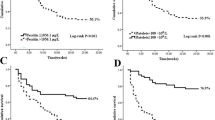
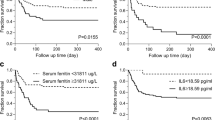
There has been no severity evaluation model for pediatric patients with hemophagocytic lymphohistiocytosis (HLH) that uses readily available parameters. This study aimed to develop a novel model for predicting the early mortality risk in pediatric patients with HLH using easily obtained parameters whatever etiologic subtype. Patients from one center were divided into training and validation sets for model derivation. The developed model was validated using an independent validation cohort from the second center. The prediction model with nomogram was developed based on logistic regression. The model performance underwent internal and external evaluation and validation using the area under the receiver operating characteristic curve (AUC), calibration curve with 1000 bootstrap resampling, and decision curve analysis (DCA). Model performance was compared with the most prevalent severity evaluation scores, including the PELOD-2, P-MODS, and pSOFA scores. The prediction model included nine variables: glutamic-pyruvic transaminase, albumin, globulin, myohemoglobin, creatine kinase, serum potassium, procalcitonin, serum ferritin, and interval between onset and diagnosis. The AUC of the model for predicting the 28-day mortality was 0.933 and 0.932 in the training and validation sets, respectively. The AUC values of the HScore, PELOD-2, P-MODS and pSOFA were 0.815, 0.745, 0.659 and 0.788, respectively. The DCA of the 28-day mortality prediction exhibited a greater net benefit than the HScore, PELOD-2, P-MODS and pSOFA. Subgroup analyses demonstrated good model performance across HLH subtypes. The novel mortality prediction model in this study can contribute to the rapid assessment of early mortality risk after diagnosis with readily available parameters.


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Griffin G, Shenoi S, Hughes GC (2020) Hemophagocytic lymphohistiocytosis: an update on pathogenesis, diagnosis, and therapy. Best Pract Res Clin Rheumatol 34(4):101515
Al-Samkari H, Berliner N (2018) Hemophagocytic lymphohistiocytosis. Annu Rev Pathol 13:27–49
Bergsten E, Horne A, Arico M, Astigarraga I, Egeler RM, Filipovich AH et al (2017) Confirmed efficacy of etoposide and dexamethasone in HLH treatment: long-term results of the cooperative HLH-2004 study. Blood 130(25):2728–2738
Canna SW, Marsh RA (2020) Pediatric hemophagocytic lymphohistiocytosis. Blood 135(16):1332–1343
Jordan MB, Allen CE, Greenberg J, Henry M, Hermiston ML, Kumar A et al (2019) Challenges in the diagnosis of hemophagocytic lymphohistiocytosis: Recommendations from the North American Consortium for Histiocytosis (NACHO). Pediatr Blood Cancer 66(11):e27929
Chen TY, Hsu MH, Kuo HC, Sheen JM, Cheng MC, Lin YJ (2021) Outcome analysis of pediatric hemophagocytic lymphohistiocytosis. J Formos Med Assoc 120(1 Pt 1):172–179
Gregory J, Greenberg J, Basu S (2019) Outcomes analysis of children diagnosed with hemophagocytic lymphohistiocytosis in the PICU. Pediatr Crit Care Med 20(4):e185–e190
Yin G, Man C, Huang J, Liao S, Gao X, Tian T et al (2020) The prognostic role of plasma fibrinogen in adult secondary hemophagocytic lymphohistiocytosis. Orphanet J Rare Dis 15(1):332
Lehmberg K, McClain KL, Janka GE, Allen CE (2014) Determination of an appropriate cut-off value for ferritin in the diagnosis of hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 61(11):2101–2103
Huang J, Yin G, Duan L, Tian T, Xu J, Wang J et al (2020) Prognostic value of blood-based inflammatory biomarkers in secondary hemophagocytic lymphohistiocytosis. J Clin Immunol 40(5):718–728
Tang Y, Xu X, Song H, Yang S, Shi S, Wei J et al (2008) Early diagnostic and prognostic significance of a specific Th1/Th2 cytokine pattern in children with haemophagocytic syndrome. Br J Haematol 143(1):84–91
Cui T, Wang J, Wang Z (2022) The outcome of induction therapy for EBV-related hemophagocytic lymphohistiocytosis: a model for risk stratification. Front Immunol 13:876415
Lu M, Xie Y, Guan X, Wang M, Zhu L, Zhang S et al (2021) Clinical analysis and a novel risk predictive nomogram for 155 adult patients with hemophagocytic lymphohistiocytosis. Ann Hematol 100(9):2181–2193
Yao S, Wang Y, Sun Y, Liu L, Zhang R, Fang J et al (2021) Epidemiological investigation of hemophagocytic lymphohistiocytosis in China. Orphanet J Rare Dis 16(1):342
Zhou YH, Han XR, Xia FQ, Poonit ND, Liu L (2022) Clinical features and prognostic factors of early outcome in pediatric hemophagocytic lymphohistiocytosis: a retrospective analysis of 227 cases. J Pediatr Hematol Oncol 44(1):e217–e222
Li X, Yan H, Zhang X, Huang J, Xiang ST, Yao Z et al (2020) Clinical profiles and risk factors of 7-day and 30-day mortality among 160 pediatric patients with hemophagocytic lymphohistiocytosis. Orphanet J Rare Dis 15(1):229
Zhang R, Cui T, He L, Liu M, Hua Z, Wang Z et al (2022) A study on early death prognosis model in adult patients with secondary hemophagocytic lymphohistiocytosis. J Healthc Eng 2022:6704859
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S et al (2007) HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer 48(2):124–131
Fardet L, Galicier L, Lambotte O, Marzac C, Aumont C, Chahwan D et al (2014) Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol 66(9):2613–2620
Graciano AL, Balko JA, Rahn DS, Ahmad N, Giroir BP (2005) The Pediatric Multiple Organ Dysfunction Score (P-MODS): development and validation of an objective scale to measure the severity of multiple organ dysfunction in critically ill children. Crit Care Med 33(7):1484–1491
Leteurtre S, Duhamel A, Salleron J et al (2013) PELOD-2: an update of the PEdiatric logistic organ dysfunction score. Crit Care Med 41(7):1761–1773
Oguz MM, Sahin G, Altinel Acoglu E, Polat E, Yucel H, Oztek Celebi FZ et al (2019) Secondary hemophagocytic lymphohistiocytosis in pediatric patients: a single center experience and factors that influenced patient prognosis. Pediatr Hematol Oncol 36(1):1–16
Wang L, Yang Y, Tan HY, Li S, Feng Y (2020) Protective actions of acidic hydrolysates of polysaccharide extracted from mactra veneriformis against chemical-induced acute liver damage. Front Pharmacol 11:446
Chatterjee S, Dutta RK, Basak P et al (2010) Alteration in marrow stromal microenvironment and apoptosis mechanisms involved in aplastic anemia: an animal model to study the possible disease pathology. Stem Cells Int 2010:932354
Wang S, Lv K, Zhou Y et al (2023) A novel prognosis-prediction model based on coagulation indicators in secondary hemophagocytic lymphohistiocytosis. Ann Hematol 102(11):3251–3259
Tang WP, Zhong N, Chen ZW, Kong FC, Wei YL, Li F (2019) Clinical characteristics of liver dysfunction in patients with hemophagocytic syndrome. Zhongguo Shi Yan Xue Ye Xue Za Zhi 27:1297–1304
Li X, Yan H, Luo T et al (2022) Fulfillment status of hypertriglyceridemia and hypofibrinogenemia in children with hemophagocytic lymphohistiocytosis and risks of multiple organ dysfunction syndrome and early mortality. Orphanet J Rare Dis 17(1):161
Si SJ, Tasian SK, Bassiri H, Fisher BT, Atalla J, Patel R et al (2021) Diagnostic challenges in pediatric hemophagocytic lymphohistiocytosis. J Clin Immunol 41(6):1213–1218
Zoref-Lorenz A, Murakami J, Hofstetter L et al (2022) An improved index for diagnosis and mortality prediction in malignancy-associated hemophagocytic lymphohistiocytosis. Blood 139(7):1098–1110
Cai L, Xing Y, Xia Y et al (2023) Comparative study of biomarkers for the early identification of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in infectious mononucleosis. BMC Infect Dis 23(1):728
Lu X, Wei A, Yang X, Liu J, Li S, Kan Y et al (2021) The role of Pre-therapeutic (18)F-FDG PET/CT in pediatric hemophagocytic lymphohistiocytosis with epstein-barr virus infection. Front Med (Lausanne) 8:836438
Bordbar M, Sanaei Dashti A, Amanati A, Shorafa E, Mansoori Y, Dehghani SJ et al (2021) Assessment of the HScore as a predictor of disease outcome in patients with COVID-19. BMC Pulm Med 21(1):338
Acknowledgements
The authors would like to thank every colleague in Hunan Provincial Key Laboratory of Pediatric Emergency Medicine for their assistance.
Funding
This study was supported by the Hunan Provincial Natural Science Foundation of China (2023JJ30324, grant to XLu), the Hunan Provincial Science and Technology Department Project (2020SK1014-3, and 2020SK2114, grant to XLu), the Hunan Provincial Key Laboratory of Emergency Medicine for Children (No. 2018TP1028, grant to ZX), the National Natural Science Foundation of China (Young Scientists Fund, No. 82102285, grant to XLi), and the Hunan Provincial Health Commission Project (2020SK50509, grant to DZ). The study sponsors have no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
ZT contributed to the study’s conception, analyzed and interpreted the data, and wrote the manuscript. DZ, XL, HY, TL, LX, and YY contributed to the study design, interpreted the data, and revised the manuscript. MT, XJ, JH, XZ, LZ, YL and ZX interpreted the data, and revised the manuscript. XLu designed the study, interpreted the data, and revised the manuscript. All authors read and approved the final manuscript. The corresponding author (XLu) had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics statement
The study protocol was reviewed and approved by the Medical Ethics Committee of the Hunan Children's Hospital (HCHLL-2022–123) and The First People's Hospital of Chenzhou (2023140).
Consent to participate
Informed consent was waved by the Medical Ethics Committee of the Hunan Children's Hospital because of the retrospective design. The authors had no access to information that could identify individual participants during and after data collection.
Consent to publish
Not applicable.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, Z., Zhu, D., Li, X. et al. Development and validation of an early mortality risk model for pediatric hemophagocytic lymphohistiocytosis: a comparison with HScore, PELOD-2, P-MODS, and pSOFA. Ann Hematol (2024). https://doi.org/10.1007/s00277-024-05780-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00277-024-05780-2